Back
Poster Session B
Epidemiology, health policy and outcomes
Session: (0695–0723) Epidemiology and Public Health Poster I
0721: Inflammatory Rheumatic Disease and the Risk of Death Related to Coronavirus Disease-19 (COVID-19): An Analysis of the UK Biobank with Stratification by Sex
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- AA
Ashley Archer, BS
UAB Heersink School of Medicine
Decatur, AL, United States
Abstract Poster Presenter(s)
Ashley Archer1, Ruth Topless2, Angelo Gaffo1, Nicola Dalbeth3, Lisa Stamp4, Philip Robinson5 and Tony Merriman2, 1University of Alabama at Birmingham, Birmingham, AL, 2University of Otago, Dunedin, New Zealand, 3University of Auckland, Auckland, New Zealand, 4University of Otago, Christchurch, New Zealand, 5School of Clinical Medicine, University of Queensland, Brisbane, Australia
Background/Purpose: There is increasing evidence that rheumatoid arthritis (RA) is a risk factor for death related to COVID-19, however data on the risk of death for other inflammatory arthropathies is equivocal or non-existent. Our primary objective was to assess whether certain inflammatory rheumatic diseases (IRDs) like rheumatoid arthritis (RA), ankylosing spondylitis (AS), giant cell arteritis (GCA), psoriatic arthritis (PsA), scleroderma, Sjögren's syndrome (SS) and systemic lupus erythematosus (SLE) are risk factors for diagnosis of COVID-19 and death related to COVID-19. The secondary objective was to test for sex-specific differences in the risk of death related to COVID-19 in RA and a combined cohort of other IRDs.
