Back
Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes I: Pre- and Early Disease (0530–0535)
0535: Increase Rates of Bacterial Infection in Patients with 'Pre-RA'
Saturday, November 12, 2022
5:45 PM – 5:55 PM Eastern Time
Location: Ballroom AB
- DP
Duncan Porter, MD
Gartnavel General Hospital
Bearsden, United Kingdom
Presenting Author(s)
Duncan Porter1, Sahil Jain2 and Fraser Morton3, 1Gartnavel General Hospital, Bearsden, United Kingdom, 2Gartnavel General Hospital, Glasgow, Scotland, United Kingdom, 3University of Glasgow, Glasgow, Scotland, United Kingdom
Background/Purpose: In 'pre-RA' there is evidence of disordered immunity manifest by the presence of auto-antibodies, increased concentration of pro-inflammatory cytokines (e.g. TNF) and acute phase reactants (e.g. CRP). It has been postulated that infection occurring in pre-RA may be a risk factor for the development of RA. However, RA is itself associated with an increased rate of infection. The explanation is likely to be multifactorial, relating to RA-associated immune dysfunction, disease activity, comorbidities, treatment, and lifestyle factors (e.g. smoking). The relative contribution of these factors towards the infection rate is unclear.
Methods: The Scottish Early Rheumatoid Arthritis inception cohort recruited 1073 patients with newly diagnosed rheumatoid arthritis (76%) undifferentiated arthritis (24%) from across Scotland, UK. National databases record all community presciptions, hospital admissions, deaths and laboratory samples. Using the date of the first use of methotrexate as the index date, data linkage allows the retrieval of health care data derived from the pre-RA phase in all participants. Five age-sex matched control participants were selcted from the national database for each SERA patient. The prescription of an antibiotic was used as a surrogate for an episiode of community infection. A hospital admission with a main diagnostic code for an infection was used as a surrogate for severe infection. The rate of infections for two years pre- and post-diagnosis were analysed. The ECOSS database includes all positive laboratory microbiology results which allowed characterisation of the microorganisms involved in proven infections.
Results: 809 patients fulfilled the 2010 ACR/EULAR classification criteria for RA and were included in the study, with 3970 matched controls. 308 patients had no episodes of infection; 452 had >1 community infection, and 49 had >1 severe infection. Within the RA population, the risk of infection was associated with higher physical disability, disease activity and anxiety/depression (Table 1). The risk of community infections was stable in the control population (~800/1000 patient.years). In the RA population the rate of community infection rose in the pre-RA phase to ~1200 episodes/1000py in early RA (Figure 1). Very similar results were obtained when the date of diagnosis was used as the index date rather than the date of first methotrextae use. The rate of severe infections was also higher in the 6 months prior to the diagnosis of RA compared to controls. There were 55 positive microbiology cultures in the RA group and 164 in the control group. The relative risk of E Coli (RR 1.78 [1.31, 2.42], p< 0.01) and Haemophilus (RR 2.06 [1.06, 4.01], p=0.03) infections were higher in the RA compared to the control group.
