Back
Poster Session D
Crystal arthropathies
Session: (1787–1829) Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
1813: Patient-Reported Outcomes in CPPD Compared to Gout and Osteoarthritis
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MW
Mary Whelan, BS
Brigham and Women's Hospital
Boston, MA, United States
Abstract Poster Presenter(s)
Mary Grace Whelan1, Keigo Hayashi2 and Sara Tedeschi1, 1Brigham and Women's Hospital, Boston, MA, 2Brigham and Women's Hospital, Okayama, Japan
Background/Purpose: Calcium pyrophosphate deposition (CPPD) disease prevalence is similar to gout and osteoarthritis (OA), yet CPPD outcomes research greatly lags behind these other forms of arthritis. We compared validated patient-reported outcome measures in a prospective single center CPPD registry versus clinic-based gout and OA cohorts from the literature.
Methods: Potential CPPD registry participants were identified using electronic health record (EHR) data from a single academic medical center, Feb-May 2022. Presence of 1 or more CPPD manifestation (acute calcium pyrophosphate [CPP] crystal arthritis, OA with CPPD, and chronic CPP inflammatory arthritis) was assessed by manual EHR review and surveys. Baseline surveys included the Gout Assessment Questionnaire (GAQ 2.0) modified to ask about "pseudogout" rather than "gout" (range 0-100), RAPID3 (range 0-30), and WOMAC (ranges: pain, 5-25; stiffness, 2-10; function, 17-85). We used t-tests to compare responses in the CPPD registry against historical gout and OA controls from cohort studies that reported the same outcome measures.1-3
Results: Among 24 CPPD patients, mean age was 72.8 and 42% were female (Table 1). 19 had at least 1 episode of acute CPP crystal arthritis, 6 had chronic CPP inflammatory arthritis, and 18 had OA with CPPD. CPPD patients had significantly fewer joints involved during a flare (2.4± 2.7) than gout patients (5.2 ± 6.9) (p< 0.01), though pain visual analog scale (range 0-10) scores during a flare were similar in CPPD (6.4 ± 2.1) and gout (6.7 ± 2.6) (p=0.59). CPPD patients reported significantly greater unmet treatment need than gout patients (p< 0.01) (Figure 1). RAPID3 scores in CPPD (8.8 ± 5.0) indicated lower disease activity than in gout (12.1 ±6.2) (p=0.03) and similar disease activity to OA (6.8 ± 6.1) (p=0.20). CPPD patients had significantly worse WOMAC pain and WOMAC stiffness scores than patients with mild OA, and significantly better WOMAC function scores than patients with severe OA (Figure 2).
Conclusion: These preliminary data suggest that patients with CPPD may experience pain comparable to gout and OA, though future studies are needed to validate these outcome measures in CPPD. Patients with CPPD reported substantial unmet treatment needs. Ongoing recruitment to the CPPD registry will contribute further data regarding this common yet understudied arthritis.
