Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0681: Antiphospholipid Antibodies and Incident Cardiovascular Events in a Diverse Population: Results from the Dallas Heart Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- YZ
Yu (Ray) Zuo, MD, MS
University of Michigan
Ann Arbor, MI, United States
Abstract Poster Presenter(s)
Yu (Ray) Zuo1, Sherwin Navaz1, Wenying Liang1, Chun Li2, Colby Ayers3, Christine Rysenga1, Alyssa Harbaugh1, Gary Norman4, Elizabeth Solow3, Dami Akinmolayemi5, Anand Rohatgi3, David Karp6, Jason S Knight7 and James de Lemos3, 1University of Michigan, Ann Arbor, MI, 2People's Hospital Peking University, Beijing, China, 3UT Southwestern Medical Center, Dallas, TX, 4Werfen, San Diego, 5Columbia University, New York, NY, 6UT Southwestern, Dallas, TX, 7University of Michigan, Division of Rheumatology, Ann Arbor, MI
Background/Purpose: While circulating antiphospholipid antibodies (aPL) are recognized as an important acquired risk factor for thrombotic events, the prevalence of aPL in the general population remains mostly unknown. The Dallas Heart Study (DHS) is a prospective longitudinal population study that has been underway since 1999. The goal of our study was to determine the population prevalence of aPL and their association with future atherosclerotic cardiovascular disease (ASCVD) events in a large racially and ethnically diverse population. Moreover, we sought to provide potential mechanistic insights into the role of aPL in ASCVD.
Methods: We measured eight aPL species [anticardiolipin (aCL) IgG/IgM/IgA, anti-beta-2 glycoprotein I (aβ2GPI) IgG/IgM/IgA, and anti-phosphatidylserine/prothrombin (aPS/PT) IgG/IgM] (Werfen Quanta Lite®) in plasma collected from 2,427 participants during phase 2 of the DHS from 2007 to 2009. All participants were free of ASCVD at the time of blood collection and had no self-reported autoimmune disease requiring immunosuppressive medication. Median follow-up after plasma collection was eight years. Associations with future ASCVD events (defined as first nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or death from a cardiovascular cause) were assessed by Cox proportional hazards models, adjusted for known cardiovascular disease risk factors.
Results: The prevalence of any aPL was 15% in the DHS population, with approximately one-third of those being detected at a moderate or high titer; aCL IgM had the highest prevalence (6.4%), followed by aPS/PT IgM (3.4%), aβ2GPI IgM (2.6%), and aβ2GPI IgA (2.5%) (Table 1). While aPL were more commonly detected in females, there were no significant differences among racial/ethnic groups. The IgA isotypes of both aCL (hazard ratio (HR) 4.89, 95% confidence interval (CI) 1.52-15.71) and aβ2GPI (HR 2.21, 95% CI 1.02-4.84) were independently associated with future ASCVD events. The risk further increased when applying a more stringent positivity threshold (aCL IgA: HR 9.12, 95% CI 2.85-29.52; aβ2GPI IgA: HR 2.83, 95% CI 1.02-7.86) (Fig 1A-B). Mechanistically, levels of aβ2GPI IgA were negatively correlated with cholesterol efflux capacity (p=0.009) and positively correlated with circulating oxidized LDL (p=0.007). Plasma samples from aβ2GPI IgA-positive individuals were added to early-passage of human coronary artery endothelial cells, and the expression of cell adhesion molecules was determined after 6 hours via an in-cell ELISA platform. As compared with plasma from aβ2GPI IgA-negative individuals, aβ2GPI IgA-positive plasma activated cultured coronary endothelial cells to express surface adhesion molecules (E-selectin, ICAM-1, and VCAM-1) integral to inflammation and thrombosis (Fig 1C-E).
Conclusion: At least one type of aPL was detectable in 15% of adults from the general population. The IgA isotypes of aCL and aβ2GPI were independently associated with future ASCVD events, and aβ2GPI IgA demonstrated in vitro effects consistent with promotion of atherothrombosis. Extended aPL panels may help to identify individuals at risk for ASCVD in the general population.
