Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1256: A Machine Learning Pipeline for Prediction of Bone Marrow Oedema Along the Sacroiliac Joints on Magnetic Resonance Imaging
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AD
Ann-Sophie De Craemer, MD
Ghent University Hospital
Gent, Belgium
Abstract Poster Presenter(s)
Joris Roels1, Ann-Sophie Kathleen De Craemer2, Thomas Renson3, Manouk de Hooge4, Arne Gevaert1, Lennart Jans3, Nele Herregods3, Thomas Van Den Berghe3, Philippe Carron3, Filip Van den bosch5, Yvan Saeys1 and Dirk Elewaut6, 1Center for Inflammation Research, UGent-VIB, Ghent, Belgium, 2Ghent University Hospital, Gent, Belgium, 3Ghent University Hospital, Ghent, Belgium, 4Ghent University Hospital, Luxembourg, Luxembourg, 5Department of Internal Medicine and Paediatrics, Ghent University and VIB Centre for Inflammation Research, Ghent, Belgium, 6Department of Rheumatology, Ghent University Hospital, Belgium, VIB-UGent Center for Inflammation Research, Ghent University, Heusden, Belgium
Background/Purpose: Detection and semi-quantitative assessment of bone marrow oedema (BMO) on magnetic resonance imaging (MRI) of the sacroiliac (SI) joints is essential for the diagnosis and follow-up of spondyloarthritis (SpA) patients. A machine learning (ML) algorithm could address intra- and inter-reader variability and the time-consuming nature of these assessments.
Methods: We developed a deep learning workflow that automatically locates the SI joints, segments regions of interest (ilium and sacrum), performs quadrant extraction and predicts presence of BMO, suggestive of inflammatory lesions, on a quadrant-level in semi-coronal slices of T1/T2 weighted MRI scans (Figure 1). Using a ResNet18 backbone, the inflammation classifier was trained and tested (5-fold cross-validation) on scans of SpA patients (n=279), postpartum women (n=71), and healthy individuals (n=114); while 243 SpA MRIs served as external validation. Patient-level predictions were derived from aggregating quadrant-level predictions, i.e. at least one positive quadrant.
Results: The proposed method automatically detects the SI joints and segments the ilium and sacrum. An area under the receiver operating characteristics curve (ROC AUC) score of 94.7%, balanced accuracy (B-ACC) of 82.2% and an F1 score of 62.1% is reported for the proposed inflammation prediction algorithm in cross validation. In the external validation dataset, ROC AUC was 88.2%, B-ACC 72.1% and F1 score 50.8%. On a patient-level, the model achieved an accuracy of 81.6% and 81.4% in the cross validation and external validation dataset, respectively.
Conclusion: We propose a fully automated ML pipeline for detection of BMO on MRI of the SI joints that has the potential to assist clinicians in early diagnosis and reliable quantification of inflammatory lesions in patients with (suspected) SpA.
