Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0629–0670) SLE – Etiology and Pathogenesis Poster
0634: Total Interstitial Inflammation Predicts Chronic Kidney Disease Progression in Patients with Lupus Nephritis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- SW
Shudan Wang, MD, MS
Albert Einstein College of Medicine
New York, NY, United States
Abstract Poster Presenter(s)
Minh Dien Duong1, Shudan Wang2, Daniel Schwartz3, Wenzhu B. Mowrey4, Anna Broder5 and Beatrice Goilav6, 1The Children's Hospital of Montefiore / Albert Einstein College of Medicine, Bronx, NY, 2Montefiore Medical Center / Albert Einstein College of Medicine, New York, NY, 3Montefiore Medical Center / Albert Einstein College of Medicine, Bronx, NY, 4Albert Einstein College of Medicine, Bronx, NY, 5Hackensack University Medical Center, Hackensack, NJ, 6Children's Hospital of Montefiore / Albert Einstein College of Medicine, Bronx, NY
Background/Purpose: Kidney biopsy is a gold standard for diagnosis and prognostication of lupus nephritis (LN). While interstitial fibrosis and tubular atrophy (IFTA) predict progression to chronic kidney disease (CKD), current NIH classification of interstitial inflammation only assesses for inflammation in unscarred cortical parenchyma and is found not predictive of CKD progression. The objective of this study was to determine whether total interstitial inflammation that accounts for inflammation in the entire cortical parenchyma in areas with and without fibrosis could predict CKD progression in patients with LN. Early identification of at-risk patients and combination therapies may improve outcomes.
Methods: A retrospective cohort study included 125 SLE patients with LN class III, IV, V or mixed (III/V, IV/V) on the index biopsy (2005-2018). Renal biopsies were reviewed and assigned based on the 2018-NIH Activity Index/Chronicity Index, and tubulointerstitial lesion categories. Total interstitial inflammation in the entire cortical parenchyma (ti score) was graded as 0, 1, 2, and 3 corresponding to < 10%, 10-25%, 26-50%, and >50% of the total cortical parenchyma containing an inflammatory infiltrate (similar to the definition used in the Banff ti score). CKD progression was defined as an estimated glomerular filtration rate (eGFR) decline by ≥30% within 5 years post-index biopsy. Parallel time-dependent analyses were performed to determine whether the total intestinal inflammation score and NIH interstitial inflammation score predict CKD progression.
Results: Of 125 patients, 46 developed CKD progression. There were no differences in baseline characteristics between progressors and non-progressors (Table 1). Of these patients, 28 (22.4%) had moderate-to-severe total interstitial inflammation and 8 (6.4%) had moderate-to-severe NIH interstitial inflammation (Table 2). Total interstitial inflammation was associated with CKD progression in bivariate and time-dependent analyses [HR (95%CI): 2.76 (1.4-5.43) adjusted for age at biopsy, race and sex)]. NIH interstitial inflammation was not associated with CKD progression (Table 3).
Conclusion: Accounting for interstitial inflammation in the entire cortical parenchyma in areas with and without fibrosis identifies patients at risk for CKD progression.
.jpg) (*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (**) Low serum complements 3, and 4 are below 80, and 20 mg/dL, respectively. (***) Elevated anti-ds DNA antibody is above 70 IU.
(*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (**) Low serum complements 3, and 4 are below 80, and 20 mg/dL, respectively. (***) Elevated anti-ds DNA antibody is above 70 IU.
Abbreviations: CKD, chronic kidney disease; SLE, systemic lupus erythematosus; SLEDAI, SLE disease activity index; GN, glomerulonephritis; MMF, mycophenolate mofetil; ACE, angiotensin converting enzyme; ARBs, angiotensin receptor blockades.
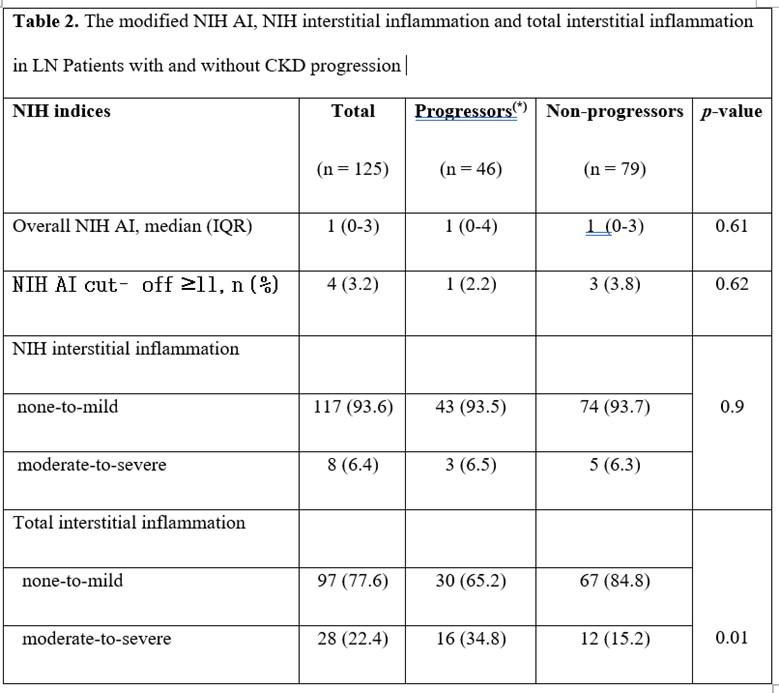 (*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy.