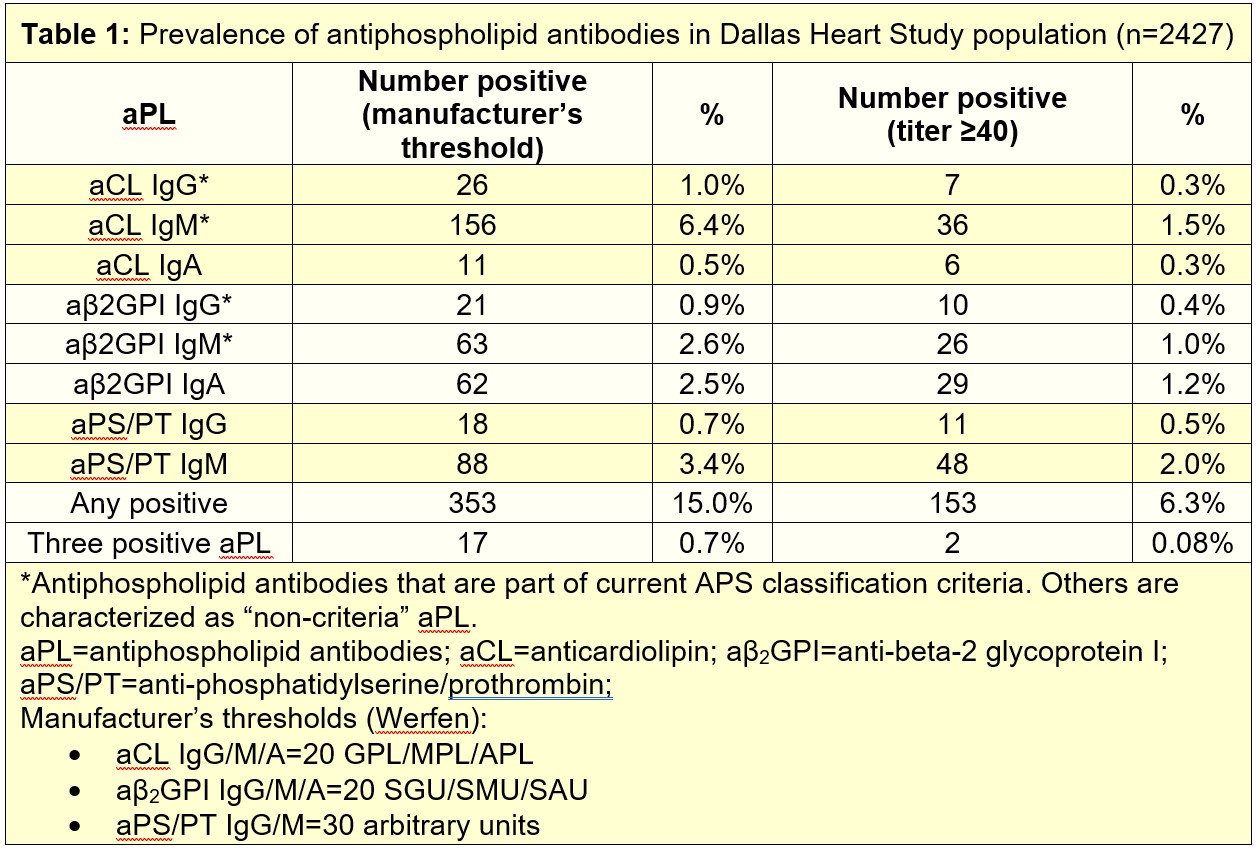
 Figure 1: Association between positive aPL based on either manufacturer’s threshold (A) or ≥40 threshold (B) and future ASCVD events were assessed in Cox proportional hazard models adjusted for known cardiovascular risks including age, ethnicity, smoking history, hypertension, diabetes, and lipid profiles. HR=Hazard ratio; ‡ HR not calculable due to 0 events in aPL group. Human coronary artery endothelial cells were cultured for 6 hours with plasma from either aβ2GPI-positive or -negative DHS2 participants. Cells were then fixed, and surface expression of E-selectin (C), ICAM-1 (D), or VCAM-1 (E) was quantified. Medium, upper and lower quartile, and range are indicated with Box and Whisker plot. Groups were analyzed by Mann-Whitney test; *p < 0.05, **p < 0.01.
Figure 1: Association between positive aPL based on either manufacturer’s threshold (A) or ≥40 threshold (B) and future ASCVD events were assessed in Cox proportional hazard models adjusted for known cardiovascular risks including age, ethnicity, smoking history, hypertension, diabetes, and lipid profiles. HR=Hazard ratio; ‡ HR not calculable due to 0 events in aPL group. Human coronary artery endothelial cells were cultured for 6 hours with plasma from either aβ2GPI-positive or -negative DHS2 participants. Cells were then fixed, and surface expression of E-selectin (C), ICAM-1 (D), or VCAM-1 (E) was quantified. Medium, upper and lower quartile, and range are indicated with Box and Whisker plot. Groups were analyzed by Mann-Whitney test; *p < 0.05, **p < 0.01.
