Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0974–1003) SLE – Treatment Poster II
0983: Hydroxychloroquine Use and Heart Failure with Preserved Ejection Fraction in Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- JA
Jake Altier, MD
Medical University of South Carolina
Johns Island, SC, United States
Abstract Poster Presenter(s)
Jake Altier, Fedelis Mutiso, Paul Nietert, Sheldon Litwin and Jim Oates, Medical University of South Carolina, Charleston, SC
Background/Purpose: Initially used as an antimalarial, hydroxychloroquine (HCQ) is standard of care treatment for systemic lupus erythematosus (SLE) and is used as monotherapy or adjunct therapy for rheumatoid arthritis (RA). Long term use of HCQ has been associated with cardiotoxicity that results in conduction abnormalities and cardiomyopathies by disrupting lysosomal activity in cardiac myocytes and inducing a lysosomal storage disease. A hallmark of those with cardiomyopathy secondary to HCQ use is restrictive physiology and diastolic dysfunction, characteristics of heart failure with preserved ejection fraction (HFpEF). We hypothesized that patients with SLE and RA who take HCQ would experience an increased prevalence of HFpEF that has not been previously examined in the literature. This would have clinical implications in long term monitoring of patients on this therapy.
Methods: Patients from the Medical University of South Carolina Research Data Warehouse with at least two diagnosis codes at least 30 days apart for either SLE or RA were identified from January 1st 2015 to March 23rd 2021. Patients were divided into cases who were prescribed HCQ for at least six months prior to assessment and controls who were not prescribed any hydroxychloroquine during the study interval. Patients were assessed for HFPEF diagnosis by diagnosis code. Those patients on < 6 months of HCQ therapy within the interval were excluded from analysis. Propensity matching for covariables known to influence the risk for HFpEF (including gender, obesity, chronic kidney disease, obstructive sleep apnea, hypertension , race, atrial fibrillation, coronary heart disease, and diabetes mellitus) was used to reduce potential bias by HCQ indication. Propensity matched cases and controls were then analyzed for association with HFpEF diagnosis by logistic regression.
Results: There was no statistically significant association between HCQ use and the diagnosis of HFpEF, though there was a trend towards a negative association. Significant associations were not seen within specific co variables and the outcome in this propensity matched case and control group.
Conclusion: These results suggest that HFPEF risk with HCQ does not occur at a population level. This is important to realize given the significant negative association between cardiovascular mortality and HCQ use in SLE (REF). One might hypothesize that cardiac toxicity occurs only in individuals with an underlying genetic risk, such as a risk for lysosomal storage disease. Thus, to study the occurrence of HFPEF with HCQ use at an individual level, pharmacogenomic analysis may also be required. However, these findings do not support the practice withholding clinically indicated HCQ therapy due to a population-level concern for HFPEF as a HCQ-related adverse event.
.jpg) Consort table describing the allocation of patients into their respective groups and subsequent propensity matching. Abbreviations key: MUSC-Medical University of South Carolina, SLE-systemic lupus erythematosus, RA-rheumatoid arthritis, HCQ-hydroxychloroquine.
Consort table describing the allocation of patients into their respective groups and subsequent propensity matching. Abbreviations key: MUSC-Medical University of South Carolina, SLE-systemic lupus erythematosus, RA-rheumatoid arthritis, HCQ-hydroxychloroquine.
.jpg) Distribution of heart failure (outcome) and its risk factors by Hydroxychloroquine (exposure) and patient diagnosis (RA or SLE) in the propensity score matched data set. Matching ratio: RA (1:1) and SLE (2:1). Exact matching by HTN and sex. Abbreviations key: Rheumatoid arthritis1, systemic lupus erythematosus2, hydroxychloroquine3, standard deviation4.
Distribution of heart failure (outcome) and its risk factors by Hydroxychloroquine (exposure) and patient diagnosis (RA or SLE) in the propensity score matched data set. Matching ratio: RA (1:1) and SLE (2:1). Exact matching by HTN and sex. Abbreviations key: Rheumatoid arthritis1, systemic lupus erythematosus2, hydroxychloroquine3, standard deviation4.
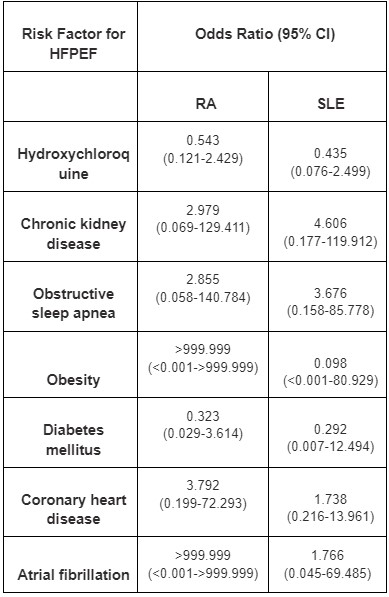 Logistic regression modeling for HFpEF diagnosis among propensity matched RA (left column) and SLE (right column) patients. Hypertension and sex were forced in the propensity matching algorithm and were thus not included in the logistic regression.
Logistic regression modeling for HFpEF diagnosis among propensity matched RA (left column) and SLE (right column) patients. Hypertension and sex were forced in the propensity matching algorithm and were thus not included in the logistic regression.