Methods: We used data from the UK Biobank that included 5,973 people diagnosed with RA, 1,070 with ankylosing spondylitis, 996 with giant cell arteritis, 4,976 with psoriatic arthritis, 302 with scleroderma, 1,111 with Sjögren's syndrome, and 289 with SLE. Three logistic regression models were employed to test for association of the IRDs with death related to COVID-19 in the entire UK Biobank cohort (n=471,743): unadjusted; adjusted for demographic variables (Model 1) and adjusted by demographic variables, seventeen co-morbid diseases, and the other IRDs (Model 2). The analysis was repeated in sex-stratified cohorts for RA and for AS+PsA+scleroderma+SS+SLE.
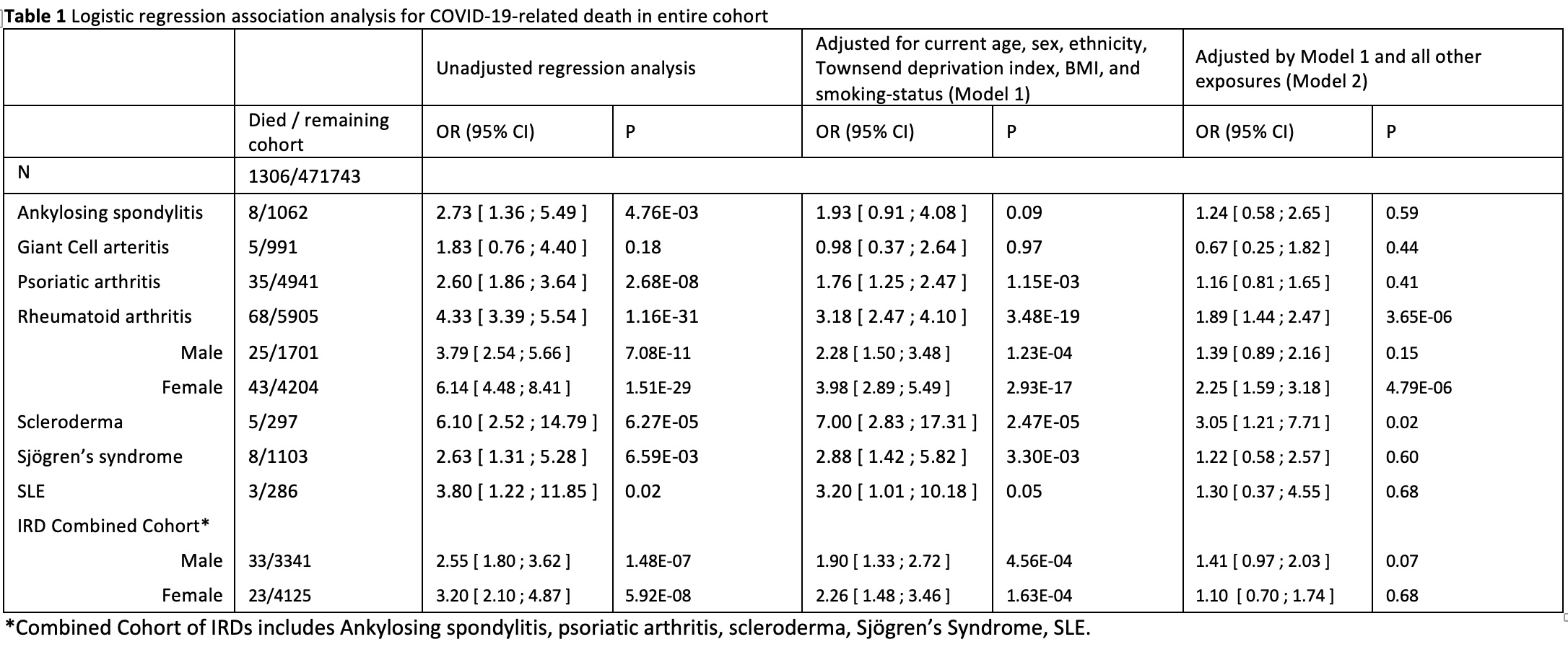
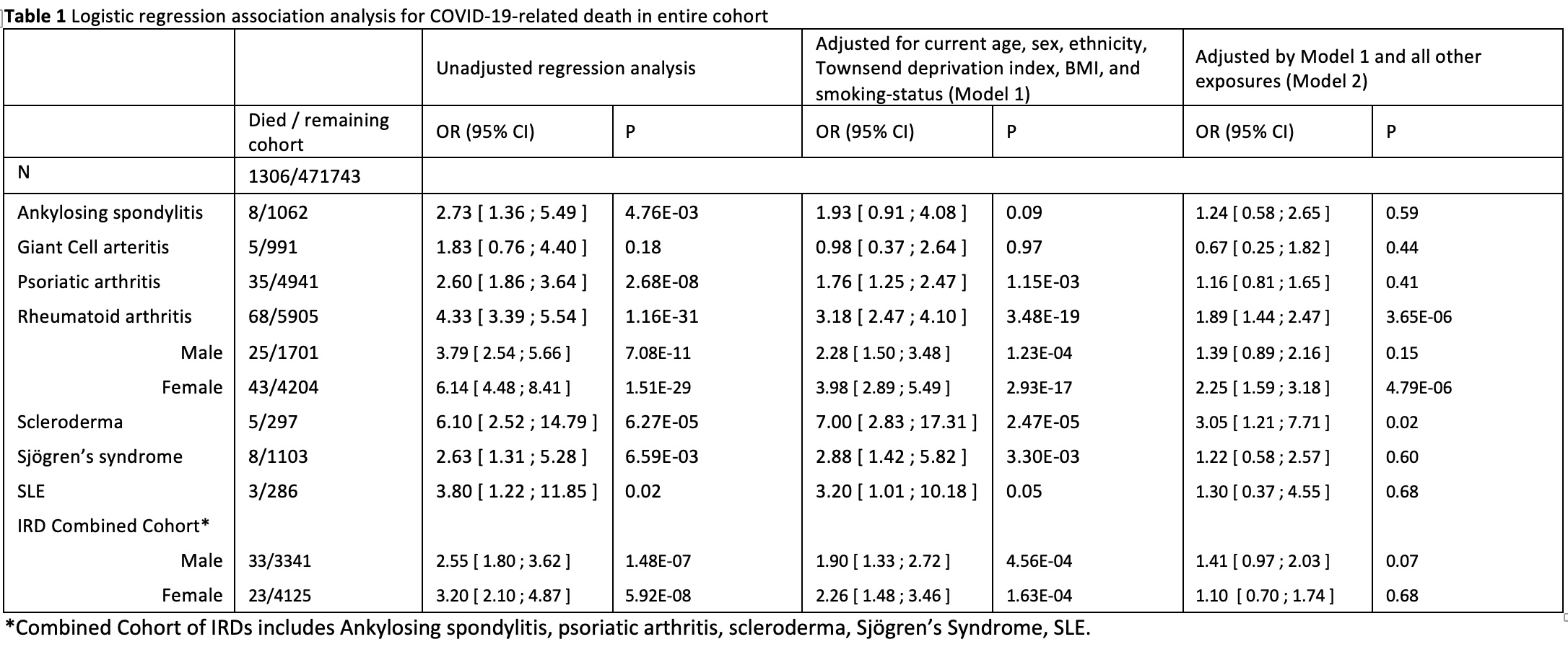
Results: There was no evidence for association of GCA with death related to COVID-19 in any of the models (Table 1), therefore GCA was not included in the following analyses. There was strong evidence (P< 1x10-4) for association of RA, PsA and scleroderma with death in the unadjusted model, RA and scleroderma in Model 1 and only for RA in Model 2 (OR=1.9 [95% CI 1.4 ; 2.5]). In Model 2, the only other IRD associated with death was scleroderma (OR=3.1 [1.2 ; 7.7]). In sex-specific analysis, the risk of death for women with RA (OR=2.2 [1.6 ; 3.2]) was significant but not for men in Model 2 (OR=1.4 [0.9 ; 2.2]). Under the hypothesis that any sex specific effect would be common to the IRDs, and to increase power to detect any effect, we combined AS+PsA+scleroderma+SS+SLE. There was no statistically significant evidence for association with death related to COVID-19 in either females (OR=1.1 [0.7 ; 1.7]) or males (OR=1.4 [1.0 ; 2.0]).