Disclosures: Y. Zuo, None; S. Navaz, None; W. Liang, None; C. Li, None; C. Ayers, None; C. Rysenga, None; A. Harbaugh, None; G. Norman, None; E. Solow, None; D. Akinmolayemi, None; A. Rohatgi, None; D. Karp, None; J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb; J. de Lemos, None.
Background/Purpose: While circulating antiphospholipid antibodies (aPL) are recognized as an important acquired risk factor for thrombotic events, the prevalence of aPL in the general population remains mostly unknown. The Dallas Heart Study (DHS) is a prospective longitudinal population study that has been underway since 1999. The goal of our study was to determine the population prevalence of aPL and their association with future atherosclerotic cardiovascular disease (ASCVD) events in a large racially and ethnically diverse population. Moreover, we sought to provide potential mechanistic insights into the role of aPL in ASCVD.
Methods: We measured eight aPL species [anticardiolipin (aCL) IgG/IgM/IgA, anti-beta-2 glycoprotein I (aβ2GPI) IgG/IgM/IgA, and anti-phosphatidylserine/prothrombin (aPS/PT) IgG/IgM] (Werfen Quanta Lite®) in plasma collected from 2,427 participants during phase 2 of the DHS from 2007 to 2009. All participants were free of ASCVD at the time of blood collection and had no self-reported autoimmune disease requiring immunosuppressive medication. Median follow-up after plasma collection was eight years. Associations with future ASCVD events (defined as first nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or death from a cardiovascular cause) were assessed by Cox proportional hazards models, adjusted for known cardiovascular disease risk factors.
Results: The prevalence of any aPL was 15% in the DHS population, with approximately one-third of those being detected at a moderate or high titer; aCL IgM had the highest prevalence (6.4%), followed by aPS/PT IgM (3.4%), aβ2GPI IgM (2.6%), and aβ2GPI IgA (2.5%) (Table 1). While aPL were more commonly detected in females, there were no significant differences among racial/ethnic groups. The IgA isotypes of both aCL (hazard ratio (HR) 4.89, 95% confidence interval (CI) 1.52-15.71) and aβ2GPI (HR 2.21, 95% CI 1.02-4.84) were independently associated with future ASCVD events. The risk further increased when applying a more stringent positivity threshold (aCL IgA: HR 9.12, 95% CI 2.85-29.52; aβ2GPI IgA: HR 2.83, 95% CI 1.02-7.86) (Fig 1A-B). Mechanistically, levels of aβ2GPI IgA were negatively correlated with cholesterol efflux capacity (p=0.009) and positively correlated with circulating oxidized LDL (p=0.007). Plasma samples from aβ2GPI IgA-positive individuals were added to early-passage of human coronary artery endothelial cells, and the expression of cell adhesion molecules was determined after 6 hours via an in-cell ELISA platform. As compared with plasma from aβ2GPI IgA-negative individuals, aβ2GPI IgA-positive plasma activated cultured coronary endothelial cells to express surface adhesion molecules (E-selectin, ICAM-1, and VCAM-1) integral to inflammation and thrombosis (Fig 1C-E).
Conclusion: At least one type of aPL was detectable in 15% of adults from the general population. The IgA isotypes of aCL and aβ2GPI were independently associated with future ASCVD events, and aβ2GPI IgA demonstrated in vitro effects consistent with promotion of atherothrombosis. Extended aPL panels may help to identify individuals at risk for ASCVD in the general population.
