Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0674: Prevalence of Heparin Induced Thrombocytopenia in Hospitalized Patients with Antiphospholipid Syndrome or Systemic Lupus Erythematosus with Antiphospholipid Antibodies
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- VT
Vincent Tran, MD
UCLA
Los Angeles, CA, United States
Abstract Poster Presenter(s)
Vincent Tran, Amy Schmitt and Shanthini Kasturi, Tufts Medical Center, Boston, MA
Background/Purpose: Thrombosis and thrombocytopenia are defining characteristics of antiphospholipid syndrome (APS), but can also be seen in heparin-induced thrombocytopenia (HIT). Hospitalized patients with APS are often tested for HIT, but the prevalence of HIT in this population is unclear. Our study investigated the prevalence of HIT among high risk inpatients with APS or systemic lupus erythematosus (SLE) with antiphospholipid antibodies (aPL).
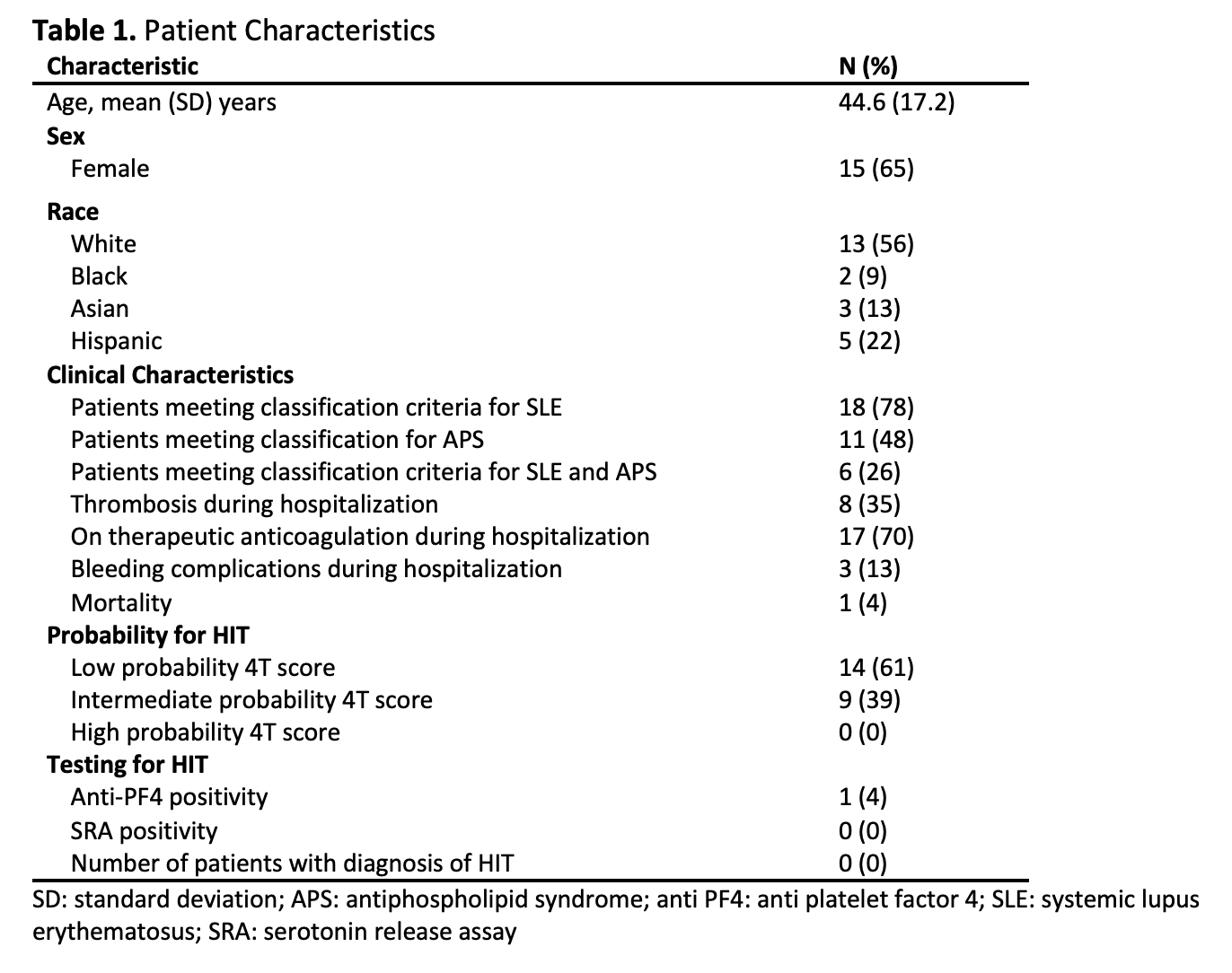
