Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0679: Outcomes of Antiphospholipid Antibody Syndrome and Acute Coronary Syndrome: Analysis of National Inpatient Sample
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- FS
Faria Sami, MD, MBBS
John H. Stroger Hospital of Cook County
Chicago, IL, United States
Abstract Poster Presenter(s)
Faria Sami, Dennis Kumi and Shilpa Arora, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Background/Purpose: Antiphospholipid antibody syndrome (APLS) is strongly associated with the risk of cardiovascular events including acute coronary syndrome (ACS). However, there is limited data on the clinical characteristics and outcomes of APLS patients who develop ACS. We aimed to investigate the inpatient outcomes of ACS hospitalizations with and without APLS.
Methods: National inpatient sample (NIS) database from 2016 to 2018 was used to extract data. Hospitalizations with the principal diagnosis of ACS with and without secondary diagnosis of APLS were searched. Only adult patients above the age of 18 years were included. The primary outcome was mortality and secondary outcomes included health care burden (length of stay and charges) and cardiac complications of ventricular tachycardia, hypotension, cardiac arrest, cardiogenic shock, intra-aortic balloon pump and acute venous thromboembolism (VTE). We performed multivariate logistic regression analyses to adjust for confounders.
Results: There were a total of 1,945,054 hospitalizations for ACS. Of the ACS admissions, 1,775 had associated APLS accounting for 0.092% hospitalizations (Table 1). Patients with ACS and APLS were younger in comparison to those without APLS (58.89 vs 66.81 years, 95% CI -9.51 to -6.33, P value < 0.001). Females with ACS were more likely to have the concomitant diagnosis of APLS with an adjusted OR of 2.41 (95% CI 1.93 to 3.01, P value < 0.001). The primary outcome of mortality was not different between the two groups (3.96% in ACS and APLS vs 4.56% ACS without APLS, P value 0.78) (Table 2). The length of stay was longer in patients with ACS and APLS (6.52 vs 4.39 days, 95% CI 0.92 to 2.74, P value < 0.001) but total charges were not statistically different. Secondary outcomes of ventricular tachycardia, hypotension, cardiac arrest, intra-aortic balloon pump and cardiogenic shock were also comparable between the two groups with no statistically significant difference. Remarkably, the risk of acute VTE in patients with ACS and APLS was increased 7-fold with the adjusted OR of 7.52 (95% CI 5.02-11.26, P value < 0.001).
