Back
Poster Session B
Infection-related rheumatic syndromes
Session: (0779–0806) Infection-related Rheumatic Disease Poster
0789: The Persistence of Anti-Spike Antibodies Following Two SARS-CoV-2 Vaccine Doses in Patients with Immune-mediated Inflammatory Diseases on Immunosuppressive Therapy Compared to Healthy Controls: A Prospective Cohort Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- IC
Ingrid Christensen, MD
Diakonhjemmet Hospital
Oslo, Norway
Abstract Poster Presenter(s)
Ingrid Egeland Christensen1, Ingrid Jyssum1, Anne Therese Tveter1, Joe Sexton1, Siri Mjaaland2, Grete Birkeland Kro3, Tore K. Kvien1, David Warren3, Jørgen Jahnsen4, Ludvig A. Munthe3, Espen Haavardsholm1, Gunnveig Grødeland3, Kristin Kaasen Jørgensen4, Silje Watterdal Syversen1, Guro Løvik Goll1 and Sella Aarrestad Provan1, 1Diakonhjemmet Hospital, Oslo, Norway, 2Norwegian Institute of Public Health, Oslo, Norway, 3Oslo University Hospital, Oslo, Norway, 4Akershus University Hospital, Oslo, Norway
Background/Purpose: The durability of vaccine-induced humoral immunity against SARS-CoV-2 in patients with immune-mediated inflammatory diseases (IMIDs) on immunosuppressive therapy is not well characterized. The aim of this study was to compare the persistence of anti-Spike antibodies following two-dose SARS-CoV-2 vaccination between IMID patients and healthy controls, and to identify factors associated with antibody decline.
Methods: IMID patients on immunosuppressive medication enrolled in the prospective observational Nor-vaC study were included. Participants received two-dose SARS-CoV-2 vaccination. Serum collected at two time points following vaccination (first assessment within 6–48 days, second within 49–123 days) were analysed for antibodies binding the receptor-binding domain (RBD) of the SARS-CoV-2 Spike protein. Multivariable regression models estimated percent reduction in anti-RBD over 30 days and factors associated with reduction.
Results: A total of 1108 patients (403 rheumatoid arthritis, 195 psoriatic arthritis, 195 spondyloarthritis, 124 ulcerative colitis, 191 Crohn´s disease) and 134 controls provided blood samples within the defined intervals (median 19 days [IQR 15–24] and 97 days [87–105] after second vaccine dose). Antibody levels were lower in patients compared to controls at both time points, with median anti-RBD 2806 BAU/ml [IQR 1018–6068] in patients and 6187 BAU/ml [4105–7496] in controls (p< 0.001) at first assessment, and 608 BAU/ml [IQR 58–1053] in patients and 1520 BAU/ml [979–3766] in controls (p< 0.001) at second assessment. At second assessment, low anti-RBD antibody levels (defined as < 200 BAU/ml) were found in 449 (41%) patients, and 6 (5%) controls (p< 0.001). The change was -83% in patients and -66% in controls (p< 0.001). Patients had a greater estimated 30 days percent reduction in anti-RBD levels compared to controls -4.9 (95% CI -7.4 – -2.4), (p< 0.05). Among therapies, mono- or combination treatment with tumor necrosis factor inhibitors were associated with the greatest decline.
Conclusion: Within 4 months after vaccination, antibody levels declined considerably in both IMID patients and controls. Patients had lower initial antibody levels and a more pronounced decline compared to healthy controls, and were therefore more likely to decline to low antibody levels. These results support that additional vaccine doses may be of particular importance in IMID patients who may also need this at an earlier stage than healthy individuals.