Conclusion: We provide further evidence that RA is a risk factor for death related to COVID-19 independent of various co-morbidities. There was an increased risk in women, however this was not statistically greater than in men (the 95% CIs overlapped). There was weak evidence for association of scleroderma with death related to COVID-19 in the fully adjusted Model, and no evidence for a sex-specific effect on risk of death in five other IRDs combined. However, the non-RA analyses were limited by the lower prevalence in the UK Biobank of some of the IRDs, in particular SLE and scleroderma (< 0.1%).
Disclosures: A. Archer, None; R. Topless, None; A. Gaffo, None; N. Dalbeth, AstraZeneca, Dyve Biosciences, Horizon, Selecta, JW Pharmaceutical Corporation, PK Med, PTC Therapeutics, Protalix; L. Stamp, None; P. Robinson, Pfizer, AbbVie/Abbott, Novartis, UCB, GlaxoSmithKlein(GSK), Janssen, Eli Lilly, Kukdong, Atom Biosciences; T. Merriman, None.
Background/Purpose: There is increasing evidence that rheumatoid arthritis (RA) is a risk factor for death related to COVID-19, however data on the risk of death for other inflammatory arthropathies is equivocal or non-existent. Our primary objective was to assess whether certain inflammatory rheumatic diseases (IRDs) like rheumatoid arthritis (RA), ankylosing spondylitis (AS), giant cell arteritis (GCA), psoriatic arthritis (PsA), scleroderma, Sjögren's syndrome (SS) and systemic lupus erythematosus (SLE) are risk factors for diagnosis of COVID-19 and death related to COVID-19. The secondary objective was to test for sex-specific differences in the risk of death related to COVID-19 in RA and a combined cohort of other IRDs.
Methods: We used data from the UK Biobank that included 5,973 people diagnosed with RA, 1,070 with ankylosing spondylitis, 996 with giant cell arteritis, 4,976 with psoriatic arthritis, 302 with scleroderma, 1,111 with Sjögren's syndrome, and 289 with SLE. Three logistic regression models were employed to test for association of the IRDs with death related to COVID-19 in the entire UK Biobank cohort (n=471,743): unadjusted; adjusted for demographic variables (Model 1) and adjusted by demographic variables, seventeen co-morbid diseases, and the other IRDs (Model 2). The analysis was repeated in sex-stratified cohorts for RA and for AS+PsA+scleroderma+SS+SLE.
Results: There was no evidence for association of GCA with death related to COVID-19 in any of the models (Table 1), therefore GCA was not included in the following analyses. There was strong evidence (P< 1x10-4) for association of RA, PsA and scleroderma with death in the unadjusted model, RA and scleroderma in Model 1 and only for RA in Model 2 (OR=1.9 [95% CI 1.4 ; 2.5]). In Model 2, the only other IRD associated with death was scleroderma (OR=3.1 [1.2 ; 7.7]). In sex-specific analysis, the risk of death for women with RA (OR=2.2 [1.6 ; 3.2]) was significant but not for men in Model 2 (OR=1.4 [0.9 ; 2.2]). Under the hypothesis that any sex specific effect would be common to the IRDs, and to increase power to detect any effect, we combined AS+PsA+scleroderma+SS+SLE. There was no statistically significant evidence for association with death related to COVID-19 in either females (OR=1.1 [0.7 ; 1.7]) or males (OR=1.4 [1.0 ; 2.0]).
Conclusion: We provide further evidence that RA is a risk factor for death related to COVID-19 independent of various co-morbidities. There was an increased risk in women, however this was not statistically greater than in men (the 95% CIs overlapped). There was weak evidence for association of scleroderma with death related to COVID-19 in the fully adjusted Model, and no evidence for a sex-specific effect on risk of death in five other IRDs combined. However, the non-RA analyses were limited by the lower prevalence in the UK Biobank of some of the IRDs, in particular SLE and scleroderma (< 0.1%).
Disclosures: A. Archer, None; R. Topless, None; A. Gaffo, None; N. Dalbeth, AstraZeneca, Dyve Biosciences, Horizon, Selecta, JW Pharmaceutical Corporation, PK Med, PTC Therapeutics, Protalix; L. Stamp, None; P. Robinson, Pfizer, AbbVie/Abbott, Novartis, UCB, GlaxoSmithKlein(GSK), Janssen, Eli Lilly, Kukdong, Atom Biosciences; T. Merriman, None.