Conclusion: ACS and APLS patients were younger and more likely to be females adding to the existing literature that APLS is a risk factor for ACS especially in young women. APLS did not impact mortality or other cardiac complications in patients with ACS. There was however a striking 7-fold increased risk of developing acute VTE in patients with ACS and APLS which underscores the importance of anticoagulation in these patients.
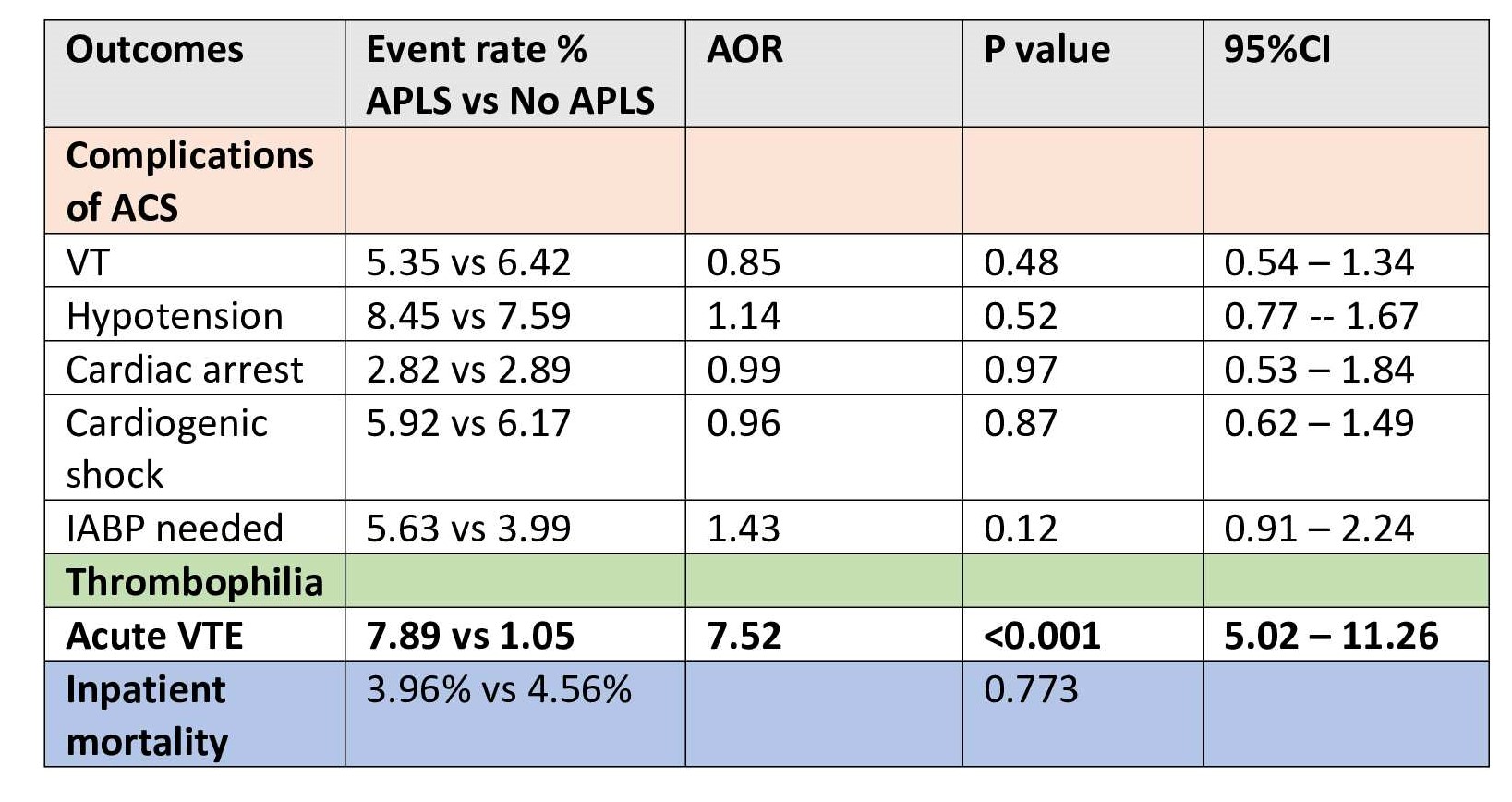 Outcomes in ACS patients with and without APLS
Outcomes in ACS patients with and without APLS
Disclosures: F. Sami, None; D. Kumi, None; S. Arora, None.
Background/Purpose: Antiphospholipid antibody syndrome (APLS) is strongly associated with the risk of cardiovascular events including acute coronary syndrome (ACS). However, there is limited data on the clinical characteristics and outcomes of APLS patients who develop ACS. We aimed to investigate the inpatient outcomes of ACS hospitalizations with and without APLS.
Methods: National inpatient sample (NIS) database from 2016 to 2018 was used to extract data. Hospitalizations with the principal diagnosis of ACS with and without secondary diagnosis of APLS were searched. Only adult patients above the age of 18 years were included. The primary outcome was mortality and secondary outcomes included health care burden (length of stay and charges) and cardiac complications of ventricular tachycardia, hypotension, cardiac arrest, cardiogenic shock, intra-aortic balloon pump and acute venous thromboembolism (VTE). We performed multivariate logistic regression analyses to adjust for confounders.
Results: There were a total of 1,945,054 hospitalizations for ACS. Of the ACS admissions, 1,775 had associated APLS accounting for 0.092% hospitalizations (Table 1). Patients with ACS and APLS were younger in comparison to those without APLS (58.89 vs 66.81 years, 95% CI -9.51 to -6.33, P value < 0.001). Females with ACS were more likely to have the concomitant diagnosis of APLS with an adjusted OR of 2.41 (95% CI 1.93 to 3.01, P value < 0.001). The primary outcome of mortality was not different between the two groups (3.96% in ACS and APLS vs 4.56% ACS without APLS, P value 0.78) (Table 2). The length of stay was longer in patients with ACS and APLS (6.52 vs 4.39 days, 95% CI 0.92 to 2.74, P value < 0.001) but total charges were not statistically different. Secondary outcomes of ventricular tachycardia, hypotension, cardiac arrest, intra-aortic balloon pump and cardiogenic shock were also comparable between the two groups with no statistically significant difference. Remarkably, the risk of acute VTE in patients with ACS and APLS was increased 7-fold with the adjusted OR of 7.52 (95% CI 5.02-11.26, P value < 0.001).