Conclusion: Infections are more common in patients with pre-RA and RA than in age/sex/neighbourhood matched controls. The risk rises >1 year prior to the diagnosis of RA and treatment with methotrexate, and then remains stable in the first two years of the disease. Infection may hasten the progression through the pre-RA phases. Alternatively, disease assocaited immune dysfunction in pre-RA may predispose to infection.
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291921-1-ANY(1).jpg width=440 height=249.885783718104 border=0 style=border-style: none;>
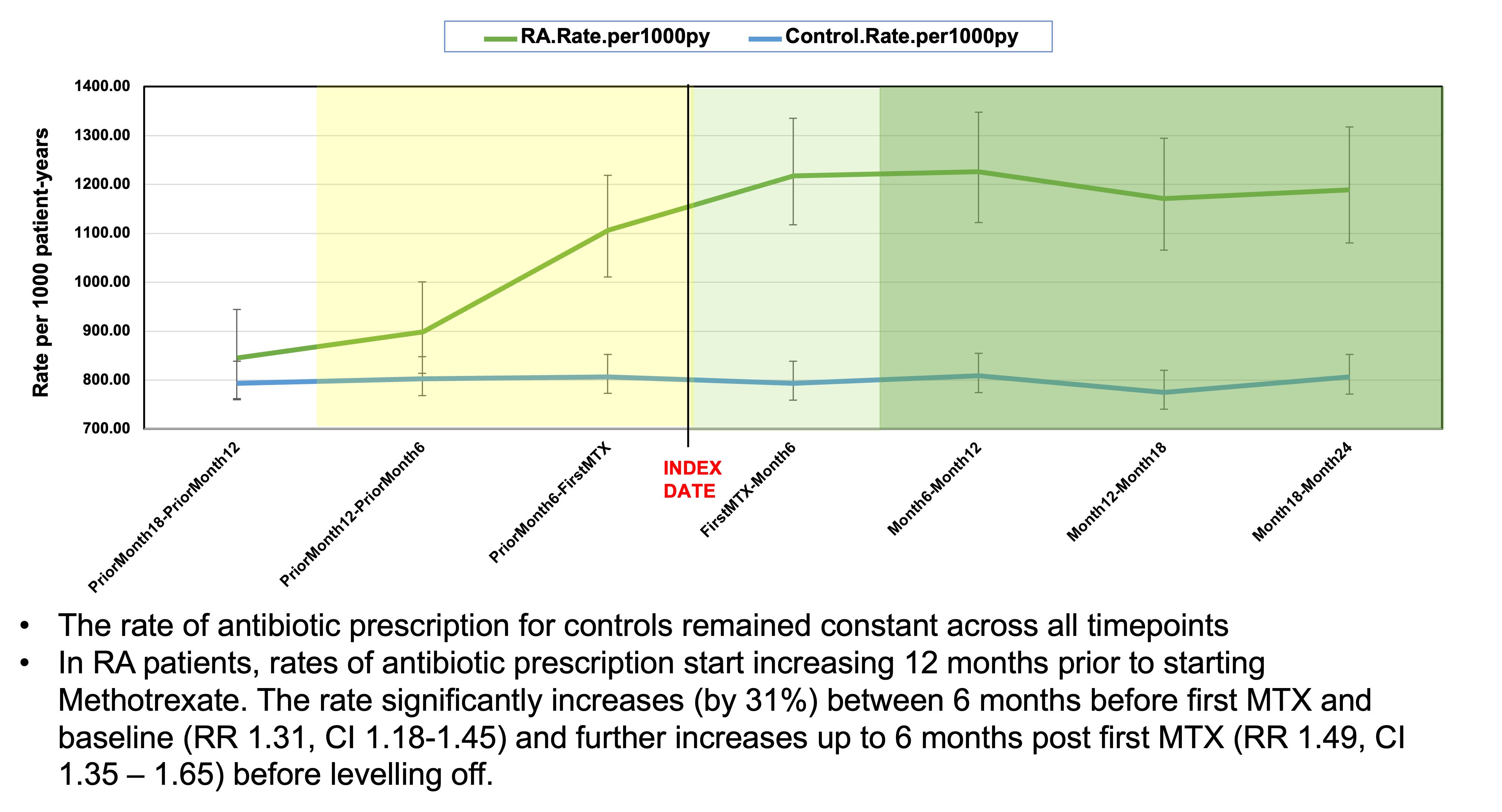 Figure 1 - community infection rates per 1000 patient.years in pre-RA and early RA compared to age/sex/neighbourhood matched controls
Figure 1 - community infection rates per 1000 patient.years in pre-RA and early RA compared to age/sex/neighbourhood matched controls
Disclosures: D. Porter, None; S. Jain, None; F. Morton, None.
Background/Purpose: In 'pre-RA' there is evidence of disordered immunity manifest by the presence of auto-antibodies, increased concentration of pro-inflammatory cytokines (e.g. TNF) and acute phase reactants (e.g. CRP). It has been postulated that infection occurring in pre-RA may be a risk factor for the development of RA. However, RA is itself associated with an increased rate of infection. The explanation is likely to be multifactorial, relating to RA-associated immune dysfunction, disease activity, comorbidities, treatment, and lifestyle factors (e.g. smoking). The relative contribution of these factors towards the infection rate is unclear.
Methods: The Scottish Early Rheumatoid Arthritis inception cohort recruited 1073 patients with newly diagnosed rheumatoid arthritis (76%) undifferentiated arthritis (24%) from across Scotland, UK. National databases record all community presciptions, hospital admissions, deaths and laboratory samples. Using the date of the first use of methotrexate as the index date, data linkage allows the retrieval of health care data derived from the pre-RA phase in all participants. Five age-sex matched control participants were selcted from the national database for each SERA patient. The prescription of an antibiotic was used as a surrogate for an episiode of community infection. A hospital admission with a main diagnostic code for an infection was used as a surrogate for severe infection. The rate of infections for two years pre- and post-diagnosis were analysed. The ECOSS database includes all positive laboratory microbiology results which allowed characterisation of the microorganisms involved in proven infections.
Results: 809 patients fulfilled the 2010 ACR/EULAR classification criteria for RA and were included in the study, with 3970 matched controls. 308 patients had no episodes of infection; 452 had >1 community infection, and 49 had >1 severe infection. Within the RA population, the risk of infection was associated with higher physical disability, disease activity and anxiety/depression (Table 1). The risk of community infections was stable in the control population (~800/1000 patient.years). In the RA population the rate of community infection rose in the pre-RA phase to ~1200 episodes/1000py in early RA (Figure 1). Very similar results were obtained when the date of diagnosis was used as the index date rather than the date of first methotrextae use. The rate of severe infections was also higher in the 6 months prior to the diagnosis of RA compared to controls. There were 55 positive microbiology cultures in the RA group and 164 in the control group. The relative risk of E Coli (RR 1.78 [1.31, 2.42], p< 0.01) and Haemophilus (RR 2.06 [1.06, 4.01], p=0.03) infections were higher in the RA compared to the control group.
