Back
Poster Session B
Vasculitis
Session: (1071–1093) Vasculitis – ANCA-Associated Poster II: Treatment Efficacy, Clinical Outcomes, Biomarkers
1086: Characteristics and Outcomes of Patients with ANCA Associated Vasculitis Treated with Plasma Exchange: An Analysis of the National Inpatient Sample Database
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- VG
Vinit Gilvaz, MD
Brown University
East Providence, RI, United States
Abstract Poster Presenter(s)
Vinit Gilvaz1, Akil Sherif2, Sonu Abraham3, Anu Saji2 and Anthony Reginato4, 1Brown University, East Providence, RI, 2Saint Vincent Hospital, Worcester, MA, 3Lahey Medical Center, Burlington, MA, 4Brown University, Providence, RI
Background/Purpose: Plasma exchange (PLEX) has been used in the management of patients with severe anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) for decades. The most recent guidelines set forth by the American College of Rheumatology (ACR) and the Vasculitis Foundation conditionally recommended against the routine use of PLEX in patients with AAV citing the lack of mortality benefit and increased infection risk in this subset of patients. Data from select clinical trials were used to support these guidelines. To our knowledge, there are no studies that have compared outcomes and characteristics of AAV patients treated with and without PLEX using national-level population data.
Methods: Data from 2016 to 2019 was extracted from the NIS (National Inpatient Sample) database. A search was performed using the International Classification of Diseases, Tenth Revision codes (ICD-10) for Granulomatosis with Polyangiitis (GPA) and Microscopic Polyangiitis (MPA). Patients hospitalized with a primary diagnosis of GPA or MPA - with and without an additional ICD 10 PCS (Procedure Coding System) code for PLEX were included in our analysis. Baseline demographics were analyzed. Multivariate logistic and linear regression analysis was used to adjust for confounders. Outcomes of mortality, length of stay (LOS), and costs were compared between the two groups.
Results: We identified 7,280 hospitalizations with a primary diagnosis of AAV. Of these, 935 (12.8 %) were treated with PLEX. Patients in the PLEX group were more likely to have acute kidney injury (78.6% vs. 43.3%) and diffuse alveolar hemorrhage (36.9% vs. 7.7%). Other baseline characteristics (including cardiovascular risk factors) were similar between the two groups. Overall patients treated with PLEX had significantly higher mortality rates (10.7% vs. 2.7%, OR 2.63, P< 0.01, CI: 1.27-5.42), longer average LOS (8.2 days vs 17.0 days, 0R 1.5, P< 0.01, CI:1.03-1.07) and significantly higher average hospital costs (112,439$ vs. 296,891$, OR 1.0, p< 0.01, CI:1-1.0). PLEX was almost exclusively performed in large, urban (100%), academic hospitals (90.3%).
Conclusion: In this large population-based study, PLEX was only used in a minority of patients admitted with AAV (avg. 1 out of 10). However, the overall inpatient mortality of patients treated with PLEX was significantly higher compared to those treated without PLEX. This could potentially be attributed to the selective use of PLEX in patients with more severe disease. However, given these poor outcomes, significantly higher healthcare costs, and longer LOS seen in patients treated with PLEX, our study supports the current recommendations and argues against the routine use of PLEX in patients admitted with AAV.