References
1. Hirsch JD, et al. Patient Relat Outcome Meas 2010.
2. Castrejón I, et al. Arthritis Care Res 2013.
3. Woo J, et al. J Rheum 2004.
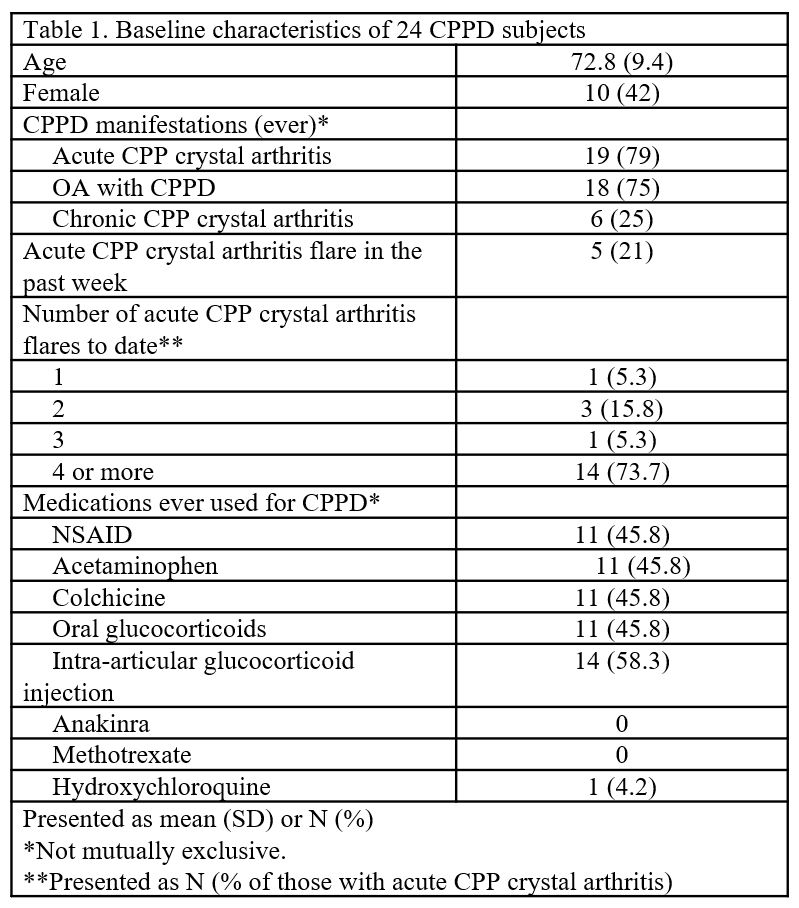 Table 1. Baseline Characteristics of 24 CPPD Subjects
Table 1. Baseline Characteristics of 24 CPPD Subjects
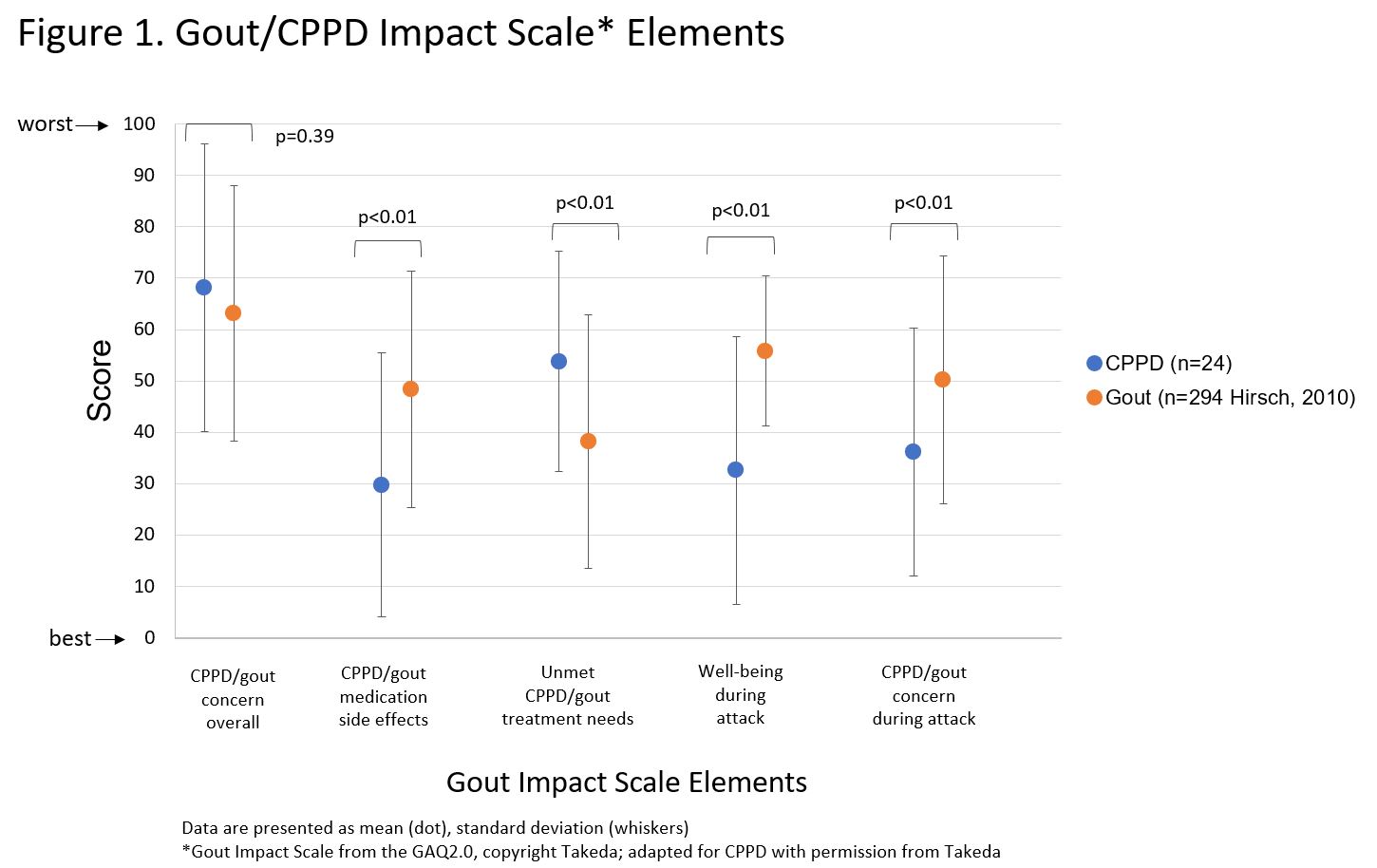 Figure 1. Gout/CPPD Impact Scale* Elements
Figure 1. Gout/CPPD Impact Scale* Elements
Data are presented as mean (dot), standard deviation (whiskers)
*Gout Impact Scale from the GAQ2.0, copyright Takeda; adapted for CPPD with permission from Takeda
.jpg) Figure 2. WOMAC Subscales for CPPD, Mild OA, and Severe OA
Figure 2. WOMAC Subscales for CPPD, Mild OA, and Severe OA
Data are presented as mean (dot), standard deviation (whiskers)
Disclosures: M. Whelan, None; K. Hayashi, None; S. Tedeschi, Moderna, NGM Biopharmaceuticals.
Background/Purpose: Calcium pyrophosphate deposition (CPPD) disease prevalence is similar to gout and osteoarthritis (OA), yet CPPD outcomes research greatly lags behind these other forms of arthritis. We compared validated patient-reported outcome measures in a prospective single center CPPD registry versus clinic-based gout and OA cohorts from the literature.