(*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy.
Abbreviations: NIH, National Institutes of Health; AI, activity index.
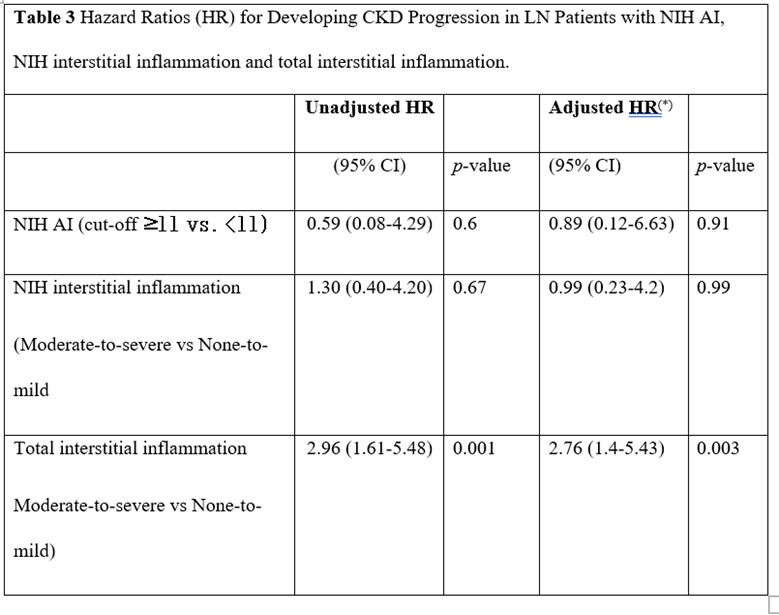 CKD progression was defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (*) Adjusted for age at kidney biopsy, sex, and race.
CKD progression was defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (*) Adjusted for age at kidney biopsy, sex, and race.
Disclosures: M. Duong, None; S. Wang, None; D. Schwartz, None; W. Mowrey, None; A. Broder, None; B. Goilav, None.
Background/Purpose: Kidney biopsy is a gold standard for diagnosis and prognostication of lupus nephritis (LN). While interstitial fibrosis and tubular atrophy (IFTA) predict progression to chronic kidney disease (CKD), current NIH classification of interstitial inflammation only assesses for inflammation in unscarred cortical parenchyma and is found not predictive of CKD progression. The objective of this study was to determine whether total interstitial inflammation that accounts for inflammation in the entire cortical parenchyma in areas with and without fibrosis could predict CKD progression in patients with LN. Early identification of at-risk patients and combination therapies may improve outcomes.
Methods: A retrospective cohort study included 125 SLE patients with LN class III, IV, V or mixed (III/V, IV/V) on the index biopsy (2005-2018). Renal biopsies were reviewed and assigned based on the 2018-NIH Activity Index/Chronicity Index, and tubulointerstitial lesion categories. Total interstitial inflammation in the entire cortical parenchyma (ti score) was graded as 0, 1, 2, and 3 corresponding to < 10%, 10-25%, 26-50%, and >50% of the total cortical parenchyma containing an inflammatory infiltrate (similar to the definition used in the Banff ti score). CKD progression was defined as an estimated glomerular filtration rate (eGFR) decline by ≥30% within 5 years post-index biopsy. Parallel time-dependent analyses were performed to determine whether the total intestinal inflammation score and NIH interstitial inflammation score predict CKD progression.
Results: Of 125 patients, 46 developed CKD progression. There were no differences in baseline characteristics between progressors and non-progressors (Table 1). Of these patients, 28 (22.4%) had moderate-to-severe total interstitial inflammation and 8 (6.4%) had moderate-to-severe NIH interstitial inflammation (Table 2). Total interstitial inflammation was associated with CKD progression in bivariate and time-dependent analyses [HR (95%CI): 2.76 (1.4-5.43) adjusted for age at biopsy, race and sex)]. NIH interstitial inflammation was not associated with CKD progression (Table 3).
