Back
Poster Session B
Epidemiology, health policy and outcomes
Session: (0724–0751) Health Services Research Poster II
0744: University of North Carolina and Piedmont Health Collaborative Tele-Rheumatology Project to Optimize Rural Health Specialty Access
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- LB
Leah Bettner, MD
University of North Carolina Hospital System
Chapel Hill, NC, United States
Abstract Poster Presenter(s)
Leah Bettner1, Eli Tiller2, John Doughton2, Rumey Ishizawar1 and Alfredo Rivadeneira1, 1University of North Carolina at Chapel Hill, Division of Rheumatology, Allergy and Immunology, Thurston Arthritis Research Center, Chapel Hill, NC, 2University of North Carolina Department of Family Medicine, Piedmont Health Services, Chapel Hill, NC
Background/Purpose: Telemedicine can offset barriers rural minority populations face for rheumatology care. However, implementing virtual health technology is challenging as broadband adoption is lower among rural residents, minority populations, and adults with low income and education attainment.1 With support from the Arthritis Foundation, this pilot project started in January 2022 utilizing telehealth visits between the University of North Carolina (UNC) Rheumatology Clinic and Piedmont Health Services (PHS), a federally qualified health center serving rural North Carolina (NC) patients. Our aims are to 1) improve rheumatology access for a racially/ethnically diverse and/or socioeconomically disadvantaged rural population, and 2) empower community providers to manage rheumatic disorders.
Methods: Patients were triaged to the program if there was 1) prior rheumatologic diagnoses with lost to rheumatology specialty care follow-up, 2) new rheumatic symptoms with