Methods: Potential CPPD registry participants were identified using electronic health record (EHR) data from a single academic medical center, Feb-May 2022. Presence of 1 or more CPPD manifestation (acute calcium pyrophosphate [CPP] crystal arthritis, OA with CPPD, and chronic CPP inflammatory arthritis) was assessed by manual EHR review and surveys. Baseline surveys included the Gout Assessment Questionnaire (GAQ 2.0) modified to ask about "pseudogout" rather than "gout" (range 0-100), RAPID3 (range 0-30), and WOMAC (ranges: pain, 5-25; stiffness, 2-10; function, 17-85). We used t-tests to compare responses in the CPPD registry against historical gout and OA controls from cohort studies that reported the same outcome measures.1-3
Results: Among 24 CPPD patients, mean age was 72.8 and 42% were female (Table 1). 19 had at least 1 episode of acute CPP crystal arthritis, 6 had chronic CPP inflammatory arthritis, and 18 had OA with CPPD. CPPD patients had significantly fewer joints involved during a flare (2.4± 2.7) than gout patients (5.2 ± 6.9) (p< 0.01), though pain visual analog scale (range 0-10) scores during a flare were similar in CPPD (6.4 ± 2.1) and gout (6.7 ± 2.6) (p=0.59). CPPD patients reported significantly greater unmet treatment need than gout patients (p< 0.01) (Figure 1). RAPID3 scores in CPPD (8.8 ± 5.0) indicated lower disease activity than in gout (12.1 ±6.2) (p=0.03) and similar disease activity to OA (6.8 ± 6.1) (p=0.20). CPPD patients had significantly worse WOMAC pain and WOMAC stiffness scores than patients with mild OA, and significantly better WOMAC function scores than patients with severe OA (Figure 2).
