Back
Poster Session B
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1004–1034) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster II
1004: SPARCC, MASES, LEI and MEI Indexes Capture Different Patients with Enthesitis in Axial Spondyloarthritis, Peripheral Spondyloartrhitis and Psoriatic Arthritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- RG
Raquel Granados, MD
Hospital Universitario Reina Sofia
Cordoba, Spain
Abstract Poster Presenter(s)
Raquel Granados1, lourdes Ladehesa-Pineda2, Maria Angeles Puche Larrubia3, Maxime Dougados4, Eduardo Collantes5 and Clementina Lopez-Medina6, 1Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Córdoba, Spain, 2Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Cordoba, Spain, 3Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Granada, Spain, 4Department of Rheumatology, Hôpital Cochin, Paris, France, Paris, France, 5IMIBIC/University of Cordoba/Reina Sofia Hospital, Cordoba, Spain, 6Reina Sofia University Hospital, Rheumatology Department, Jaén, Spain
Background/Purpose: Spondyloarthritis, (axial (axSpA), peripheral (pSpA)) and psoriatic arthritis (PsA)) share enthesitis as a hallmark clinical feature. Reliable clinical instruments have been developed to assess enthesitis: Spondyloarthritis Research Consortium of Canada Enthesitis (SPARCC), Leeds Enthesitis Index (LEI), Maastricht Ankylosing Spondylitis Enthesitis Score (MASES) and Mander Enthesitis Index (MEI). Since these four indexes include different enthesis locations, they may capture a different number of patients with enthesitis in the different SpA entities.
For that, the purpose of the study is a) to describe the individual locations of enthesitis in axSpA, pSpA and PsA; b) to evaluate whether the prevalence of patients with at least one enthesitis across the three groups differs depending on the use of SPARCC, LEI, MASES and MEI indexes; c) to evaluate the level of agreement between these indexes for detecting patients with at least one enthesitis in axSpA, pSpA and PsA populations.
Methods: 4185 patients from the cross-sectional ASAS-PerSpA study with a diagnosis of axSpA (2719), pSpA (433) and PsA (1033) according to the Rheumatologist were included. The location of enthesitis during the study visit were evaluated according to the four indexes. The prevalence of patients with at least one enthesitis according to the different indexes were compared across the three diseases and pair-wise agreement between indexes were evaluated using the Cohen's kappa.
Results: In the overall population, 10.7%, 8.3%, 13.5% and 17.2% of patients showed at least one enthesitis according to the SPARCC, LEI, MASES and MEI indexes, respectively. Figure 1 shows that, among patients with axSpA, MEI and MASES indexes capture the majority of patients with at least one enthesitis (98.7% and 82.4%, respectively), while in pSpA and PsA, MEI and SPARCC are the indexes which capture the majority of patients with enthesitis (100% and 84.6% for MEI and SPARCC in pSpA, and 97.3% and 77% for MEI and SPARCC in PsA, respectively). In the total population, MASES and MEI showed the strongest agreement for patients with at least one enthesitis (absolute agreement 96.3%; Cohen's kappa: 0.86). Similar results were found among axSpA patients (97.3%; 0.90). In pSpA patients, SPARCC and MEI showed the strongest agreement (97.2%; 0.90), as well as among PsA patients (95.4%; 0.82).
Conclusion: The most prevalent locations of enthesitis on the global SpA population are the lumbar spinous processes, the thoracic spinous processes and Achilles tendon. MEI and MASES are the two indexes that capture more patients with enthesitis in axSpA, while MEI and SPARCC are the two indexes that capture more patients in pSpA and PsA. The LEI index may underestimate the prevalence of enthesitis in these patients. MASES and MEI showed the largest level of agreement in the overall population and in axSpA, while MEI and SPARCC showed the largest level of agreement in pSpA and PsA. These results suggest that the prevalence of enthesitis across entities differs depending on the disease and on the use of the different indexes.