transportation and/or financial barriers, and 3) established care directly to this tele-rheumatology program. Monthly clinic sessions were conducted via shared visits between the on-site PHS provider and patient with the virtually connected off-site UNC rheumatology attending and fellow. The PHS provider relayed objective data and conducted the physical exam with rheumatology guidance over video. The rheumatologists completed the medical history and provided recommendations. After each visit 5-point Likert surveys assessed patient satisfaction, PHS provider confidence and satisfaction, and UNC provider satisfaction. Patient surveys collected self-reported demographic data. Rheumatology attendings and fellows facilitated monthly virtual didactic sessions in an open-forum. After didactic sessions, 5-point Likert surveys assessed audience satisfaction.
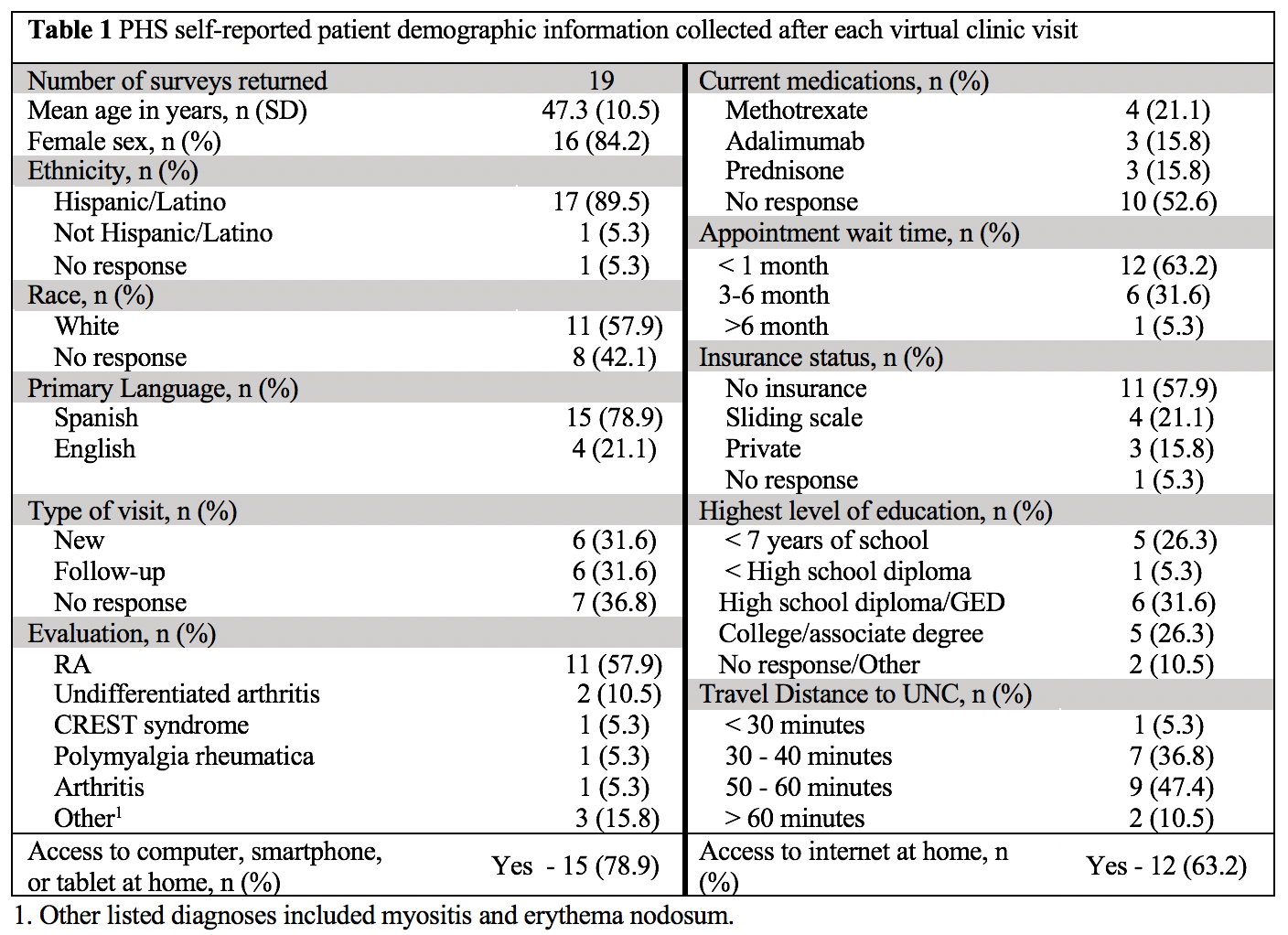
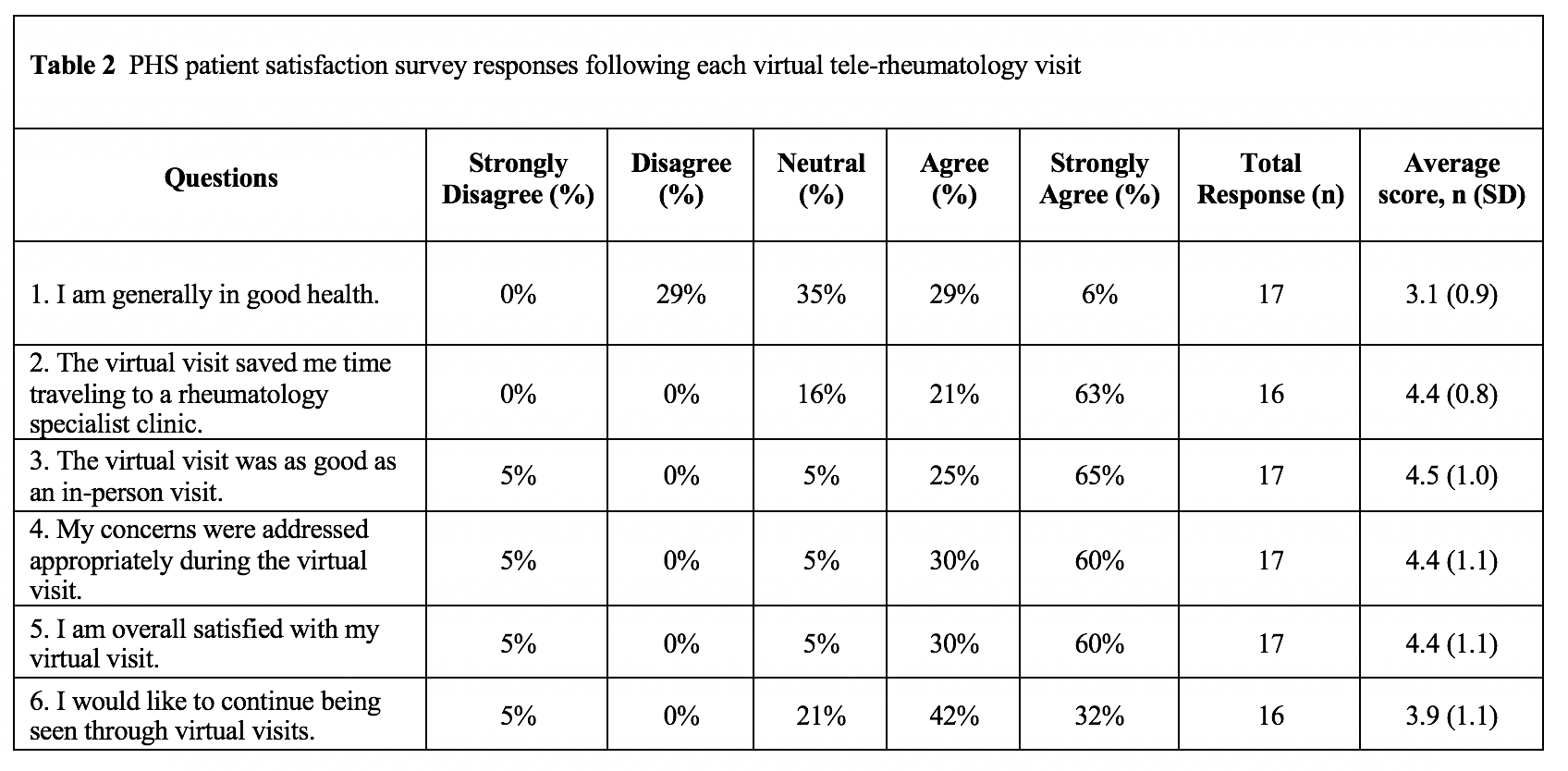
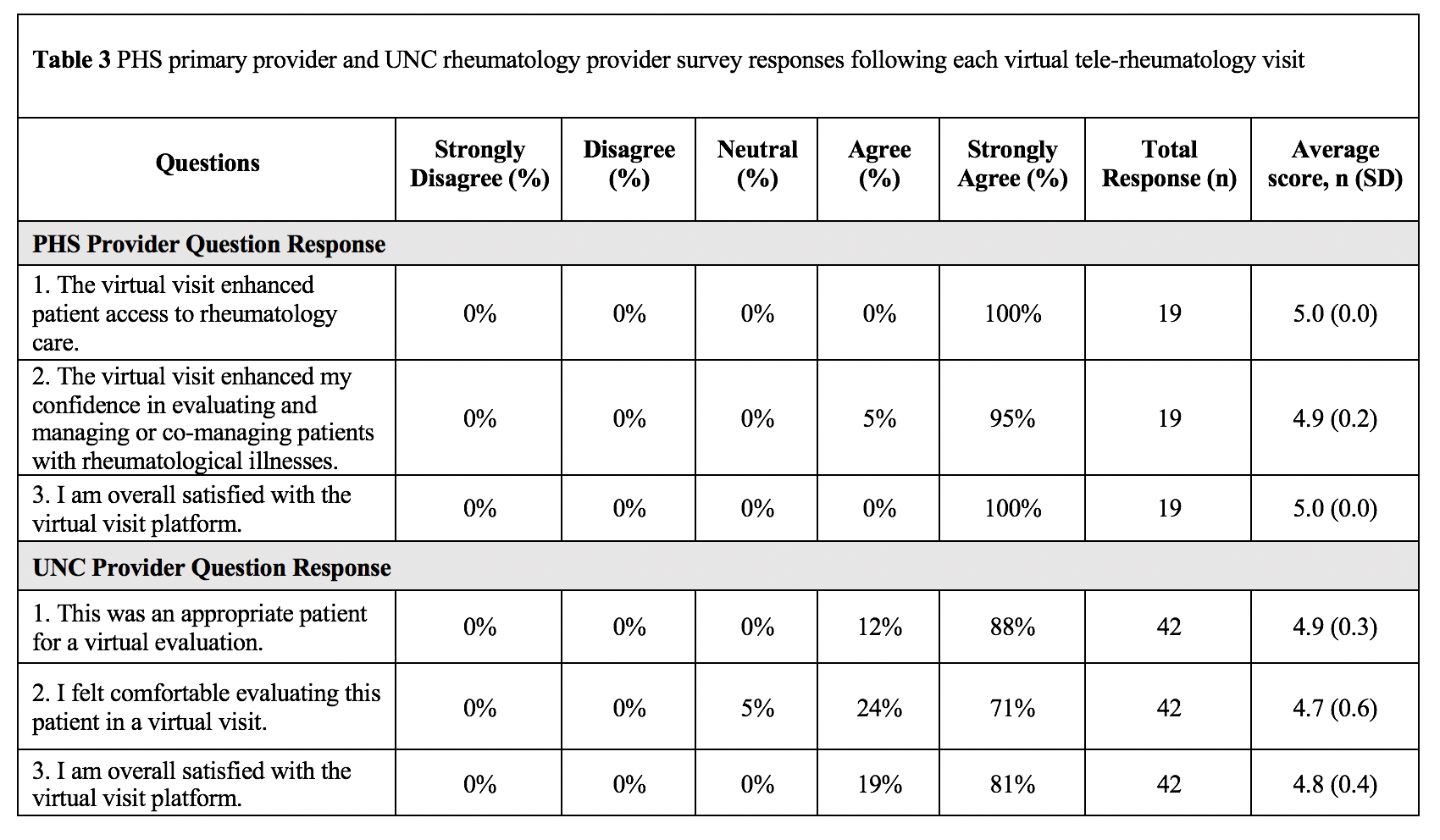
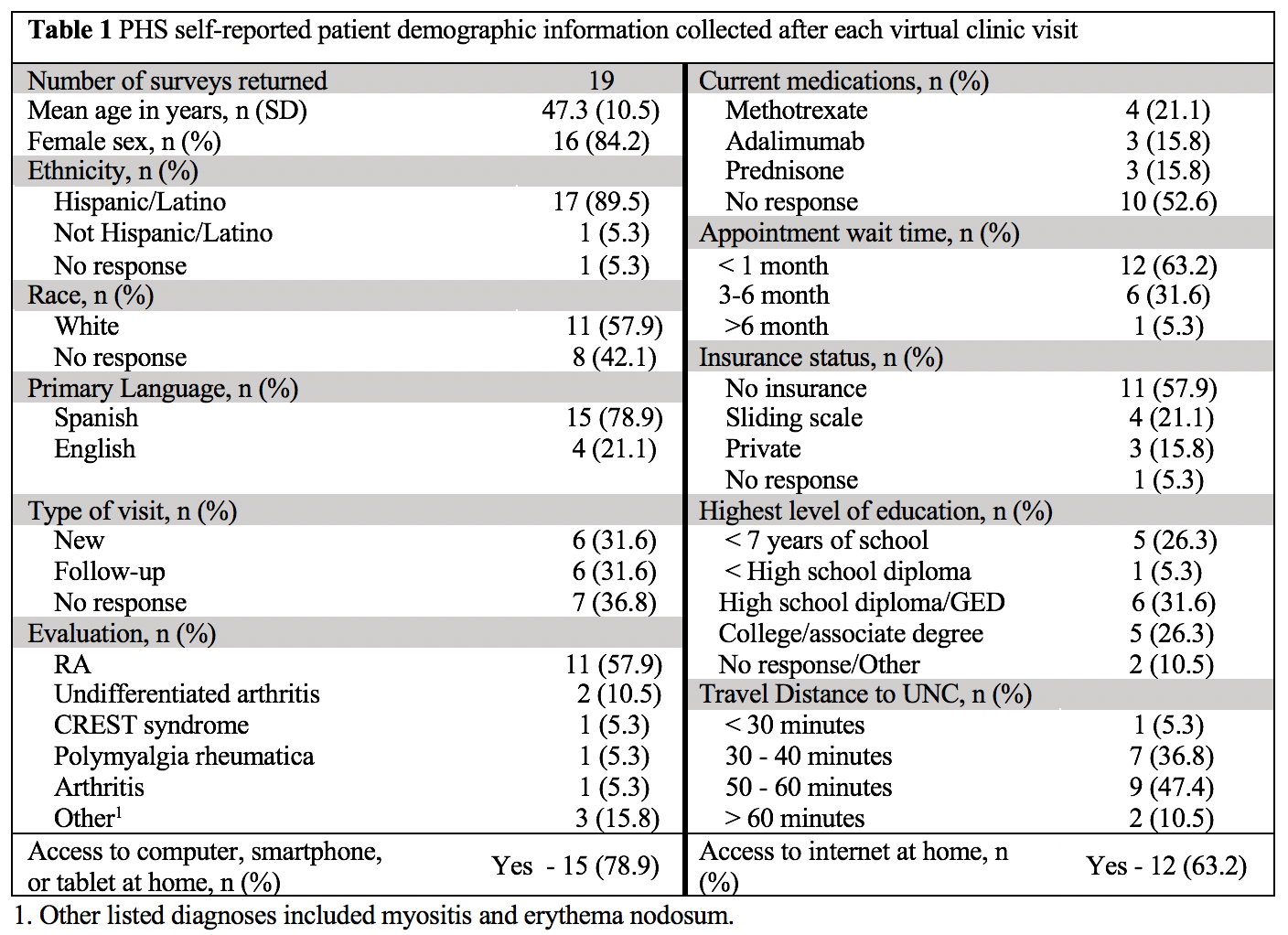
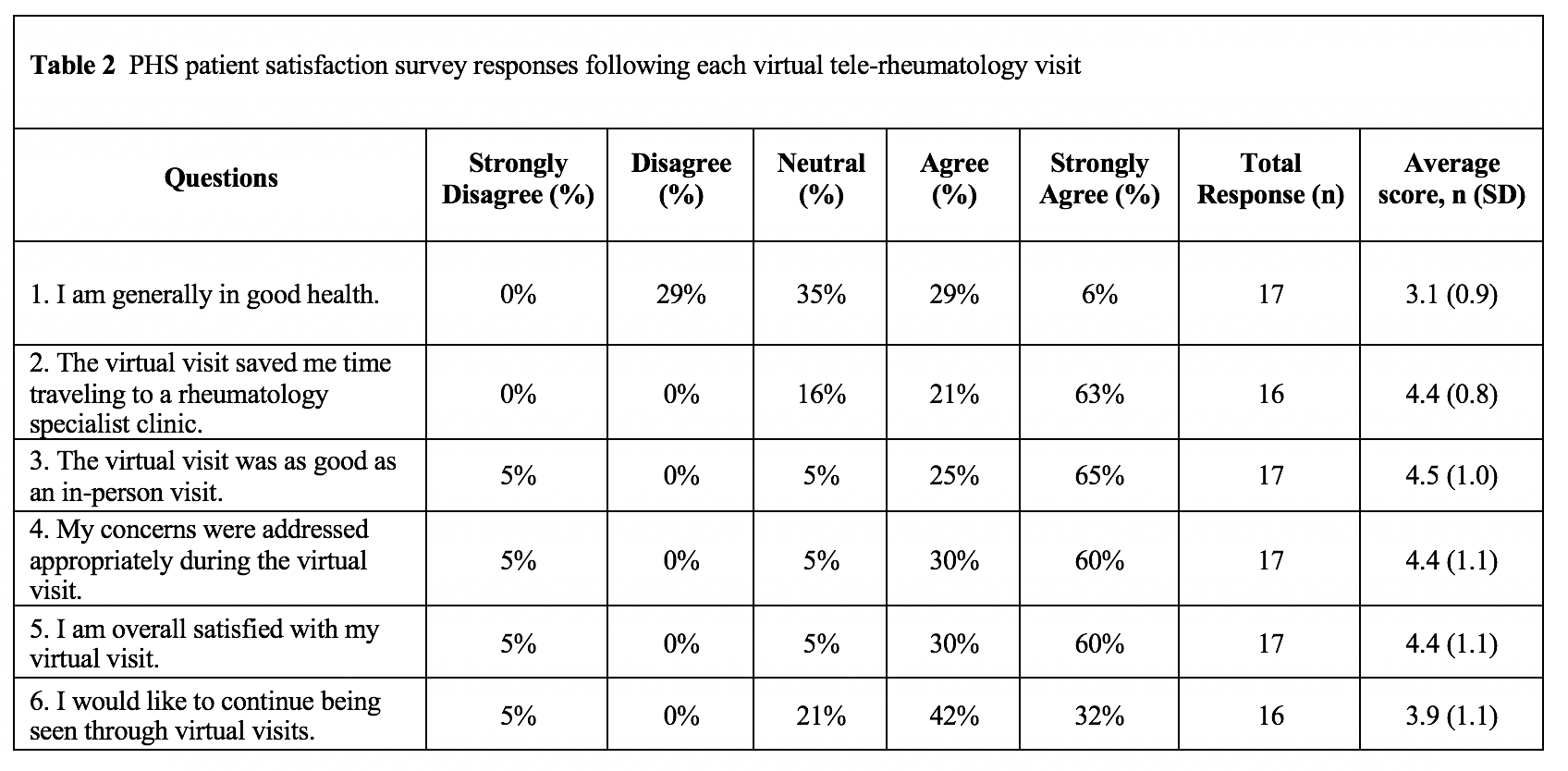
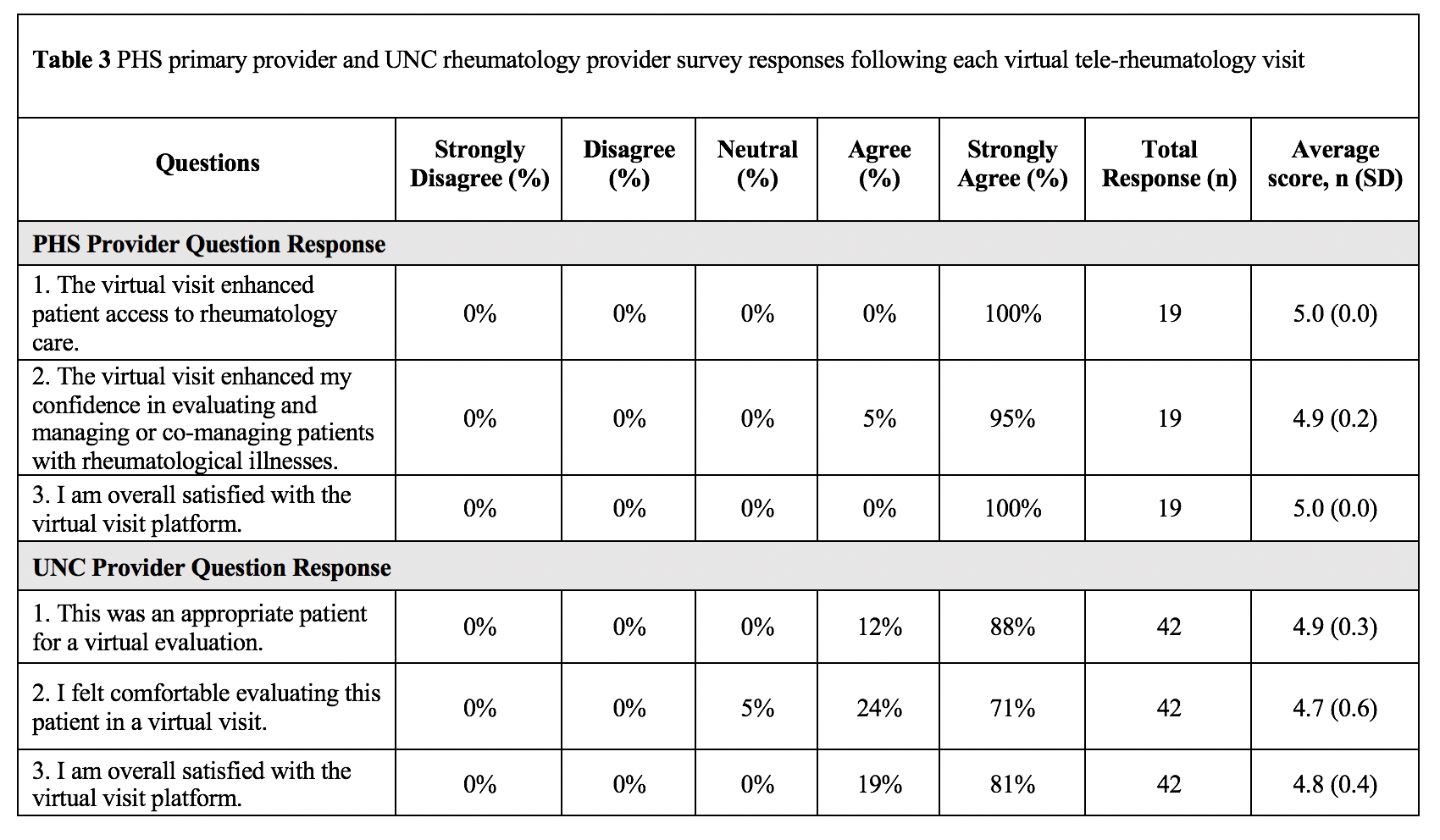
Results: Between January and April 2022, 23 patient encounters were completed. To date, 19 patient surveys were returned for analysis. Patients were self-reported as largely female, Hispanic, and Spanish-speaking. Evaluation for RA was commonly reported, and most patients were seen within 1 month (Table 1). Patients reported high satisfaction scores and noted the virtual platform saved them time traveling to UNC (Table 2). Post-visit PHS provider satisfaction and confidence scores and UNC provider satisfaction scores were high (Table 3). PHS provider responses to post-didactic surveys on the 5-point Likert scale were high ranging from 4.2-4.4.