Conclusion: These preliminary data suggest that patients with CPPD may experience pain comparable to gout and OA, though future studies are needed to validate these outcome measures in CPPD. Patients with CPPD reported substantial unmet treatment needs. Ongoing recruitment to the CPPD registry will contribute further data regarding this common yet understudied arthritis.
References
1. Hirsch JD, et al. Patient Relat Outcome Meas 2010.
2. Castrejón I, et al. Arthritis Care Res 2013.
3. Woo J, et al. J Rheum 2004.
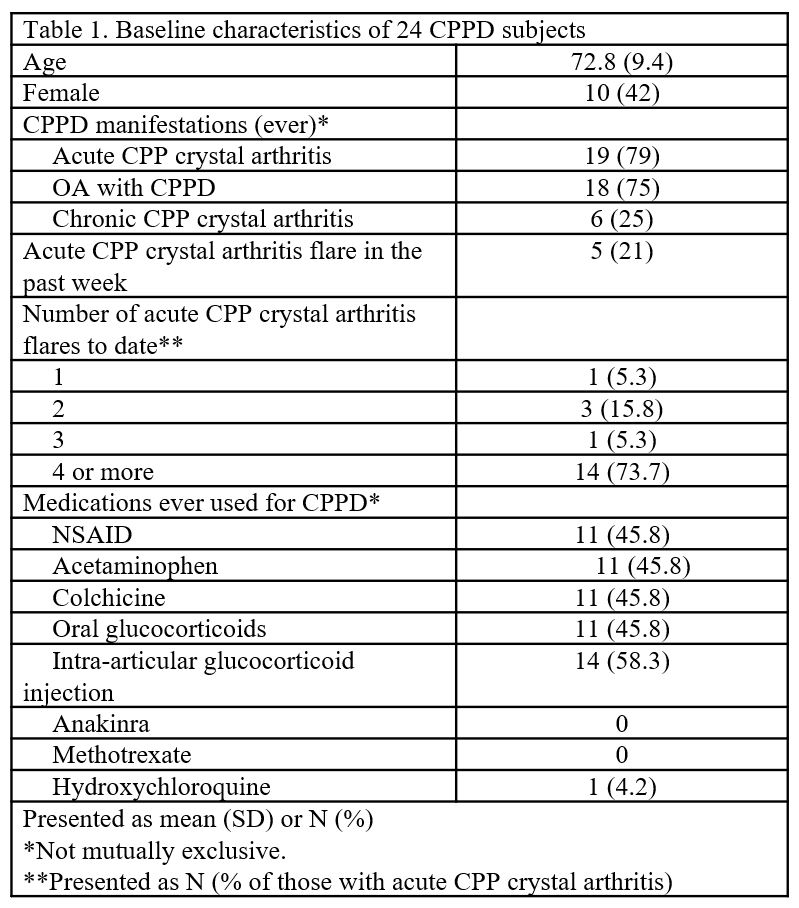 Table 1. Baseline Characteristics of 24 CPPD Subjects
