Back
Poster Session B
Juvenile idiopathic arthritis (JIA) and pediatric joint disorders
Session: (0850–0880) Pediatric Rheumatology – Clinical Poster I: JIA
0865: Opioid Use in Youth with Inflammatory Bowel Disease (IBD)-related Arthritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- AB
Atiye Bilgic Dagci, MD
University of Michigan Department of Pediatric Rheumatology
Ann Arbor, MI, United States
Abstract Poster Presenter(s)
Atiye Bilgic Dagci1, Joyce Chang2, Rui Xiao3, Andrew Grossman4 and Pamela Weiss5, 1Children's Hospital of Philadelphia, Bala Cynwyd, PA, 2Boston Children's Hospital, Boston, MA, 3University of Pennsylvania, Philadelphia, PA, 4Children's Hospital of Philadelphia, Philadelphia, 5Children's Hospital of Philadelphia, Glen Mills, PA
Background/Purpose: Opioid use is common among youth with IBD and associated with increased health care utilization and opioid dependence. Arthritis affects up to 20% of youth with IBD and may increase risk of chronic opioid use. This study aimed to assess trends and clinical features associated with opioid use in this understudied population.
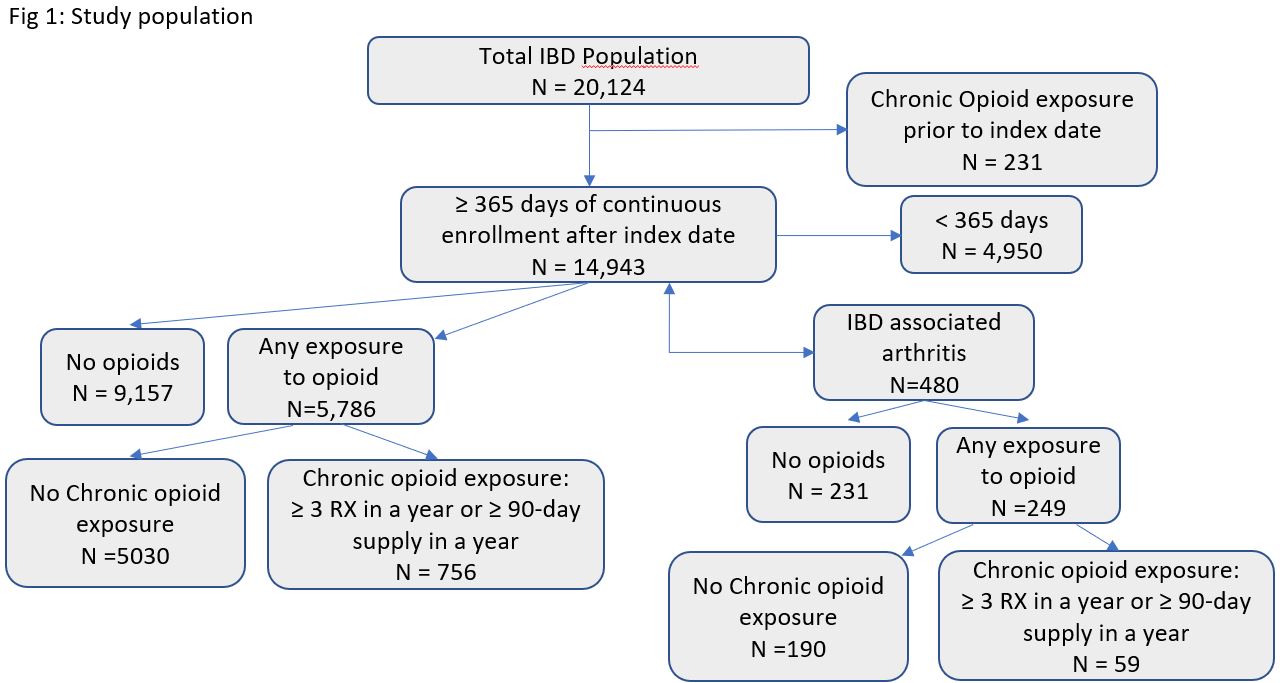