.jpg)
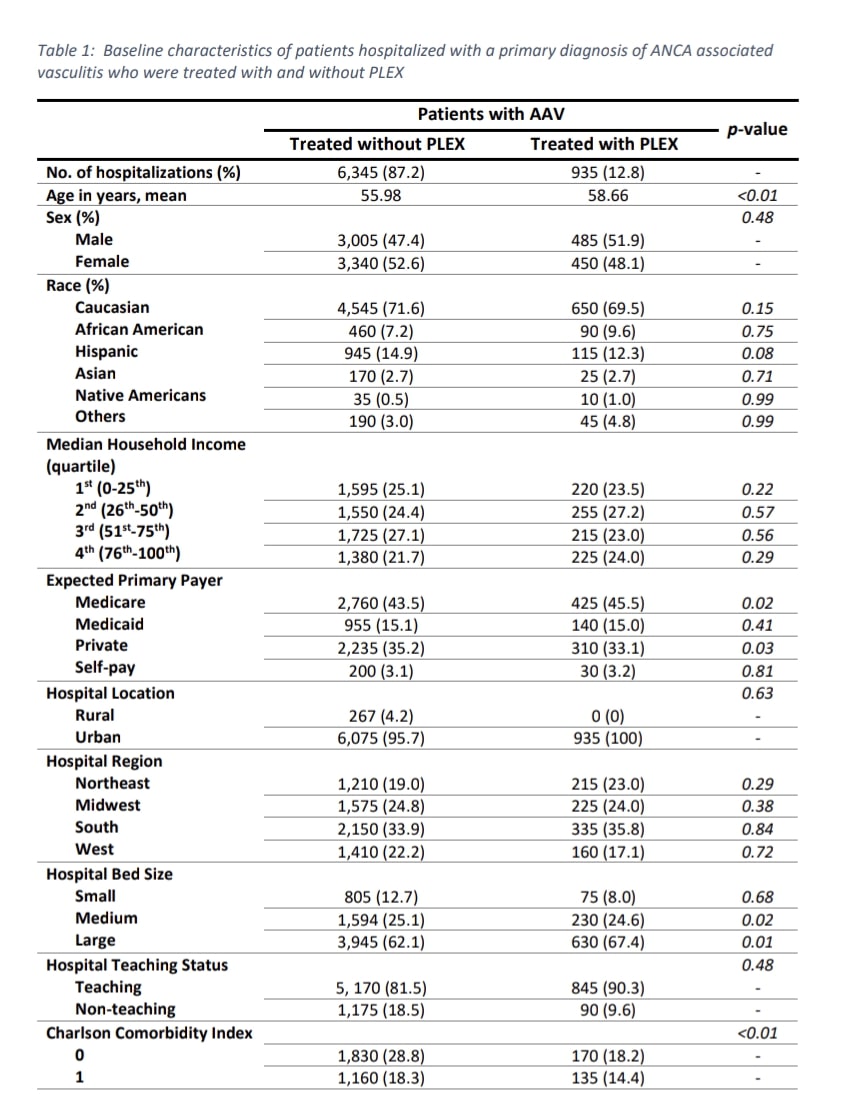 Baseline characteristics
Baseline characteristics
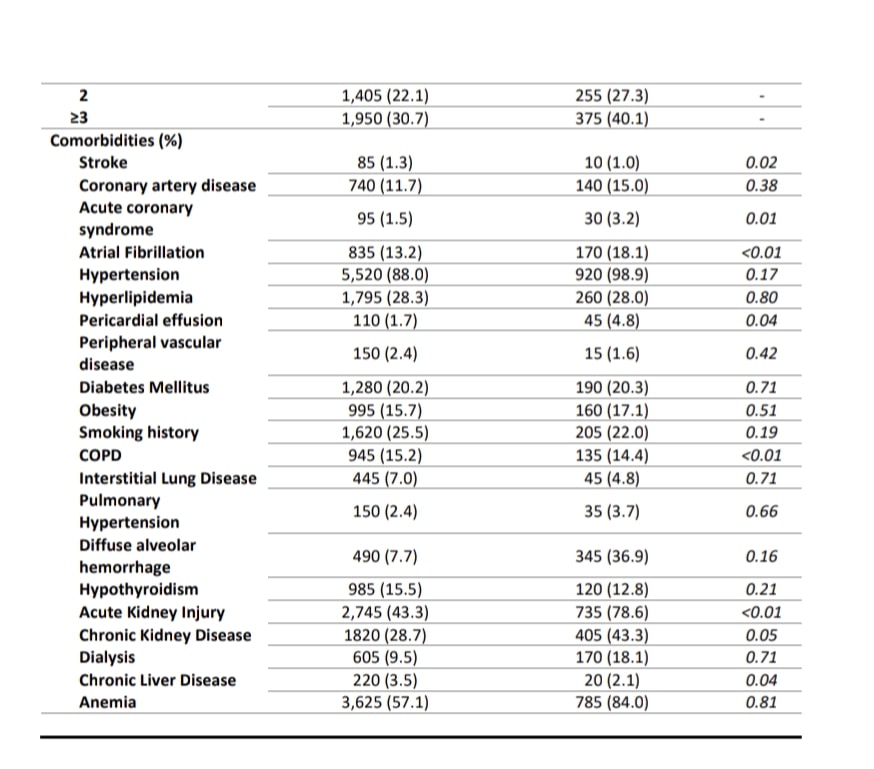 Baseline characteristics
Baseline characteristics
Disclosures: V. Gilvaz, None; A. Sherif, None; S. Abraham, None; A. Saji, None; A. Reginato, None.
