Back
Poster Session D
Crystal arthropathies
Session: (1787–1829) Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
1788: Pulmonary Vascular Dysfunction Occurs in Association with Hyperuricaemia: Assessment by a Novel Non-Invasive Measurement of Pulmonary Pulse Wave Transit Time
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- RF
Rachael Flood, MD
Tallaght University Hospital
DUBLIN, Dublin, Ireland
Abstract Poster Presenter(s)
Rachael Flood1, Nicole Fagan2, Diarmuid O'Brien1, Colm Kirby1, David Kane1 and Ronan Mullan1, 1Tallaght University Hospital, Dublin, Ireland, 2St James' Hospital, Dublin, Ireland
Background/Purpose: Hyperuricaemia is common in pulmonary hypertension (PH) occurring in up to 80% of patients with serum uric acid levels(sUA) correlating with poor PH outcomes. sUA through its role in nitric oxide inhibition and endothelial dysfunction has been suggested as a potential mediator of PH. Right heart catheterization (RHC) is the diagnostic gold-standard in PH, however by virtue of its invasive nature other methods are required. Pulmonary Pulse Wave Transit Time (pPTT) is a novel, validated echocardiographic measurement of increased pulmonary vascular tone in PH, defined as the delay between onset of ventricular electrical activity and the arrival of the pulse wave in the pulmonary vein by Doppler echocardiography. pPTT is shortened in PH. Following validation of pPTT in patients with confirmed PH, we assessed pPTT in a gout cohort before and after urate lowering therapy.
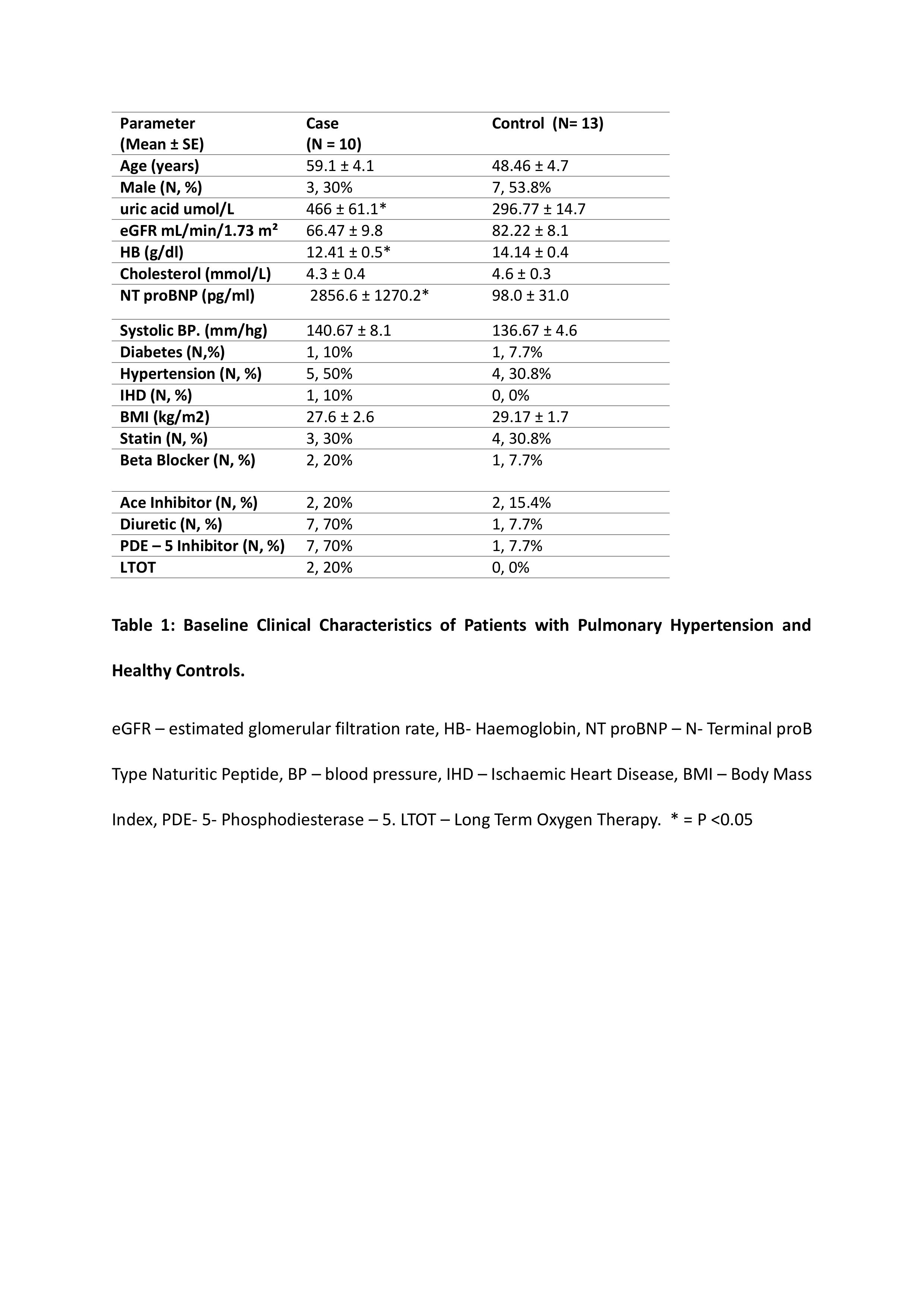
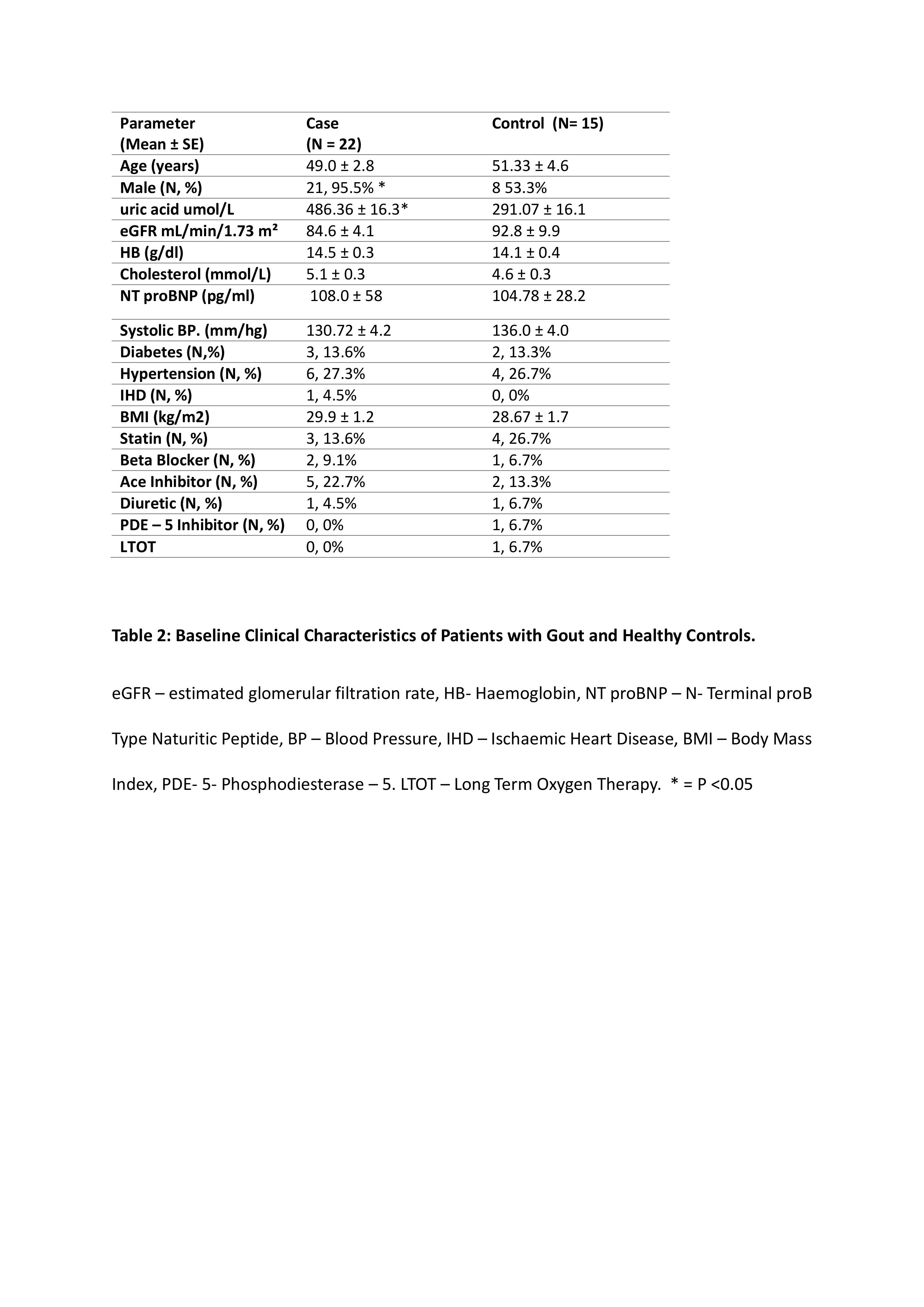
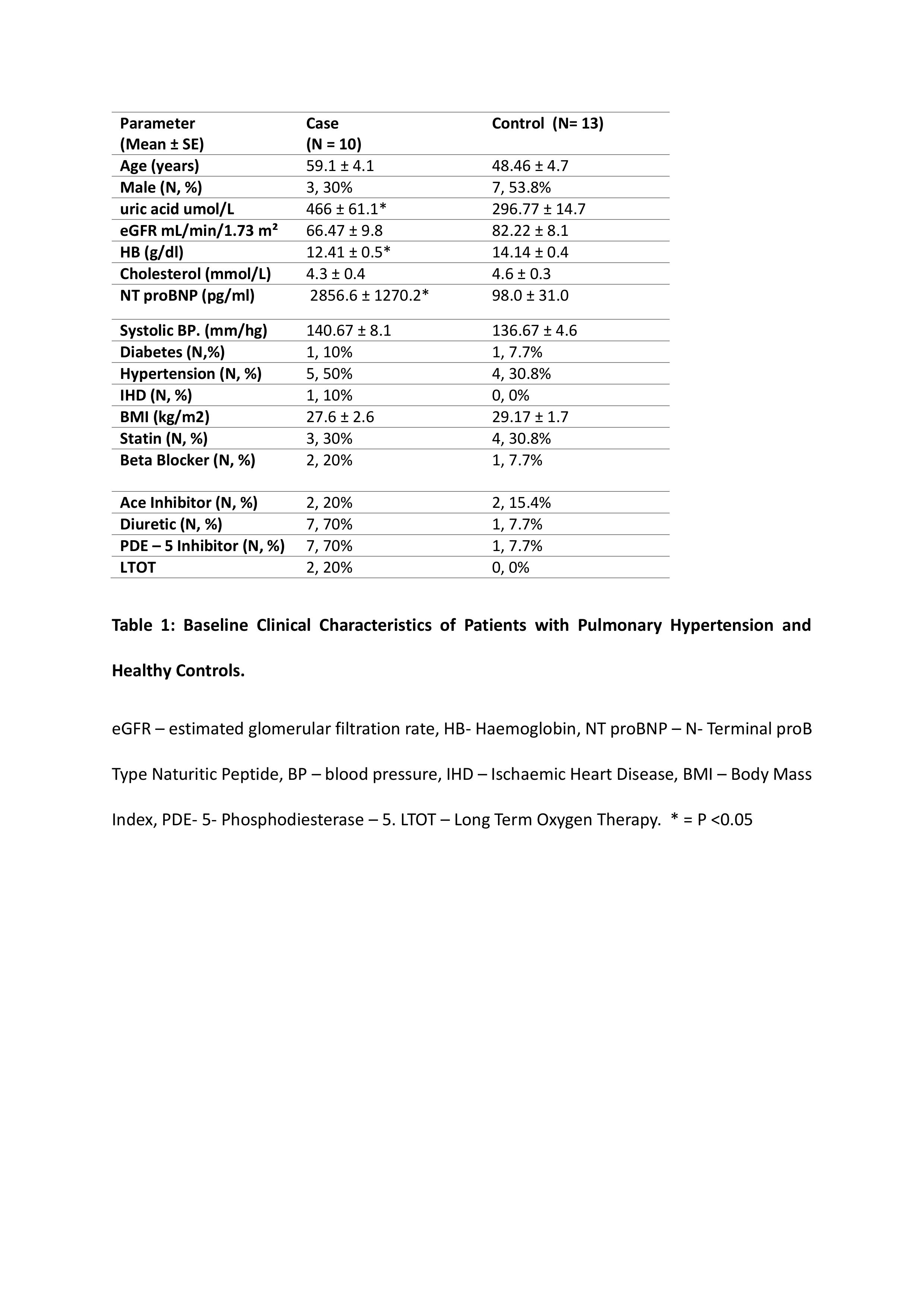
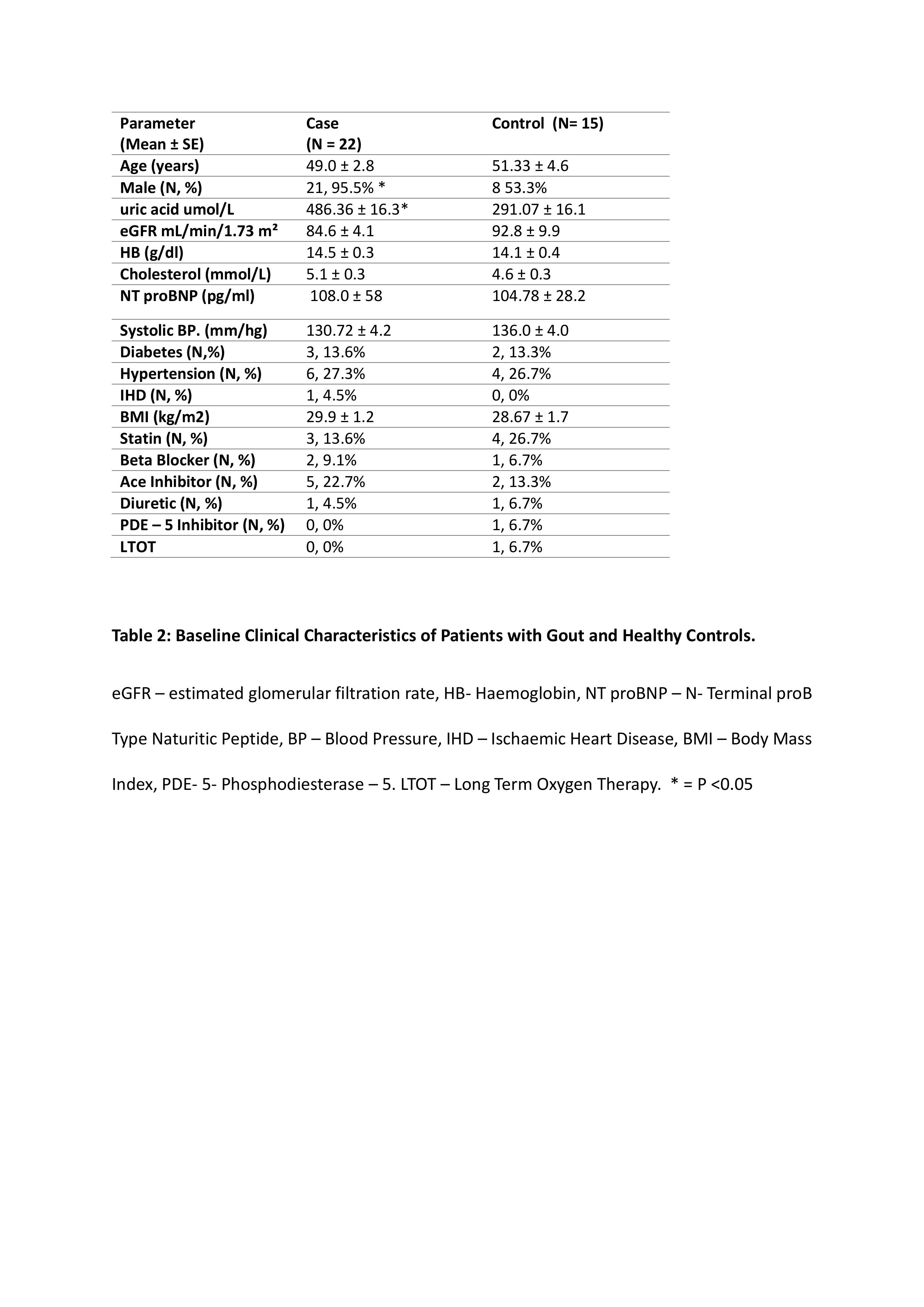
Methods: Patients with PH confirmed at right heart catheterisation versus matched controls were recruited and consented for baseline anthropomorphic assessment and focused echocardiograms. pPTT was calculated as the time interval between the R-wave on the ecg and the corresponding onset of RVOT pulse Doppler flow velocity (R-RVOT) minus the time between the R-wave on the ecg and the corresponding peak late-systolic pulmonary vein flow velocity (R- PVs2) normalized to cardiac cycle length. Treatment naïve hyperuricaemic ( >420umol/L Men. >360umol/L Women.) gout cases vs normouricaemic controls were recruited, with repeat assessments after a 3 month period of sUA within target range following treatment with urate lowering therapy for gout.