Conclusion: Accounting for interstitial inflammation in the entire cortical parenchyma in areas with and without fibrosis identifies patients at risk for CKD progression.
.jpg) (*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (**) Low serum complements 3, and 4 are below 80, and 20 mg/dL, respectively. (***) Elevated anti-ds DNA antibody is above 70 IU.
(*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (**) Low serum complements 3, and 4 are below 80, and 20 mg/dL, respectively. (***) Elevated anti-ds DNA antibody is above 70 IU. Abbreviations: CKD, chronic kidney disease; SLE, systemic lupus erythematosus; SLEDAI, SLE disease activity index; GN, glomerulonephritis; MMF, mycophenolate mofetil; ACE, angiotensin converting enzyme; ARBs, angiotensin receptor blockades.
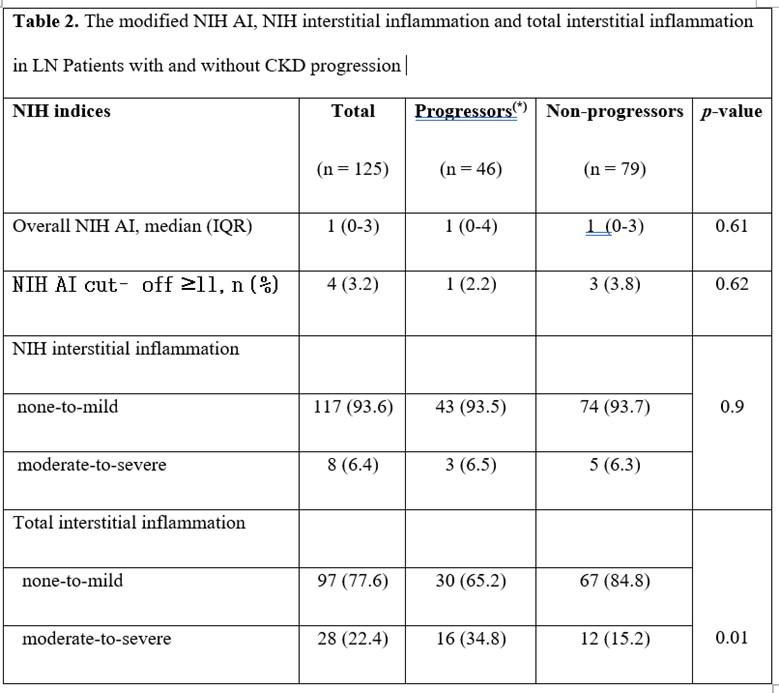 (*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy.
(*) CKD progressors were defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. Abbreviations: NIH, National Institutes of Health; AI, activity index.
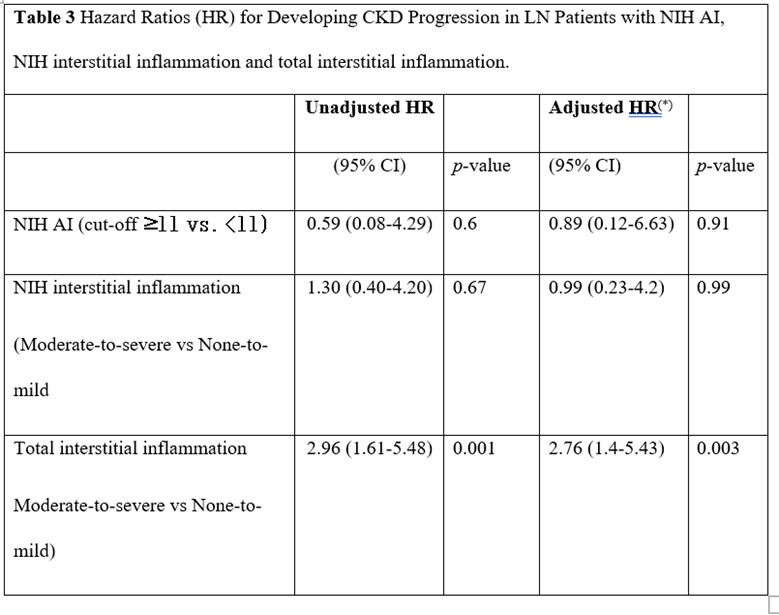 CKD progression was defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (*) Adjusted for age at kidney biopsy, sex, and race.
CKD progression was defined as LN patients with an eGFR decline of ≥30% within 5 years post-index biopsy. (*) Adjusted for age at kidney biopsy, sex, and race. Disclosures: M. Duong, None; S. Wang, None; D. Schwartz, None; W. Mowrey, None; A. Broder, None; B. Goilav, None.