Disclosures: J. Altier, None; F. Mutiso, None; P. Nietert, None; S. Litwin, None; J. Oates, None.
Background/Purpose: Initially used as an antimalarial, hydroxychloroquine (HCQ) is standard of care treatment for systemic lupus erythematosus (SLE) and is used as monotherapy or adjunct therapy for rheumatoid arthritis (RA). Long term use of HCQ has been associated with cardiotoxicity that results in conduction abnormalities and cardiomyopathies by disrupting lysosomal activity in cardiac myocytes and inducing a lysosomal storage disease. A hallmark of those with cardiomyopathy secondary to HCQ use is restrictive physiology and diastolic dysfunction, characteristics of heart failure with preserved ejection fraction (HFpEF). We hypothesized that patients with SLE and RA who take HCQ would experience an increased prevalence of HFpEF that has not been previously examined in the literature. This would have clinical implications in long term monitoring of patients on this therapy.
Methods: Patients from the Medical University of South Carolina Research Data Warehouse with at least two diagnosis codes at least 30 days apart for either SLE or RA were identified from January 1st 2015 to March 23rd 2021. Patients were divided into cases who were prescribed HCQ for at least six months prior to assessment and controls who were not prescribed any hydroxychloroquine during the study interval. Patients were assessed for HFPEF diagnosis by diagnosis code. Those patients on < 6 months of HCQ therapy within the interval were excluded from analysis. Propensity matching for covariables known to influence the risk for HFpEF (including gender, obesity, chronic kidney disease, obstructive sleep apnea, hypertension , race, atrial fibrillation, coronary heart disease, and diabetes mellitus) was used to reduce potential bias by HCQ indication. Propensity matched cases and controls were then analyzed for association with HFpEF diagnosis by logistic regression.
Results: There was no statistically significant association between HCQ use and the diagnosis of HFpEF, though there was a trend towards a negative association. Significant associations were not seen within specific co variables and the outcome in this propensity matched case and control group.
Conclusion: These results suggest that HFPEF risk with HCQ does not occur at a population level. This is important to realize given the significant negative association between cardiovascular mortality and HCQ use in SLE (REF). One might hypothesize that cardiac toxicity occurs only in individuals with an underlying genetic risk, such as a risk for lysosomal storage disease. Thus, to study the occurrence of HFPEF with HCQ use at an individual level, pharmacogenomic analysis may also be required. However, these findings do not support the practice withholding clinically indicated HCQ therapy due to a population-level concern for HFPEF as a HCQ-related adverse event.
.jpg) Consort table describing the allocation of patients into their respective groups and subsequent propensity matching. Abbreviations key: MUSC-Medical University of South Carolina, SLE-systemic lupus erythematosus, RA-rheumatoid arthritis, HCQ-hydroxychloroquine.
Consort table describing the allocation of patients into their respective groups and subsequent propensity matching. Abbreviations key: MUSC-Medical University of South Carolina, SLE-systemic lupus erythematosus, RA-rheumatoid arthritis, HCQ-hydroxychloroquine. .jpg) Distribution of heart failure (outcome) and its risk factors by Hydroxychloroquine (exposure) and patient diagnosis (RA or SLE) in the propensity score matched data set. Matching ratio: RA (1:1) and SLE (2:1). Exact matching by HTN and sex. Abbreviations key: Rheumatoid arthritis1, systemic lupus erythematosus2, hydroxychloroquine3, standard deviation4.
Distribution of heart failure (outcome) and its risk factors by Hydroxychloroquine (exposure) and patient diagnosis (RA or SLE) in the propensity score matched data set. Matching ratio: RA (1:1) and SLE (2:1). Exact matching by HTN and sex. Abbreviations key: Rheumatoid arthritis1, systemic lupus erythematosus2, hydroxychloroquine3, standard deviation4. 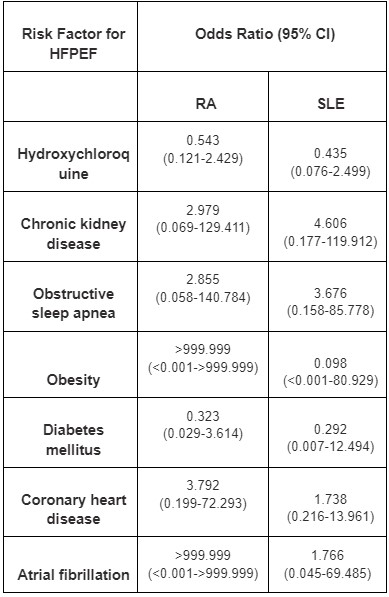 Logistic regression modeling for HFpEF diagnosis among propensity matched RA (left column) and SLE (right column) patients. Hypertension and sex were forced in the propensity matching algorithm and were thus not included in the logistic regression.
Logistic regression modeling for HFpEF diagnosis among propensity matched RA (left column) and SLE (right column) patients. Hypertension and sex were forced in the propensity matching algorithm and were thus not included in the logistic regression. Disclosures: J. Altier, None; F. Mutiso, None; P. Nietert, None; S. Litwin, None; J. Oates, None.