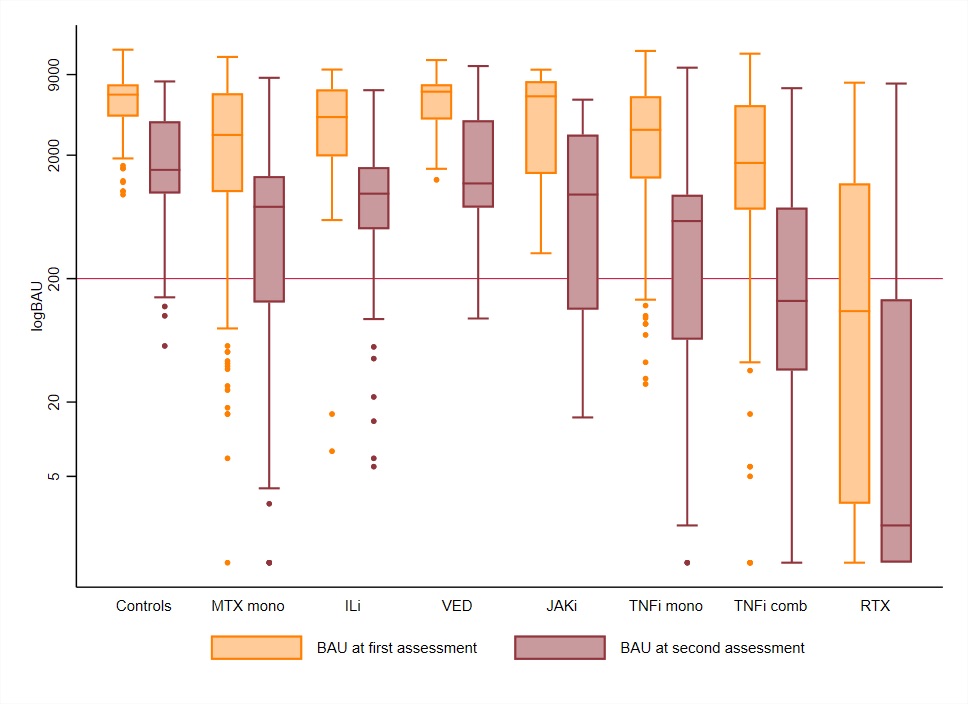 Figure 1. Levels of anti-RBD antibodies at first and second assessment according to medication groups
Figure 1. Levels of anti-RBD antibodies at first and second assessment according to medication groups
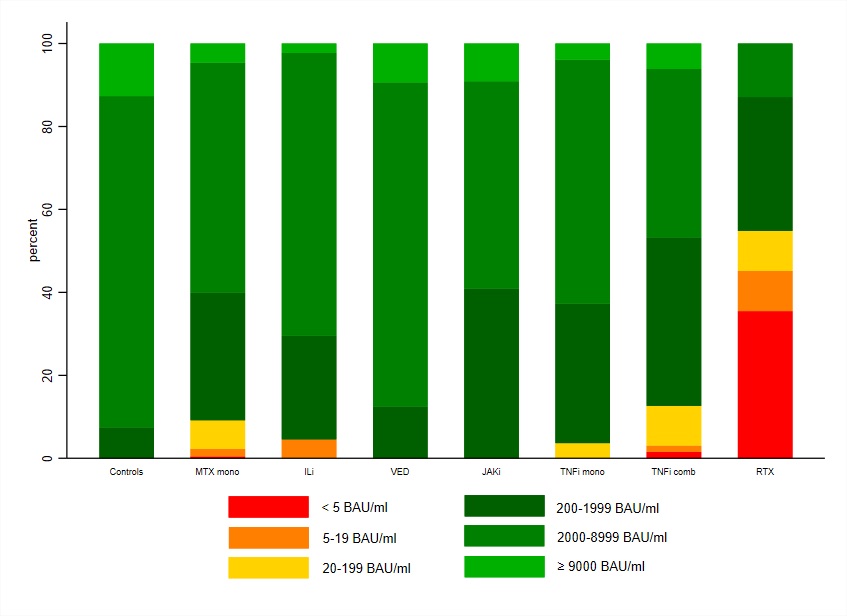 Figure 2. Percent distribution of anti-RBD levels at the first (A) and second (B) assessment in patients and healthy controls
Figure 2. Percent distribution of anti-RBD levels at the first (A) and second (B) assessment in patients and healthy controls
A)
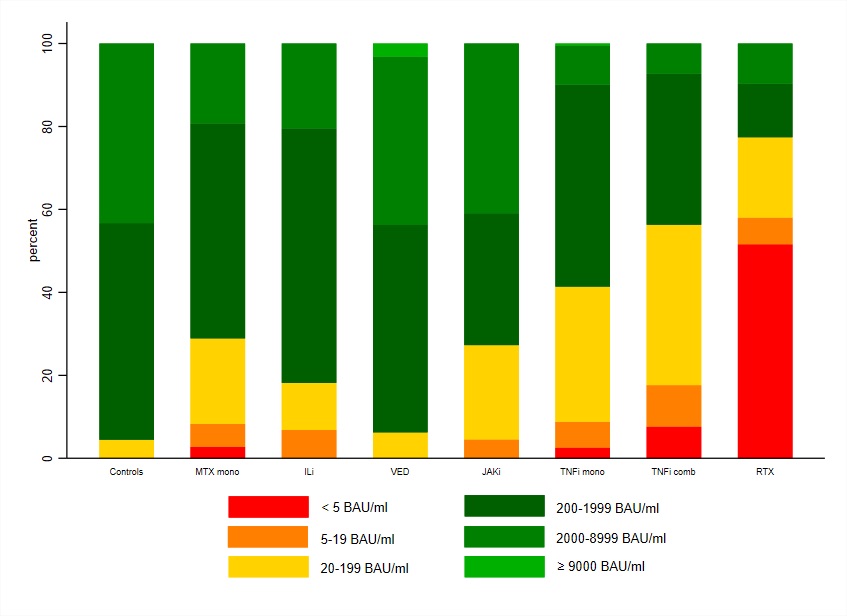 B)
B)
Disclosures: I. Christensen, None; I. Jyssum, None; A. Tveter, None; J. Sexton, None; S. Mjaaland, None; G. Kro, None; T. Kvien, None; D. Warren, None; J. Jahnsen, AbbVie/Abbott, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Janssen, Gilead, Pfizer, Roche, Sandoz, Takeda, Galapagos; L. Munthe, None; E. Haavardsholm, Pfizer, AbbVie, Eli Lilly, UCB, Boehringer-Ingelheim, Gilead; G. Grødeland, AstraZeneca, Sanofi, Bayer, ThermoFisher; K. Jørgensen, Roche, Bristol-Myers Squibb(BMS); S. Syversen, None; G. Goll, Galapagos, AbbVie/Abbott, Pfizer, UCB; S. Provan, None.
Background/Purpose: The durability of vaccine-induced humoral immunity against SARS-CoV-2 in patients with immune-mediated inflammatory diseases (IMIDs) on immunosuppressive therapy is not well characterized. The aim of this study was to compare the persistence of anti-Spike antibodies following two-dose SARS-CoV-2 vaccination between IMID patients and healthy controls, and to identify factors associated with antibody decline.
Methods: IMID patients on immunosuppressive medication enrolled in the prospective observational Nor-vaC study were included. Participants received two-dose SARS-CoV-2 vaccination. Serum collected at two time points following vaccination (first assessment within 6–48 days, second within 49–123 days) were analysed for antibodies binding the receptor-binding domain (RBD) of the SARS-CoV-2 Spike protein. Multivariable regression models estimated percent reduction in anti-RBD over 30 days and factors associated with reduction.