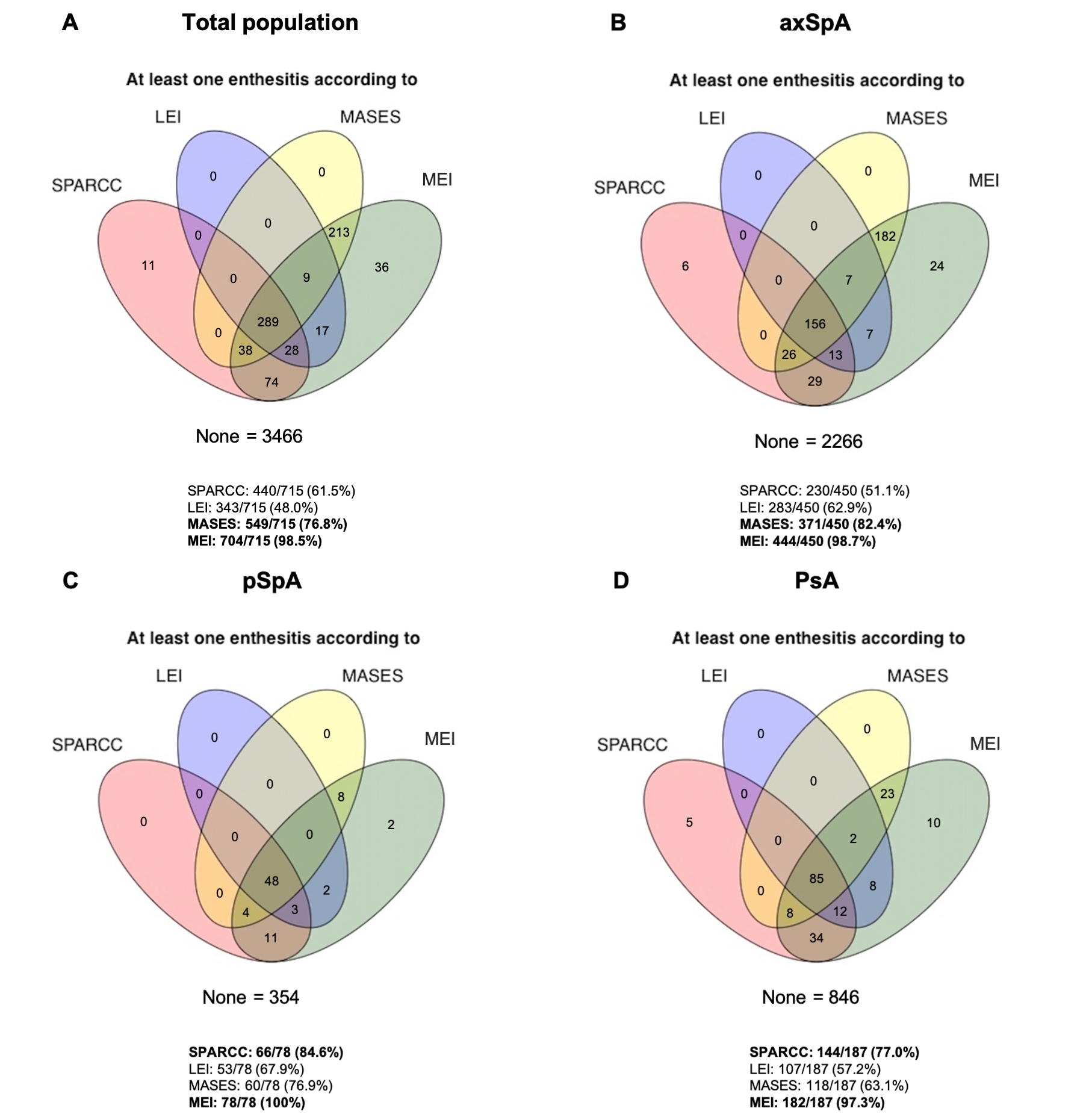 Figure 1. Prevalence of enthesitis captured by different indexes.