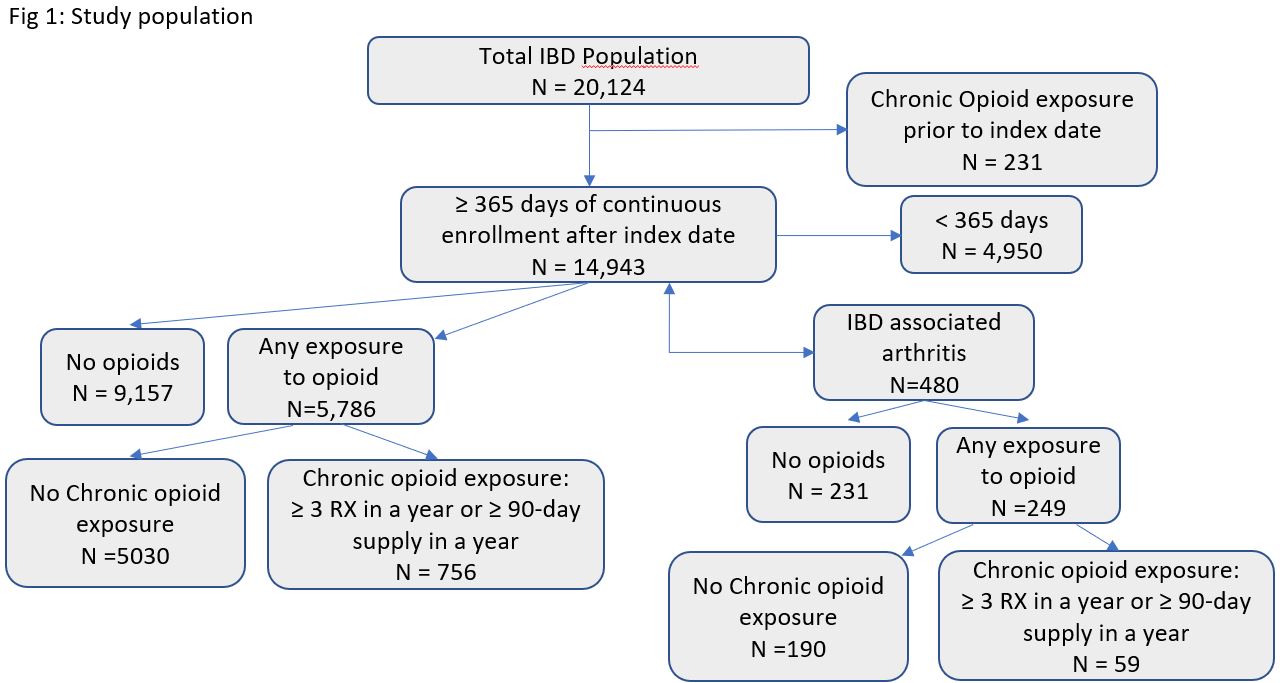
Methods: This was a retrospective cohort study of youth less than 18 years of age with IBD-related arthritis with at least 1 year of continuous enrollment and at least 1 pharmacy claim in the Truven Health MarketScan Claims and Encounter Database (2013-2018). Subjects with IBD and arthritis were identified using previously validated algorithms consisting of ICD codes, pharmacy claims and procedure codes. The primary outcome was chronic opioid exposure, which was defined as ≥3 prescription claims or ≥90-day supply filled within 1 year. The baseline period was defined as 6 months after inclusion criteria were met. Temporal trends in chronic opioid exposure were tested using the Cuzick-Wilcoxon non-parametric test of trend. We examined the association of chronic opioid use and baseline covariates, including arthritis, using a multivariable logistic regression model built with forward selection. Next, we examined the association of chronic opioid use and baseline covariates in the subset of youth with IBD-related arthritis using the same multivariable logistic model selection technique.