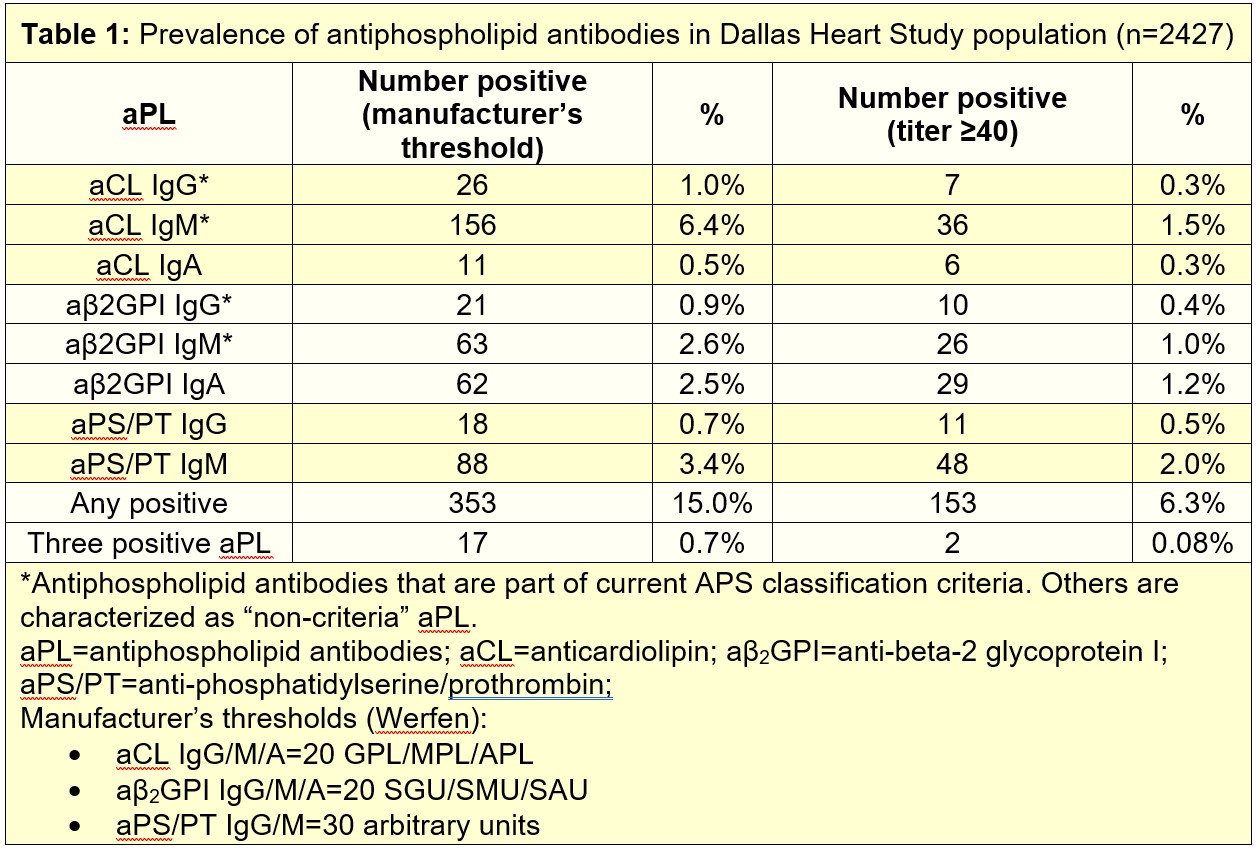
 Figure 1: Association between positive aPL based on either manufacturer’s threshold (A) or ≥40 threshold (B) and future ASCVD events were assessed in Cox proportional hazard models adjusted for known cardiovascular risks including age, ethnicity, smoking history, hypertension, diabetes, and lipid profiles. HR=Hazard ratio; ‡ HR not calculable due to 0 events in aPL group. Human coronary artery endothelial cells were cultured for 6 hours with plasma from either aβ2GPI-positive or -negative DHS2 participants. Cells were then fixed, and surface expression of E-selectin (C), ICAM-1 (D), or VCAM-1 (E) was quantified. Medium, upper and lower quartile, and range are indicated with Box and Whisker plot. Groups were analyzed by Mann-Whitney test; *p < 0.05, **p < 0.01.
Figure 1: Association between positive aPL based on either manufacturer’s threshold (A) or ≥40 threshold (B) and future ASCVD events were assessed in Cox proportional hazard models adjusted for known cardiovascular risks including age, ethnicity, smoking history, hypertension, diabetes, and lipid profiles. HR=Hazard ratio; ‡ HR not calculable due to 0 events in aPL group. Human coronary artery endothelial cells were cultured for 6 hours with plasma from either aβ2GPI-positive or -negative DHS2 participants. Cells were then fixed, and surface expression of E-selectin (C), ICAM-1 (D), or VCAM-1 (E) was quantified. Medium, upper and lower quartile, and range are indicated with Box and Whisker plot. Groups were analyzed by Mann-Whitney test; *p < 0.05, **p < 0.01.Disclosures: Y. Zuo, None; S. Navaz, None; W. Liang, None; C. Li, None; C. Ayers, None; C. Rysenga, None; A. Harbaugh, None; G. Norman, None; E. Solow, None; D. Akinmolayemi, None; A. Rohatgi, None; D. Karp, None; J. Knight, Jazz Pharmaceuticals, Bristol Myers Squibb; J. de Lemos, None.