Results: A total of 1108 patients (403 rheumatoid arthritis, 195 psoriatic arthritis, 195 spondyloarthritis, 124 ulcerative colitis, 191 Crohn´s disease) and 134 controls provided blood samples within the defined intervals (median 19 days [IQR 15–24] and 97 days [87–105] after second vaccine dose). Antibody levels were lower in patients compared to controls at both time points, with median anti-RBD 2806 BAU/ml [IQR 1018–6068] in patients and 6187 BAU/ml [4105–7496] in controls (p< 0.001) at first assessment, and 608 BAU/ml [IQR 58–1053] in patients and 1520 BAU/ml [979–3766] in controls (p< 0.001) at second assessment. At second assessment, low anti-RBD antibody levels (defined as < 200 BAU/ml) were found in 449 (41%) patients, and 6 (5%) controls (p< 0.001). The change was -83% in patients and -66% in controls (p< 0.001). Patients had a greater estimated 30 days percent reduction in anti-RBD levels compared to controls -4.9 (95% CI -7.4 – -2.4), (p< 0.05). Among therapies, mono- or combination treatment with tumor necrosis factor inhibitors were associated with the greatest decline.
Conclusion: Within 4 months after vaccination, antibody levels declined considerably in both IMID patients and controls. Patients had lower initial antibody levels and a more pronounced decline compared to healthy controls, and were therefore more likely to decline to low antibody levels. These results support that additional vaccine doses may be of particular importance in IMID patients who may also need this at an earlier stage than healthy individuals.