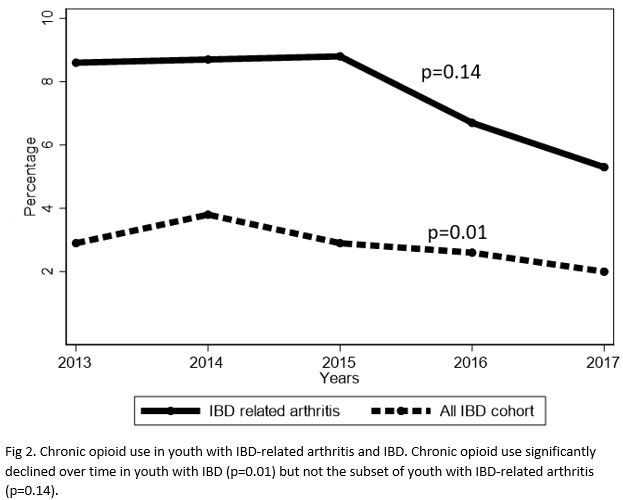
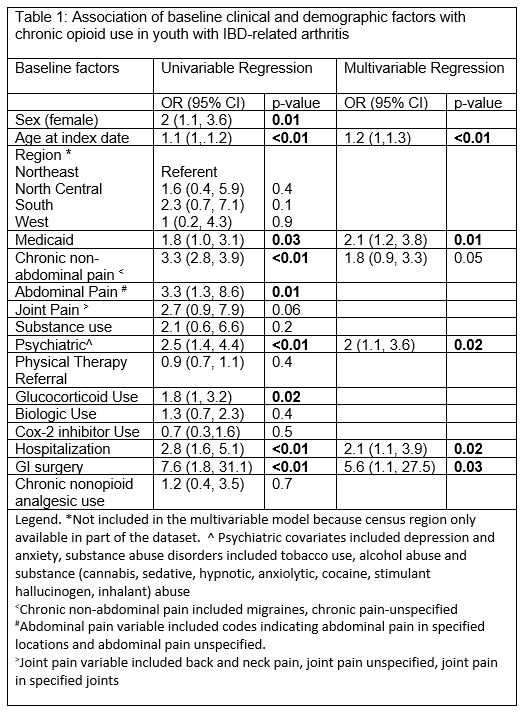
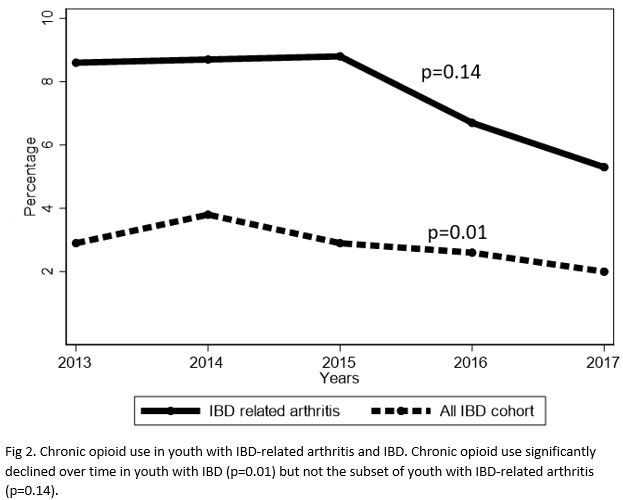
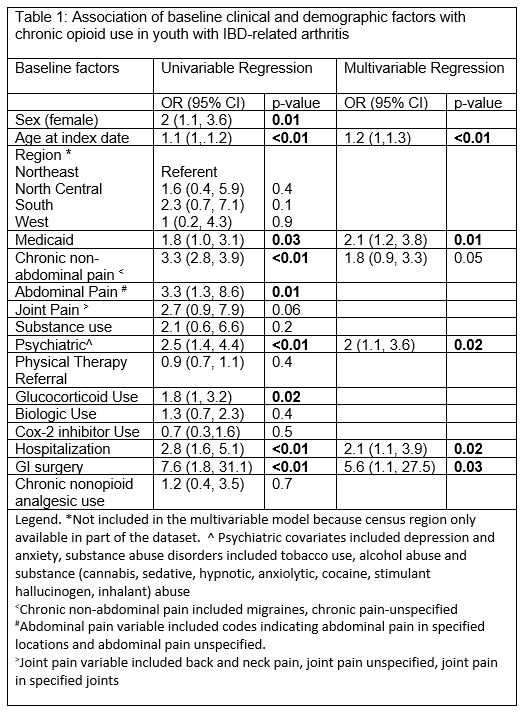
Results: A total of 14,943 youth with IBD met inclusion criteria, 480 of whom had IBD-related arthritis. 5786 (38%) and 249 (51%) of youth with IBD and IBD-related arthritis filled ≥1 opioid prescription during the study period, respectively. A significantly higher proportion of IBD-related arthritis cohort (59, 12.3%) met criteria for chronic opioid use in comparison to entire IBD cohort (756, 5%) (Fig 1; p < 0.01). Prevalent chronic opioid use over the study period varied between 2 to 3.8% in youth with IBD and 5.3 to 8.6 % in youth with IBD-related arthritis (Fig 2). Chronic opioid use significantly declined over time in youth with IBD (p=0.01) but not IBD-related arthritis (p=0.14). Using multivariable logistic regression, arthritis was significantly associated with chronic opioid exposure in youth with IBD independent of other covariates. (OR:1.6 95% CI: 1.4-2.7). Results of univariate and multivariate logistic regression for the association of chronic opioid use with covariates in youth with IBD-related arthritis are shown in Table 1. Among IBD-related arthritis patients; older age, public insurance, gastrointestinal surgeries, hospitalizations and psychiatric comorbidities within the baseline period were significantly associated with chronic opioid use.