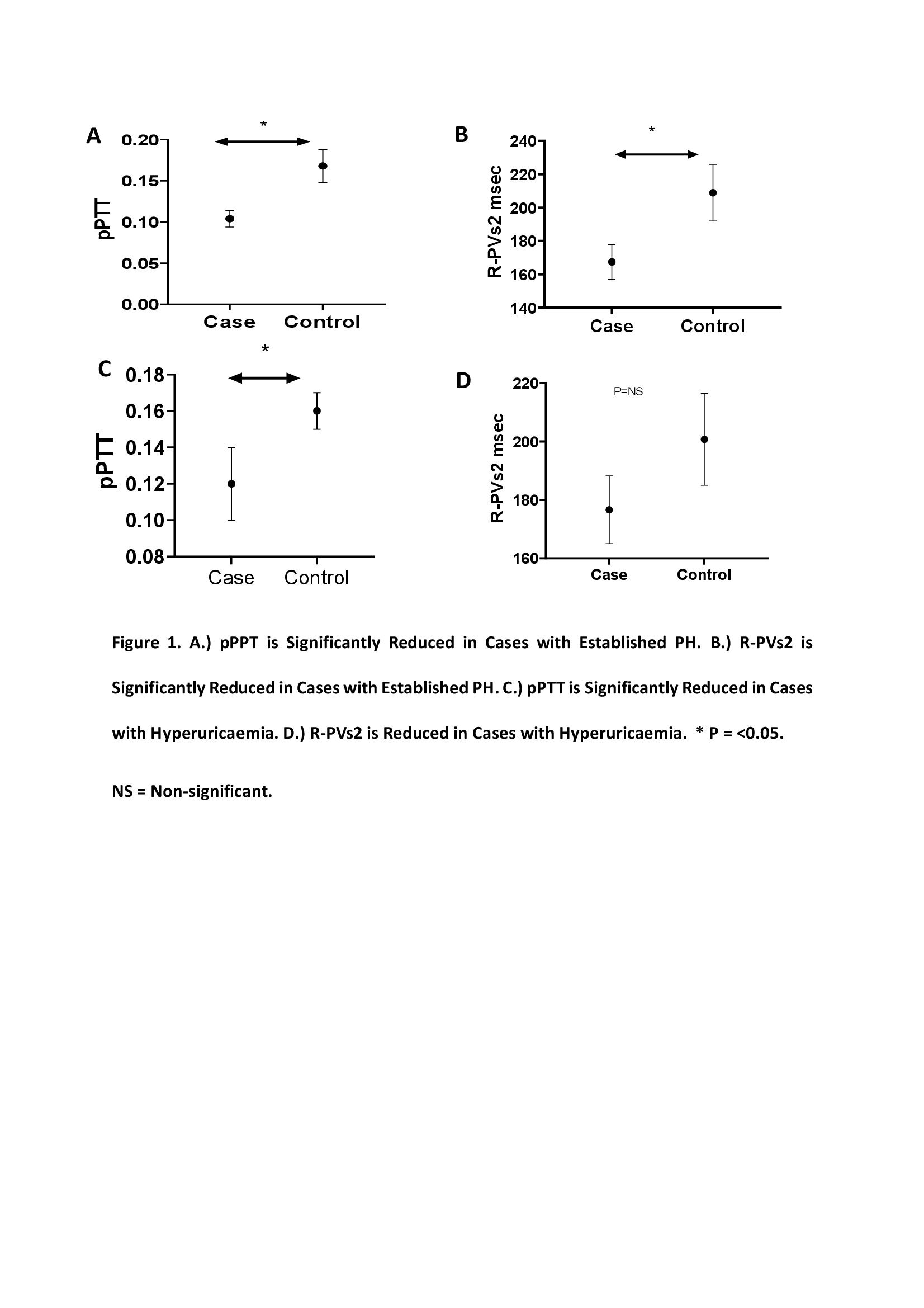
Results: R-PVs2 was reduced in PH cases(mean ± SE)(N=10. 167.40msec ±10.5) versus controls(N=13. 208.95msec ±17.01,P< 0.05.) pPTT was reduced in PH cases (0.104 ±0.01) versus controls (0.168±0.02,P< 0.01). R-PVs2 was reduced in hyperuricaemic gout cases (N= 22 176.63msec ± 11.6) versus controls(N=15 200.75msec ±15.73 P= 0.20) There was a significant reduction in pPTT in hyperuricaemic gout cases (0.12 ± 0.02) versus controls (0.16 ±0.01,P< 0.05.) pPTT was reassessed in 13 cases following a period of 3 months of normal sUA levels. sUA level was reduced (umol/L) between baseline(487.15 ±24.15) and 3 months (309.38 ±20.78 P=< 0.01). There was a non-significant increase in mean R-PVs2 from baseline(159.42ms ±14.37) and three months(168.84ms ±10.94) and non- significant increase in mean pPTT from baseline(0.09 ±0.02) following 3 months(0.12 ±0.02)
Conclusion: pPTT is a novel non invasive method of accessing pulmonary haemodynamics. Patients with hyperuricaemia have shortened pPTT indicative of pulmonary vascular dysfunction.