Background/Purpose: Plasma exchange (PLEX) has been used in the management of patients with severe anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) for decades. The most recent guidelines set forth by the American College of Rheumatology (ACR) and the Vasculitis Foundation conditionally recommended against the routine use of PLEX in patients with AAV citing the lack of mortality benefit and increased infection risk in this subset of patients. Data from select clinical trials were used to support these guidelines. To our knowledge, there are no studies that have compared outcomes and characteristics of AAV patients treated with and without PLEX using national-level population data.
Methods: Data from 2016 to 2019 was extracted from the NIS (National Inpatient Sample) database. A search was performed using the International Classification of Diseases, Tenth Revision codes (ICD-10) for Granulomatosis with Polyangiitis (GPA) and Microscopic Polyangiitis (MPA). Patients hospitalized with a primary diagnosis of GPA or MPA - with and without an additional ICD 10 PCS (Procedure Coding System) code for PLEX were included in our analysis. Baseline demographics were analyzed. Multivariate logistic and linear regression analysis was used to adjust for confounders. Outcomes of mortality, length of stay (LOS), and costs were compared between the two groups.
Results: We identified 7,280 hospitalizations with a primary diagnosis of AAV. Of these, 935 (12.8 %) were treated with PLEX. Patients in the PLEX group were more likely to have acute kidney injury (78.6% vs. 43.3%) and diffuse alveolar hemorrhage (36.9% vs. 7.7%). Other baseline characteristics (including cardiovascular risk factors) were similar between the two groups. Overall patients treated with PLEX had significantly higher mortality rates (10.7% vs. 2.7%, OR 2.63, P< 0.01, CI: 1.27-5.42), longer average LOS (8.2 days vs 17.0 days, 0R 1.5, P< 0.01, CI:1.03-1.07) and significantly higher average hospital costs (112,439$ vs. 296,891$, OR 1.0, p< 0.01, CI:1-1.0). PLEX was almost exclusively performed in large, urban (100%), academic hospitals (90.3%).
Conclusion: In this large population-based study, PLEX was only used in a minority of patients admitted with AAV (avg. 1 out of 10). However, the overall inpatient mortality of patients treated with PLEX was significantly higher compared to those treated without PLEX. This could potentially be attributed to the selective use of PLEX in patients with more severe disease. However, given these poor outcomes, significantly higher healthcare costs, and longer LOS seen in patients treated with PLEX, our study supports the current recommendations and argues against the routine use of PLEX in patients admitted with AAV.
.jpg)
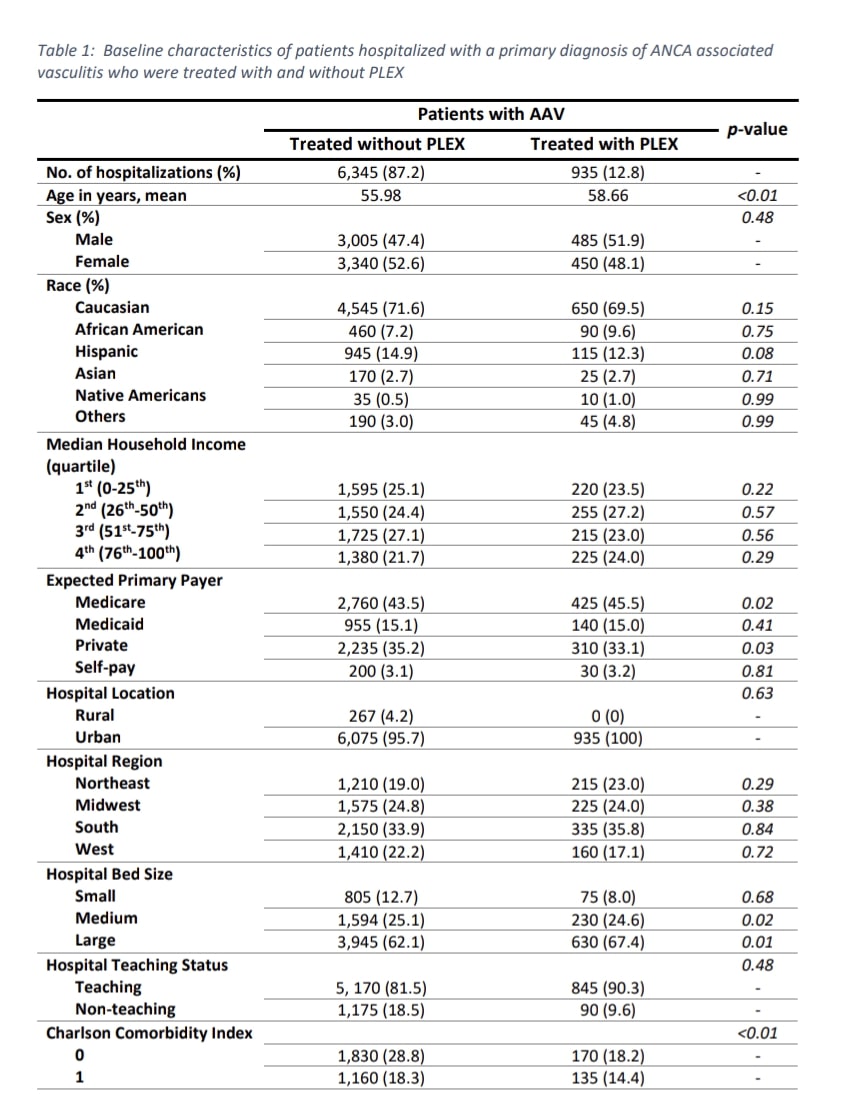 Baseline characteristics
Baseline characteristics 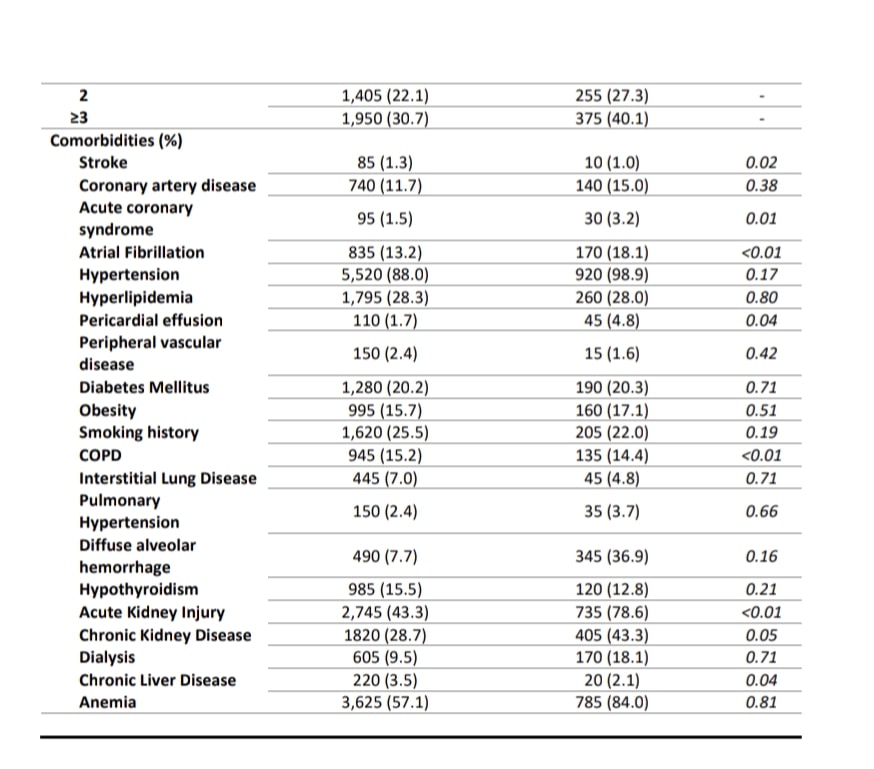 Baseline characteristics
Baseline characteristics Disclosures: V. Gilvaz, None; A. Sherif, None; S. Abraham, None; A. Saji, None; A. Reginato, None.