Conclusion: Chronic opioid use was non-trivial in youth with IBD-related arthritis, higher than that of total IBD cohort, and remained stable over the years of study. Older age, public insurance, gastrointestinal surgery, hospitalizations, and psychiatric comorbidities were significantly associated with chronic opioid use. Future study is needed to explore ways to optimize non-narcotic pain management strategies and ensuring appropriate use of opioids when necessary.
Disclosures: A. Bilgic Dagci, None; J. Chang, GlaxoSmithKline (GSK); R. Xiao, None; A. Grossman, None; P. Weiss, None.
Background/Purpose: Opioid use is common among youth with IBD and associated with increased health care utilization and opioid dependence. Arthritis affects up to 20% of youth with IBD and may increase risk of chronic opioid use. This study aimed to assess trends and clinical features associated with opioid use in this understudied population.
Methods: This was a retrospective cohort study of youth less than 18 years of age with IBD-related arthritis with at least 1 year of continuous enrollment and at least 1 pharmacy claim in the Truven Health MarketScan Claims and Encounter Database (2013-2018). Subjects with IBD and arthritis were identified using previously validated algorithms consisting of ICD codes, pharmacy claims and procedure codes. The primary outcome was chronic opioid exposure, which was defined as ≥3 prescription claims or ≥90-day supply filled within 1 year. The baseline period was defined as 6 months after inclusion criteria were met. Temporal trends in chronic opioid exposure were tested using the Cuzick-Wilcoxon non-parametric test of trend. We examined the association of chronic opioid use and baseline covariates, including arthritis, using a multivariable logistic regression model built with forward selection. Next, we examined the association of chronic opioid use and baseline covariates in the subset of youth with IBD-related arthritis using the same multivariable logistic model selection technique.
Results: A total of 14,943 youth with IBD met inclusion criteria, 480 of whom had IBD-related arthritis. 5786 (38%) and 249 (51%) of youth with IBD and IBD-related arthritis filled ≥1 opioid prescription during the study period, respectively. A significantly higher proportion of IBD-related arthritis cohort (59, 12.3%) met criteria for chronic opioid use in comparison to entire IBD cohort (756, 5%) (Fig 1; p < 0.01). Prevalent chronic opioid use over the study period varied between 2 to 3.8% in youth with IBD and 5.3 to 8.6 % in youth with IBD-related arthritis (Fig 2). Chronic opioid use significantly declined over time in youth with IBD (p=0.01) but not IBD-related arthritis (p=0.14). Using multivariable logistic regression, arthritis was significantly associated with chronic opioid exposure in youth with IBD independent of other covariates. (OR:1.6 95% CI: 1.4-2.7). Results of univariate and multivariate logistic regression for the association of chronic opioid use with covariates in youth with IBD-related arthritis are shown in Table 1. Among IBD-related arthritis patients; older age, public insurance, gastrointestinal surgeries, hospitalizations and psychiatric comorbidities within the baseline period were significantly associated with chronic opioid use.
Conclusion: Chronic opioid use was non-trivial in youth with IBD-related arthritis, higher than that of total IBD cohort, and remained stable over the years of study. Older age, public insurance, gastrointestinal surgery, hospitalizations, and psychiatric comorbidities were significantly associated with chronic opioid use. Future study is needed to explore ways to optimize non-narcotic pain management strategies and ensuring appropriate use of opioids when necessary.
Disclosures: A. Bilgic Dagci, None; J. Chang, GlaxoSmithKline (GSK); R. Xiao, None; A. Grossman, None; P. Weiss, None.