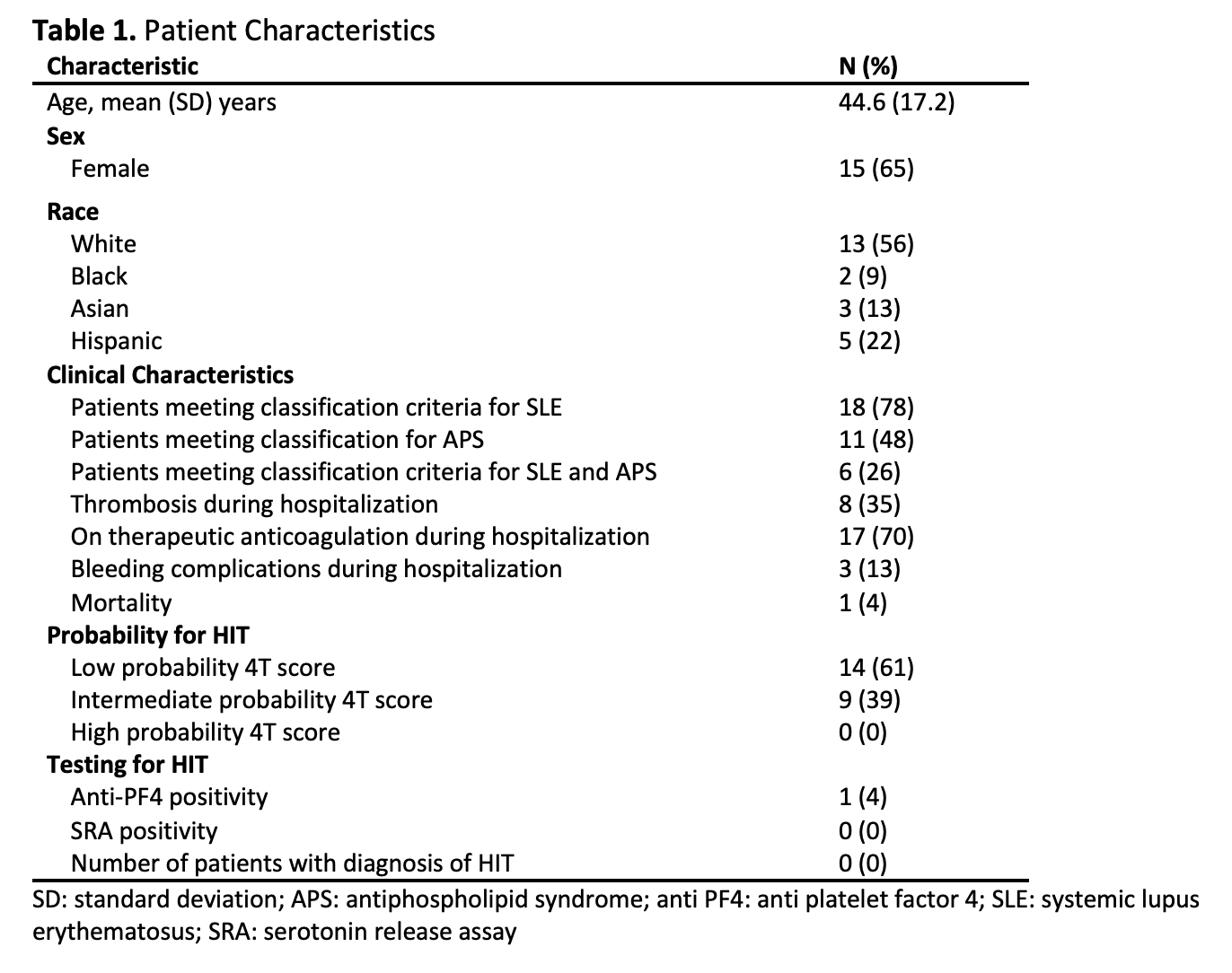
Methods: This was a retrospective cohort study of hospitalized adults meeting classification criteria for APS or SLE with aPL who were evaluated for HIT with anti-platelet factor 4 (PF4) antibodies or serotonin release assay (SRA). Patients were screened via the electronic medical record using International Classification of Diseases (ICD) codes. Of 33 patients identified in screening, 23 met study inclusion criteria (Table 1). Eighteen met 2019 American College of Rheumatology classification criteria for SLE, 11 met Sapporo classification criteria for APS, and 6 met both SLE and APS criteria. Demographics, clinical characteristics (reason for hospitalization, APS and SLE criteria, 4T score, anticoagulation status), and laboratory results (platelets, anti-PF4 antibodies, SRA) were extracted and clinical diagnosis of HIT was assessed using a positive SRA test.