Disclosures: R. Flood, None; N. Fagan, None; D. O'Brien, None; C. Kirby, None; D. Kane, AbbVie/Abbott; R. Mullan, None.
Background/Purpose: Hyperuricaemia is common in pulmonary hypertension (PH) occurring in up to 80% of patients with serum uric acid levels(sUA) correlating with poor PH outcomes. sUA through its role in nitric oxide inhibition and endothelial dysfunction has been suggested as a potential mediator of PH. Right heart catheterization (RHC) is the diagnostic gold-standard in PH, however by virtue of its invasive nature other methods are required. Pulmonary Pulse Wave Transit Time (pPTT) is a novel, validated echocardiographic measurement of increased pulmonary vascular tone in PH, defined as the delay between onset of ventricular electrical activity and the arrival of the pulse wave in the pulmonary vein by Doppler echocardiography. pPTT is shortened in PH. Following validation of pPTT in patients with confirmed PH, we assessed pPTT in a gout cohort before and after urate lowering therapy.
Methods: Patients with PH confirmed at right heart catheterisation versus matched controls were recruited and consented for baseline anthropomorphic assessment and focused echocardiograms. pPTT was calculated as the time interval between the R-wave on the ecg and the corresponding onset of RVOT pulse Doppler flow velocity (R-RVOT) minus the time between the R-wave on the ecg and the corresponding peak late-systolic pulmonary vein flow velocity (R- PVs2) normalized to cardiac cycle length. Treatment naïve hyperuricaemic ( >420umol/L Men. >360umol/L Women.) gout cases vs normouricaemic controls were recruited, with repeat assessments after a 3 month period of sUA within target range following treatment with urate lowering therapy for gout.
Results: R-PVs2 was reduced in PH cases(mean ± SE)(N=10. 167.40msec ±10.5) versus controls(N=13. 208.95msec ±17.01,P< 0.05.) pPTT was reduced in PH cases (0.104 ±0.01) versus controls (0.168±0.02,P< 0.01). R-PVs2 was reduced in hyperuricaemic gout cases (N= 22 176.63msec ± 11.6) versus controls(N=15 200.75msec ±15.73 P= 0.20) There was a significant reduction in pPTT in hyperuricaemic gout cases (0.12 ± 0.02) versus controls (0.16 ±0.01,P< 0.05.) pPTT was reassessed in 13 cases following a period of 3 months of normal sUA levels. sUA level was reduced (umol/L) between baseline(487.15 ±24.15) and 3 months (309.38 ±20.78 P=< 0.01). There was a non-significant increase in mean R-PVs2 from baseline(159.42ms ±14.37) and three months(168.84ms ±10.94) and non- significant increase in mean pPTT from baseline(0.09 ±0.02) following 3 months(0.12 ±0.02)
Conclusion: pPTT is a novel non invasive method of accessing pulmonary haemodynamics. Patients with hyperuricaemia have shortened pPTT indicative of pulmonary vascular dysfunction.
Disclosures: R. Flood, None; N. Fagan, None; D. O'Brien, None; C. Kirby, None; D. Kane, AbbVie/Abbott; R. Mullan, None.