Conclusion: Infections are more common in patients with pre-RA and RA than in age/sex/neighbourhood matched controls. The risk rises >1 year prior to the diagnosis of RA and treatment with methotrexate, and then remains stable in the first two years of the disease. Infection may hasten the progression through the pre-RA phases. Alternatively, disease assocaited immune dysfunction in pre-RA may predispose to infection.
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1291921-1-ANY(1).jpg width=440 height=249.885783718104 border=0 style=border-style: none;>
Table 1 - characteristics of RA patients with no infection, >1 community infection and >1 severe infection
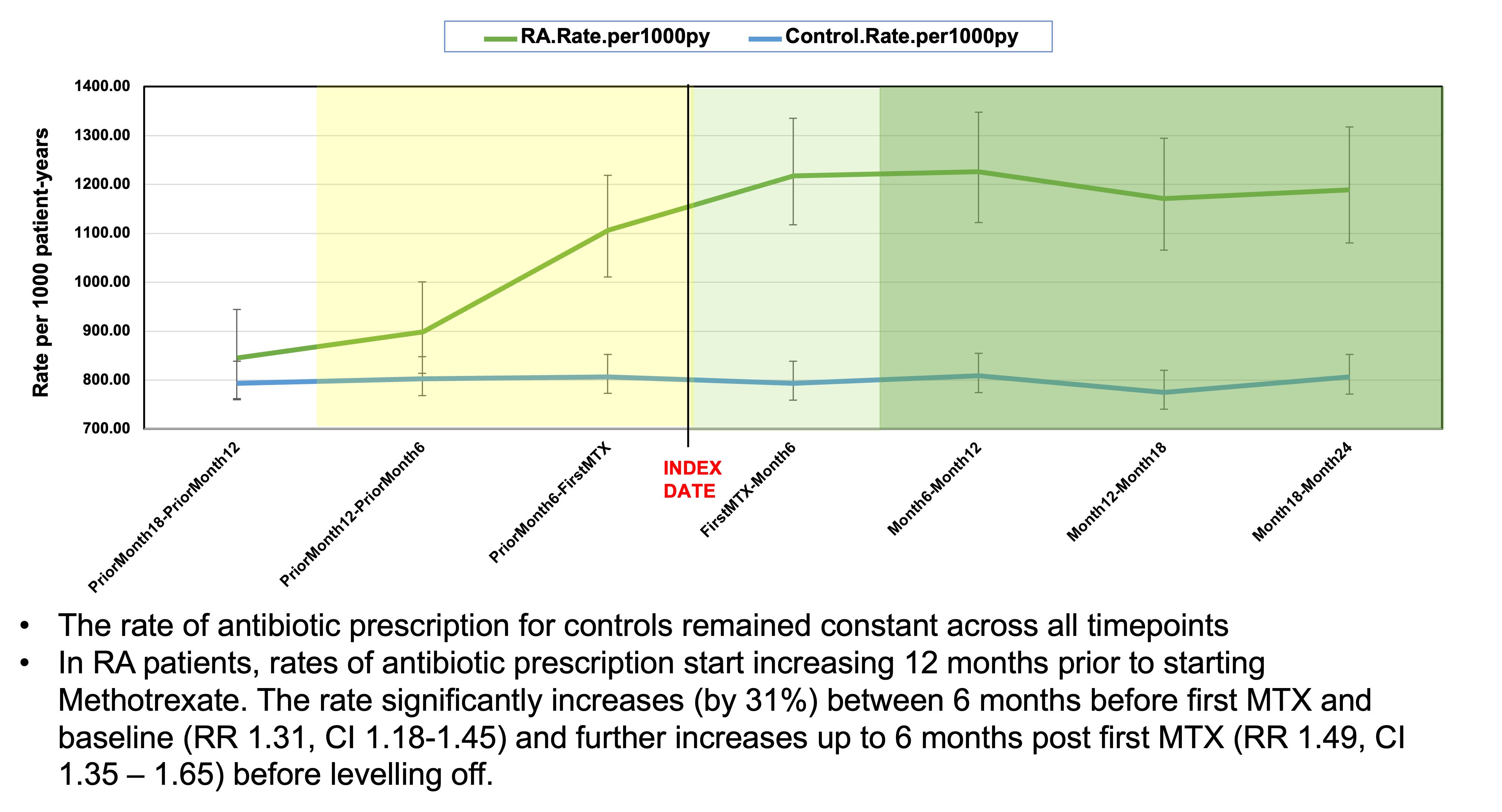 Figure 1 - community infection rates per 1000 patient.years in pre-RA and early RA compared to age/sex/neighbourhood matched controls
Figure 1 - community infection rates per 1000 patient.years in pre-RA and early RA compared to age/sex/neighbourhood matched controlsDisclosures: D. Porter, None; S. Jain, None; F. Morton, None.