Conclusion: ACS and APLS patients were younger and more likely to be females adding to the existing literature that APLS is a risk factor for ACS especially in young women. APLS did not impact mortality or other cardiac complications in patients with ACS. There was however a striking 7-fold increased risk of developing acute VTE in patients with ACS and APLS which underscores the importance of anticoagulation in these patients.
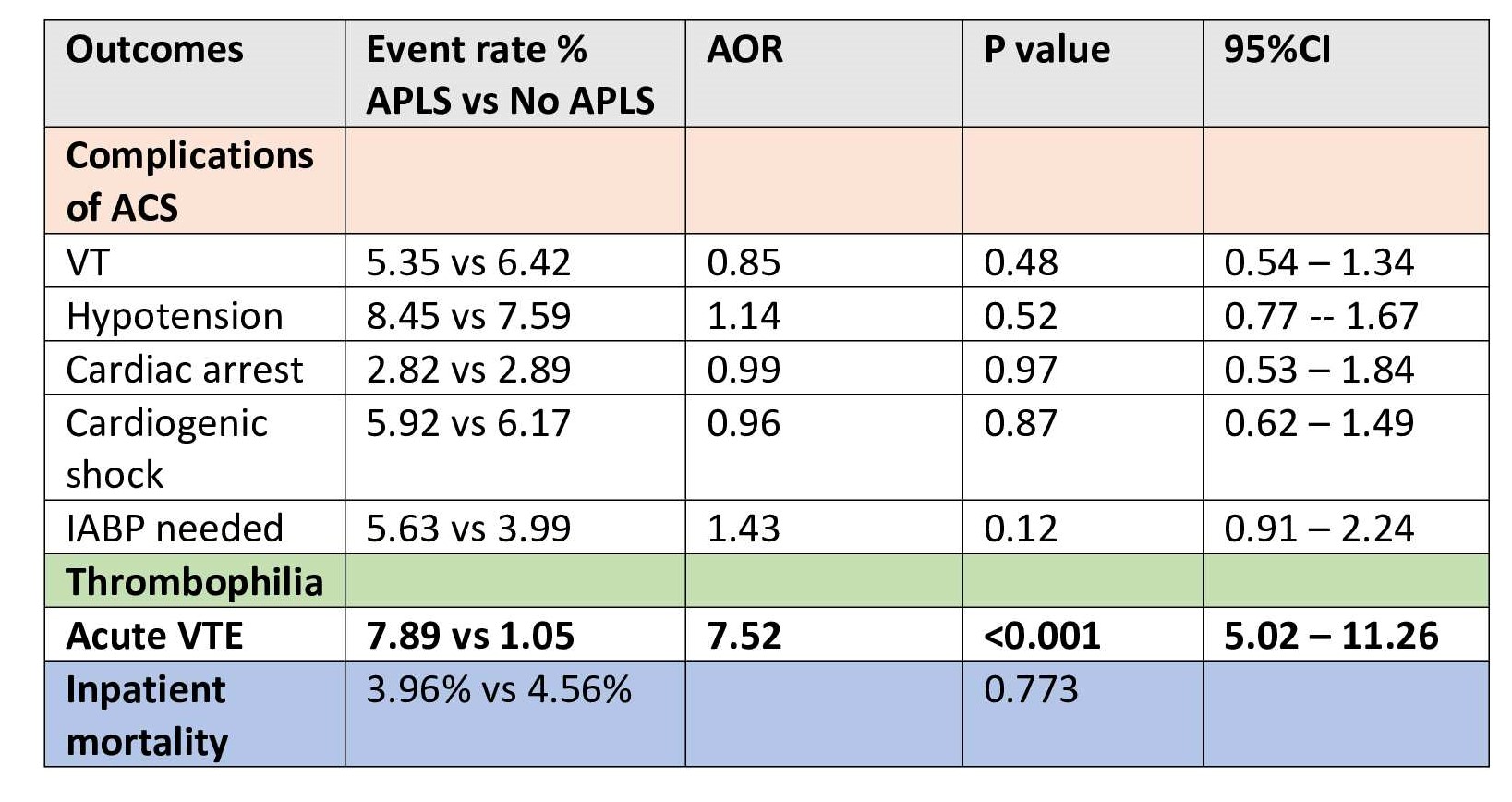 Outcomes in ACS patients with and without APLS
Outcomes in ACS patients with and without APLSDisclosures: F. Sami, None; D. Kumi, None; S. Arora, None.