Conclusion: This pilot supported by the Arthritis Foundation is a unique partnership in NC which expands rheumatology access to a rural minority population with high satisfaction scores reported in the first quarter. Our collaborative tele-rheumatology model allows for timely specialty care and alleviates barriers relating to transportation, insurance coverage, and broadband access. In addition, focused didactic sessions and shared care visits engage and empower rural community primary care providers to manage common rheumatic diseases. We are operating in 2 of the 12 PHS sites and envision the program expanding to other rural NC sites.
1. Anderson, Monica, et al. "10% of Americans don't use the internet. Who are they?." (2019).
Disclosures: L. Bettner, None; E. Tiller, None; J. Doughton, None; R. Ishizawar, None; A. Rivadeneira, None.
Background/Purpose: Telemedicine can offset barriers rural minority populations face for rheumatology care. However, implementing virtual health technology is challenging as broadband adoption is lower among rural residents, minority populations, and adults with low income and education attainment.1 With support from the Arthritis Foundation, this pilot project started in January 2022 utilizing telehealth visits between the University of North Carolina (UNC) Rheumatology Clinic and Piedmont Health Services (PHS), a federally qualified health center serving rural North Carolina (NC) patients. Our aims are to 1) improve rheumatology access for a racially/ethnically diverse and/or socioeconomically disadvantaged rural population, and 2) empower community providers to manage rheumatic disorders.
Methods: Patients were triaged to the program if there was 1) prior rheumatologic diagnoses with lost to rheumatology specialty care follow-up, 2) new rheumatic symptoms with transportation and/or financial barriers, and 3) established care directly to this tele-rheumatology program. Monthly clinic sessions were conducted via shared visits between the on-site PHS provider and patient with the virtually connected off-site UNC rheumatology attending and fellow. The PHS provider relayed objective data and conducted the physical exam with rheumatology guidance over video. The rheumatologists completed the medical history and provided recommendations. After each visit 5-point Likert surveys assessed patient satisfaction, PHS provider confidence and satisfaction, and UNC provider satisfaction. Patient surveys collected self-reported demographic data. Rheumatology attendings and fellows facilitated monthly virtual didactic sessions in an open-forum. After didactic sessions, 5-point Likert surveys assessed audience satisfaction.
Results: Between January and April 2022, 23 patient encounters were completed. To date, 19 patient surveys were returned for analysis. Patients were self-reported as largely female, Hispanic, and Spanish-speaking. Evaluation for RA was commonly reported, and most patients were seen within 1 month (Table 1). Patients reported high satisfaction scores and noted the virtual platform saved them time traveling to UNC (Table 2). Post-visit PHS provider satisfaction and confidence scores and UNC provider satisfaction scores were high (Table 3). PHS provider responses to post-didactic surveys on the 5-point Likert scale were high ranging from 4.2-4.4.
Conclusion: This pilot supported by the Arthritis Foundation is a unique partnership in NC which expands rheumatology access to a rural minority population with high satisfaction scores reported in the first quarter. Our collaborative tele-rheumatology model allows for timely specialty care and alleviates barriers relating to transportation, insurance coverage, and broadband access. In addition, focused didactic sessions and shared care visits engage and empower rural community primary care providers to manage common rheumatic diseases. We are operating in 2 of the 12 PHS sites and envision the program expanding to other rural NC sites.
1. Anderson, Monica, et al. "10% of Americans don't use the internet. Who are they?." (2019).
Disclosures: L. Bettner, None; E. Tiller, None; J. Doughton, None; R. Ishizawar, None; A. Rivadeneira, None.