Table 1. Baseline Characteristics of 24 CPPD Subjects 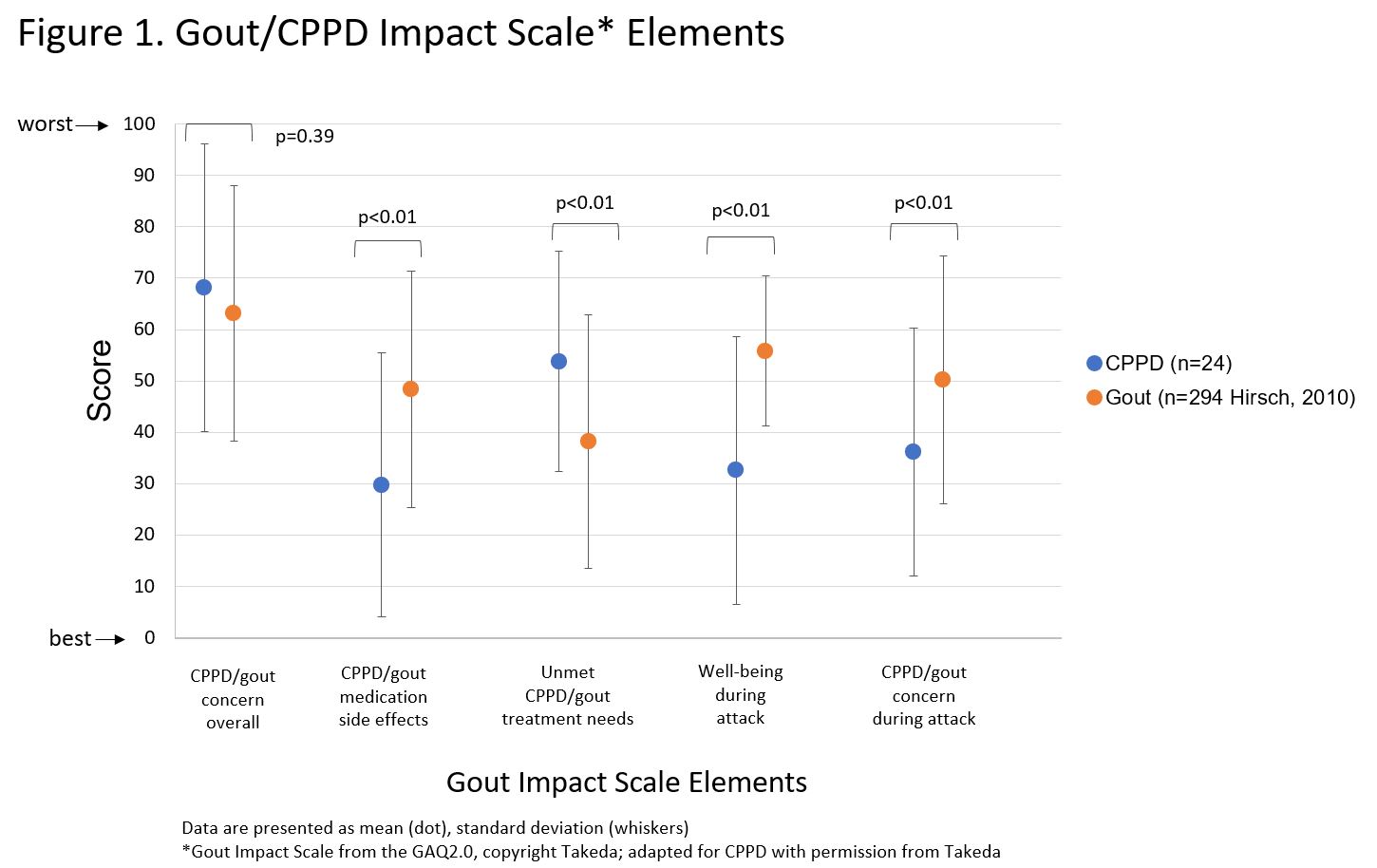 Figure 1. Gout/CPPD Impact Scale* Elements
Figure 1. Gout/CPPD Impact Scale* ElementsData are presented as mean (dot), standard deviation (whiskers)
*Gout Impact Scale from the GAQ2.0, copyright Takeda; adapted for CPPD with permission from Takeda
.jpg) Figure 2. WOMAC Subscales for CPPD, Mild OA, and Severe OA
Figure 2. WOMAC Subscales for CPPD, Mild OA, and Severe OAData are presented as mean (dot), standard deviation (whiskers)
Disclosures: M. Whelan, None; K. Hayashi, None; S. Tedeschi, Moderna, NGM Biopharmaceuticals.