Figure 1. Prevalence of enthesitis captured by different indexes.
Disclosures: R. Granados, None; l. Ladehesa-Pineda, None; M. Puche Larrubia, None; M. Dougados, Novartis, AbbVie, Eli Lilly, Merck, Pfizer, UCB Pharma; E. Collantes, None; C. Lopez-Medina, None.
Background/Purpose: Spondyloarthritis, (axial (axSpA), peripheral (pSpA)) and psoriatic arthritis (PsA)) share enthesitis as a hallmark clinical feature. Reliable clinical instruments have been developed to assess enthesitis: Spondyloarthritis Research Consortium of Canada Enthesitis (SPARCC), Leeds Enthesitis Index (LEI), Maastricht Ankylosing Spondylitis Enthesitis Score (MASES) and Mander Enthesitis Index (MEI). Since these four indexes include different enthesis locations, they may capture a different number of patients with enthesitis in the different SpA entities.
For that, the purpose of the study is a) to describe the individual locations of enthesitis in axSpA, pSpA and PsA; b) to evaluate whether the prevalence of patients with at least one enthesitis across the three groups differs depending on the use of SPARCC, LEI, MASES and MEI indexes; c) to evaluate the level of agreement between these indexes for detecting patients with at least one enthesitis in axSpA, pSpA and PsA populations.
Methods: 4185 patients from the cross-sectional ASAS-PerSpA study with a diagnosis of axSpA (2719), pSpA (433) and PsA (1033) according to the Rheumatologist were included. The location of enthesitis during the study visit were evaluated according to the four indexes. The prevalence of patients with at least one enthesitis according to the different indexes were compared across the three diseases and pair-wise agreement between indexes were evaluated using the Cohen's kappa.
Results: In the overall population, 10.7%, 8.3%, 13.5% and 17.2% of patients showed at least one enthesitis according to the SPARCC, LEI, MASES and MEI indexes, respectively. Figure 1 shows that, among patients with axSpA, MEI and MASES indexes capture the majority of patients with at least one enthesitis (98.7% and 82.4%, respectively), while in pSpA and PsA, MEI and SPARCC are the indexes which capture the majority of patients with enthesitis (100% and 84.6% for MEI and SPARCC in pSpA, and 97.3% and 77% for MEI and SPARCC in PsA, respectively). In the total population, MASES and MEI showed the strongest agreement for patients with at least one enthesitis (absolute agreement 96.3%; Cohen's kappa: 0.86). Similar results were found among axSpA patients (97.3%; 0.90). In pSpA patients, SPARCC and MEI showed the strongest agreement (97.2%; 0.90), as well as among PsA patients (95.4%; 0.82).
Conclusion: The most prevalent locations of enthesitis on the global SpA population are the lumbar spinous processes, the thoracic spinous processes and Achilles tendon. MEI and MASES are the two indexes that capture more patients with enthesitis in axSpA, while MEI and SPARCC are the two indexes that capture more patients in pSpA and PsA. The LEI index may underestimate the prevalence of enthesitis in these patients. MASES and MEI showed the largest level of agreement in the overall population and in axSpA, while MEI and SPARCC showed the largest level of agreement in pSpA and PsA. These results suggest that the prevalence of enthesitis across entities differs depending on the disease and on the use of the different indexes.