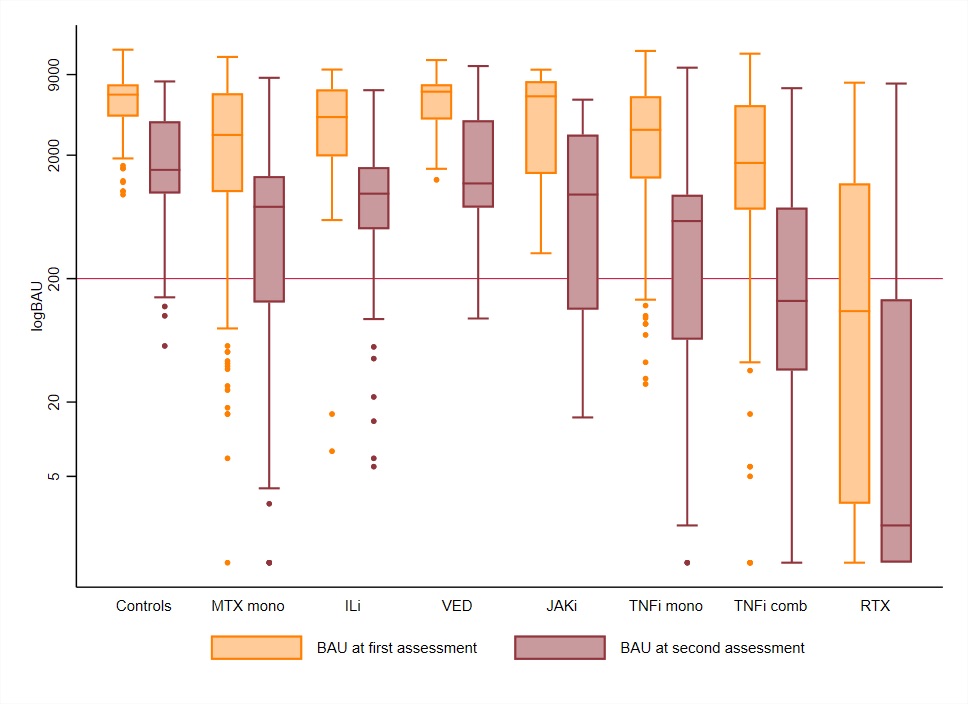 Figure 1. Levels of anti-RBD antibodies at first and second assessment according to medication groups
Figure 1. Levels of anti-RBD antibodies at first and second assessment according to medication groups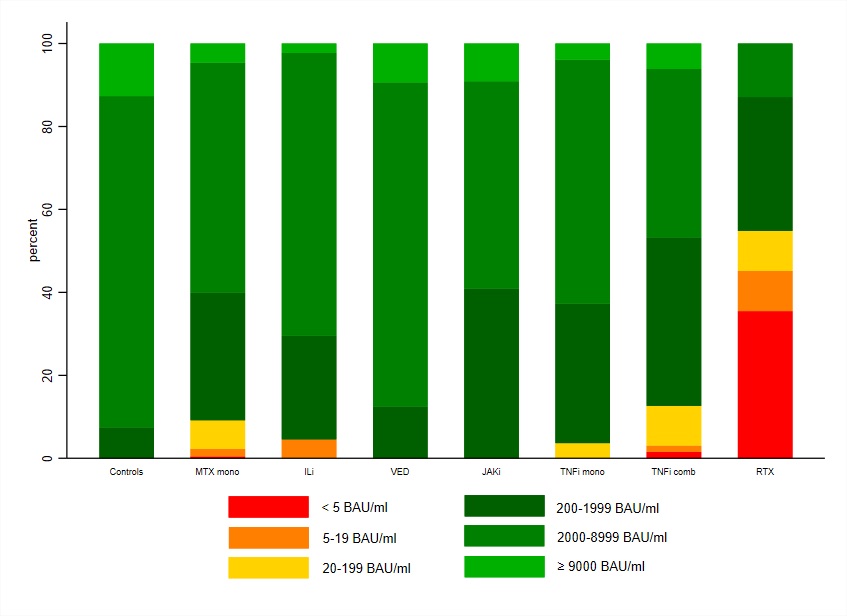 Figure 2. Percent distribution of anti-RBD levels at the first (A) and second (B) assessment in patients and healthy controls
Figure 2. Percent distribution of anti-RBD levels at the first (A) and second (B) assessment in patients and healthy controls A)
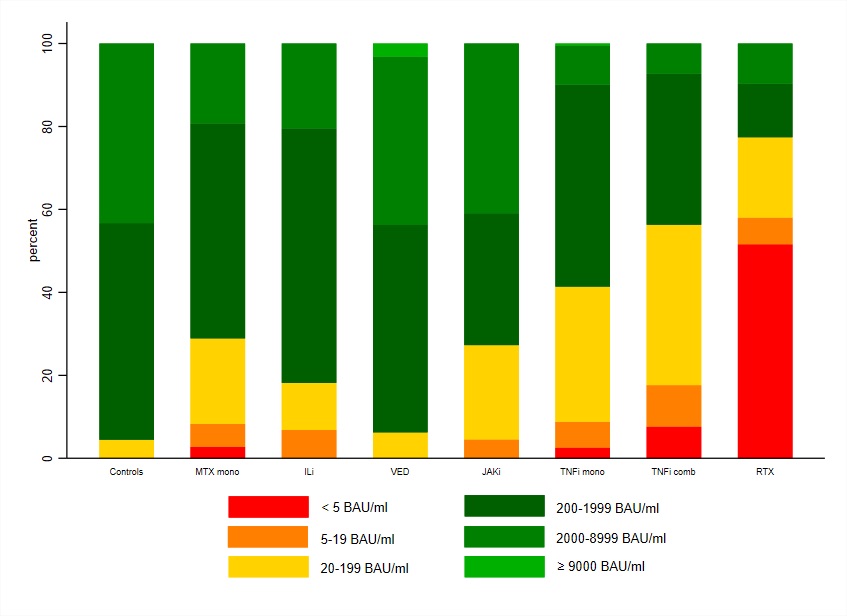 B)
B)Disclosures: I. Christensen, None; I. Jyssum, None; A. Tveter, None; J. Sexton, None; S. Mjaaland, None; G. Kro, None; T. Kvien, None; D. Warren, None; J. Jahnsen, AbbVie/Abbott, Boehringer-Ingelheim, Bristol-Myers Squibb(BMS), Janssen, Gilead, Pfizer, Roche, Sandoz, Takeda, Galapagos; L. Munthe, None; E. Haavardsholm, Pfizer, AbbVie, Eli Lilly, UCB, Boehringer-Ingelheim, Gilead; G. Grødeland, AstraZeneca, Sanofi, Bayer, ThermoFisher; K. Jørgensen, Roche, Bristol-Myers Squibb(BMS); S. Syversen, None; G. Goll, Galapagos, AbbVie/Abbott, Pfizer, UCB; S. Provan, None.

