Back
Poster Session B
Rheumatoid arthritis (RA)
Session: (0883–0912) RA – Diagnosis, Manifestations, and Outcomes Poster II
0900: Effect of Biologic Agents on Lipid Levels and Cardiovascular Risk in Rheumatoid Arthritis Patients
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- DP
Dimitrios Pappas, MD, MPH
CorEvitas
New York, NY, United States
Abstract Poster Presenter(s)
Dimitrios Pappas1, Jon Giles2, George Reed3, Kevin Kane4, Jeffrey Curtis5 and Joel Kremer6, 1CorEvitas, LLC, Waltham, MA, 2Columbia University, New York, NY, 3The Corrona Research Foundation and University of Massachusetts, Albany, NY, 4University of Massachusetts, Worcester, MA, 5University of Alabama at Birmingham, Hoover, AL, 6The Corrona Research Foundation, Delray Beach, FL
Background/Purpose: Cardiovascular (CV) risk in RA is increased due to interaction between traditional risk factors and systemic inflammation. The purpose of this analysis was to investigate the effect of biologic DMARDs on lipid levels and cardiovascular risk and evaluate whether such effect is associated with changes in CRP and disease activity measures. In addition, we evaluated whether patients with lower LDL levels experience larger increases in LDL which are tracking with disease improvement after initiation of a biologic.
Methods: Patients (pts) with at least moderate disease activity (CDAI >10) initiating a biologic DMARD enrolled in the CERTAIN comparative effectiveness study nested within CorEvitas (formerly known as Corrona) RA registry. Characteristics, including lipid values, and Reynolds Risk Score (RRS) in pts initiating a TNF-α inhibitor (TNFi) or non‐TNFi (rituximab [RTX], abatacept [ABT] or tocilizumab [TCZ]), were measured at baseline prior to biologic initiation and at 3 and 6 months later. Longitudinal mixed models examined the association of individual biologics with changes in lipid levels, and Reynolds Risk Score (RRS). Structural equation models were utilized to model mediation of CRP, CDAI or swollen joint count on lipid changes. Patients who interrupted therapy prior to follow up visits or without complete lipid data were excluded. Change in LDL at 6 months among patients with low LDL at baseline (≤90mg/dl) vs patients in groups with higher levels (90-130 and ≥130mg/dl) were compared. The association between LDL change across baseline LDL groups and disease activity improvement was evaluated.
Results: 1698 initiations of a biologic were analyzed. At baseline 36.8% of pts were biologic naïve and 24.5% on anti-hyperlipidemic therapy. History of prior CVD was present in 7.9% of pts. Pts initiating TCZ had a significant increase in lipid levels but RRS at 3 and 6 months was similar across all biologics (table 1). Mediator analyses were statistically significant regarding the CRP effect (table 2). LDL changes differed depending on baseline LDL but were consistent with estimated changes due to regression to the mean. An association between LDL improvement and CRP change was similar for all baseline LDL groups (table 3).
Conclusion: The impact of lipid changes on CVD risk must be considered in the context of the burden of inflammation in pts with RA. Lipid increases may not necessarily be atherogenic and may occur in the context of the "lipid paradox". In this analysis, moderate increases in lipid levels did not translate to an increased CVD risk as captured by RRS and were partially associated with CRP changes.
 Table 1. Baseline lipid levels, log hsCRP and Reynolds Risk Score and adjusted effect of individual biologics at 3 and 6 months after initiating biologic therapy(a)
Table 1. Baseline lipid levels, log hsCRP and Reynolds Risk Score and adjusted effect of individual biologics at 3 and 6 months after initiating biologic therapy(a)
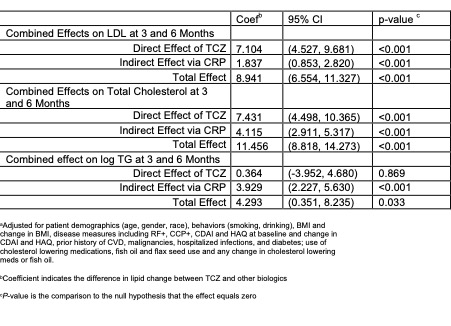 Table 2: Mediator analysis of CRP effect on lipids for TCZ vs other biologics after 3 and 6 months of therapy(a)
Table 2: Mediator analysis of CRP effect on lipids for TCZ vs other biologics after 3 and 6 months of therapy(a)
.jpg) Table 3. LDL evolution in relation to disease activity improvement and associations with CDAI and CRP change(a)
Table 3. LDL evolution in relation to disease activity improvement and associations with CDAI and CRP change(a)
Disclosures: D. Pappas, CorEvitas, Novartis, Sanofi, Genentech, Roche, AbbVie; J. Giles, Pfizer, Eli Lilly, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Novartis, Gilead; G. Reed, CorEvitas, Corrona Research Foundation; K. Kane, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology; J. Kremer, CorEvitas.