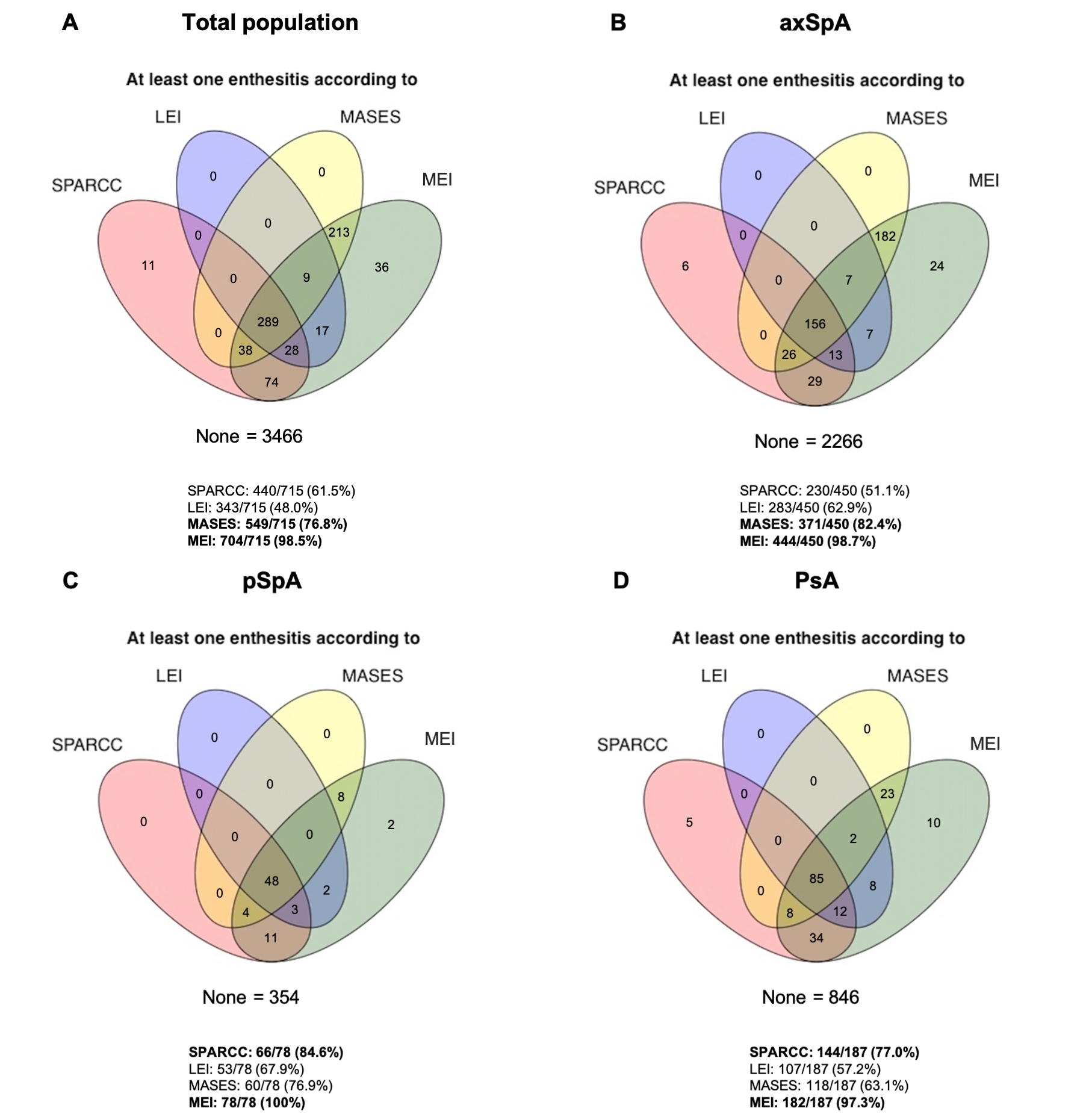 Figure 1. Prevalence of enthesitis captured by different indexes.
Figure 1. Prevalence of enthesitis captured by different indexes.Disclosures: R. Granados, None; l. Ladehesa-Pineda, None; M. Puche Larrubia, None; M. Dougados, Novartis, AbbVie, Eli Lilly, Merck, Pfizer, UCB Pharma; E. Collantes, None; C. Lopez-Medina, None.