Results: Of the 23 patients who met inclusion criteria, fourteen patients (61%) had a low probability 4T score, 9 (39%) with intermediate probability, and 0 with high probability. Of the 23 patients in whom PF4 antibodies were evaluated, only one patient (4%) tested positive. SRA was tested in a total of 4 patients (17%), including this patient, and was negative in all cases.
Conclusion: Among 23 inpatients with APS or SLE with aPL who were tested for HIT with anti-PF4 antibodies or SRA at a single tertiary care medical center, not one ultimately met clinical criteria for HIT. A majority of patients in this cohort had a 4T score that was low probability for a diagnosis of HIT, but were still tested for anti-PF4 antibodies. Our study suggests that the clinical syndrome of HIT is rare among hospitalized patients with APS or SLE with aPL and that anti-PF4 antibodies are often inappropriately tested for in this population.
Disclosures: V. Tran, None; A. Schmitt, None; S. Kasturi, GlaxoSmithKlein(GSK).
Background/Purpose: Thrombosis and thrombocytopenia are defining characteristics of antiphospholipid syndrome (APS), but can also be seen in heparin-induced thrombocytopenia (HIT). Hospitalized patients with APS are often tested for HIT, but the prevalence of HIT in this population is unclear. Our study investigated the prevalence of HIT among high risk inpatients with APS or systemic lupus erythematosus (SLE) with antiphospholipid antibodies (aPL).
Methods: This was a retrospective cohort study of hospitalized adults meeting classification criteria for APS or SLE with aPL who were evaluated for HIT with anti-platelet factor 4 (PF4) antibodies or serotonin release assay (SRA). Patients were screened via the electronic medical record using International Classification of Diseases (ICD) codes. Of 33 patients identified in screening, 23 met study inclusion criteria (Table 1). Eighteen met 2019 American College of Rheumatology classification criteria for SLE, 11 met Sapporo classification criteria for APS, and 6 met both SLE and APS criteria. Demographics, clinical characteristics (reason for hospitalization, APS and SLE criteria, 4T score, anticoagulation status), and laboratory results (platelets, anti-PF4 antibodies, SRA) were extracted and clinical diagnosis of HIT was assessed using a positive SRA test.
Results: Of the 23 patients who met inclusion criteria, fourteen patients (61%) had a low probability 4T score, 9 (39%) with intermediate probability, and 0 with high probability. Of the 23 patients in whom PF4 antibodies were evaluated, only one patient (4%) tested positive. SRA was tested in a total of 4 patients (17%), including this patient, and was negative in all cases.
Conclusion: Among 23 inpatients with APS or SLE with aPL who were tested for HIT with anti-PF4 antibodies or SRA at a single tertiary care medical center, not one ultimately met clinical criteria for HIT. A majority of patients in this cohort had a 4T score that was low probability for a diagnosis of HIT, but were still tested for anti-PF4 antibodies. Our study suggests that the clinical syndrome of HIT is rare among hospitalized patients with APS or SLE with aPL and that anti-PF4 antibodies are often inappropriately tested for in this population.
Disclosures: V. Tran, None; A. Schmitt, None; S. Kasturi, GlaxoSmithKlein(GSK).