Background/Purpose: Cardiovascular (CV) risk in RA is increased due to interaction between traditional risk factors and systemic inflammation. The purpose of this analysis was to investigate the effect of biologic DMARDs on lipid levels and cardiovascular risk and evaluate whether such effect is associated with changes in CRP and disease activity measures. In addition, we evaluated whether patients with lower LDL levels experience larger increases in LDL which are tracking with disease improvement after initiation of a biologic.
Methods: Patients (pts) with at least moderate disease activity (CDAI >10) initiating a biologic DMARD enrolled in the CERTAIN comparative effectiveness study nested within CorEvitas (formerly known as Corrona) RA registry. Characteristics, including lipid values, and Reynolds Risk Score (RRS) in pts initiating a TNF-α inhibitor (TNFi) or non‐TNFi (rituximab [RTX], abatacept [ABT] or tocilizumab [TCZ]), were measured at baseline prior to biologic initiation and at 3 and 6 months later. Longitudinal mixed models examined the association of individual biologics with changes in lipid levels, and Reynolds Risk Score (RRS). Structural equation models were utilized to model mediation of CRP, CDAI or swollen joint count on lipid changes. Patients who interrupted therapy prior to follow up visits or without complete lipid data were excluded. Change in LDL at 6 months among patients with low LDL at baseline (≤90mg/dl) vs patients in groups with higher levels (90-130 and ≥130mg/dl) were compared. The association between LDL change across baseline LDL groups and disease activity improvement was evaluated.
Results: 1698 initiations of a biologic were analyzed. At baseline 36.8% of pts were biologic naïve and 24.5% on anti-hyperlipidemic therapy. History of prior CVD was present in 7.9% of pts. Pts initiating TCZ had a significant increase in lipid levels but RRS at 3 and 6 months was similar across all biologics (table 1). Mediator analyses were statistically significant regarding the CRP effect (table 2). LDL changes differed depending on baseline LDL but were consistent with estimated changes due to regression to the mean. An association between LDL improvement and CRP change was similar for all baseline LDL groups (table 3).
Conclusion: The impact of lipid changes on CVD risk must be considered in the context of the burden of inflammation in pts with RA. Lipid increases may not necessarily be atherogenic and may occur in the context of the "lipid paradox". In this analysis, moderate increases in lipid levels did not translate to an increased CVD risk as captured by RRS and were partially associated with CRP changes.
 Table 1. Baseline lipid levels, log hsCRP and Reynolds Risk Score and adjusted effect of individual biologics at 3 and 6 months after initiating biologic therapy(a)
Table 1. Baseline lipid levels, log hsCRP and Reynolds Risk Score and adjusted effect of individual biologics at 3 and 6 months after initiating biologic therapy(a) 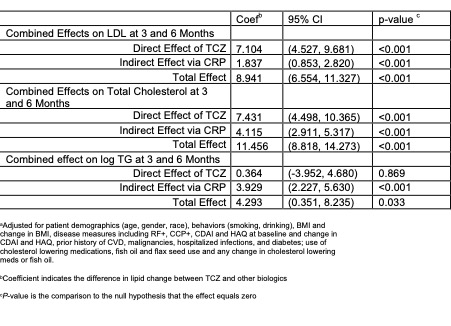 Table 2: Mediator analysis of CRP effect on lipids for TCZ vs other biologics after 3 and 6 months of therapy(a)
Table 2: Mediator analysis of CRP effect on lipids for TCZ vs other biologics after 3 and 6 months of therapy(a).jpg) Table 3. LDL evolution in relation to disease activity improvement and associations with CDAI and CRP change(a)
Table 3. LDL evolution in relation to disease activity improvement and associations with CDAI and CRP change(a)Disclosures: D. Pappas, CorEvitas, Novartis, Sanofi, Genentech, Roche, AbbVie; J. Giles, Pfizer, Eli Lilly, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Novartis, Gilead; G. Reed, CorEvitas, Corrona Research Foundation; K. Kane, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology; J. Kremer, CorEvitas.