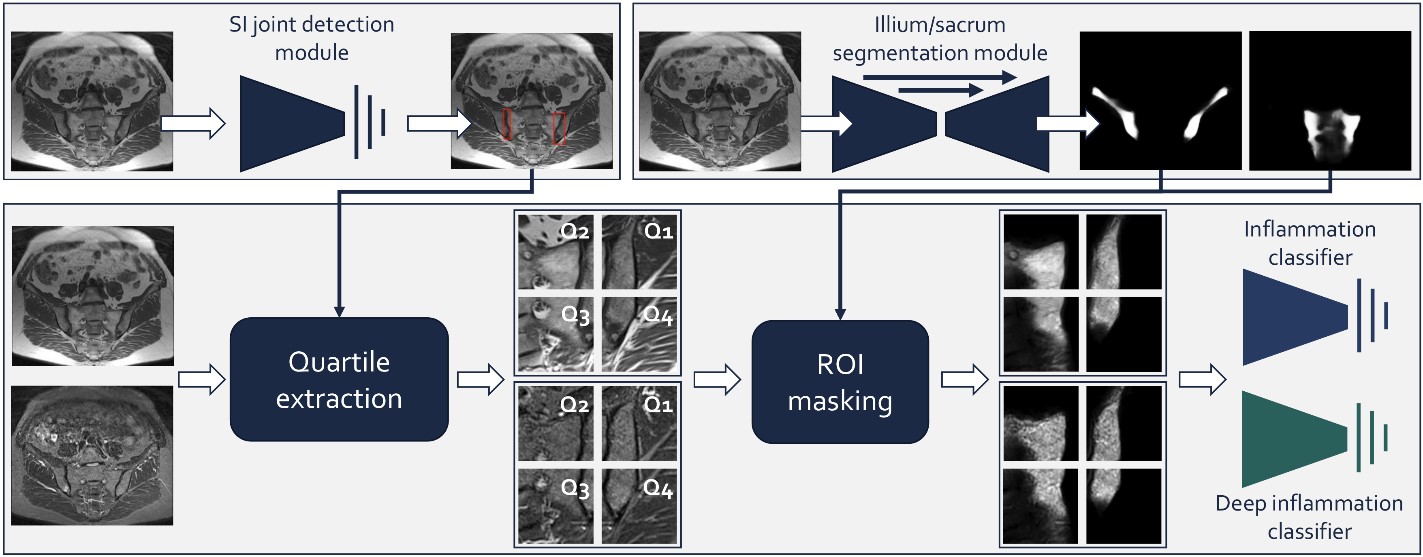 Figure 1: Proposed pipeline for automated scoring of the MRI data. The T1-weightes sequence is used for locating the SI joints and segmentation of the ilium/sacrum. Based on this, the SI regions of interest (ROI) are extracted, and (optionally) masked with the ilium/sacrum segments. These ROIs are then fed to a convolutional neural network to predict presence of (deep) inflammatory lesions.
Figure 1: Proposed pipeline for automated scoring of the MRI data. The T1-weightes sequence is used for locating the SI joints and segmentation of the ilium/sacrum. Based on this, the SI regions of interest (ROI) are extracted, and (optionally) masked with the ilium/sacrum segments. These ROIs are then fed to a convolutional neural network to predict presence of (deep) inflammatory lesions.
Disclosures: J. Roels, None; A. De Craemer, None; T. Renson, None; M. de Hooge, None; A. Gevaert, None; L. Jans, None; N. Herregods, None; T. Van Den Berghe, None; P. Carron, Biogen, AbbVie/Abbott, Eli Lilly, Fresenius Kabi, Galapagos, Merck/MSD, Pfizer, Sanofi, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; Y. Saeys, None; D. Elewaut, AbbVie, Eli Lilly, Galapagos, Novartis, UCB Pharma.
Background/Purpose: Detection and semi-quantitative assessment of bone marrow oedema (BMO) on magnetic resonance imaging (MRI) of the sacroiliac (SI) joints is essential for the diagnosis and follow-up of spondyloarthritis (SpA) patients. A machine learning (ML) algorithm could address intra- and inter-reader variability and the time-consuming nature of these assessments.
Methods: We developed a deep learning workflow that automatically locates the SI joints, segments regions of interest (ilium and sacrum), performs quadrant extraction and predicts presence of BMO, suggestive of inflammatory lesions, on a quadrant-level in semi-coronal slices of T1/T2 weighted MRI scans (Figure 1). Using a ResNet18 backbone, the inflammation classifier was trained and tested (5-fold cross-validation) on scans of SpA patients (n=279), postpartum women (n=71), and healthy individuals (n=114); while 243 SpA MRIs served as external validation. Patient-level predictions were derived from aggregating quadrant-level predictions, i.e. at least one positive quadrant.
Results: The proposed method automatically detects the SI joints and segments the ilium and sacrum. An area under the receiver operating characteristics curve (ROC AUC) score of 94.7%, balanced accuracy (B-ACC) of 82.2% and an F1 score of 62.1% is reported for the proposed inflammation prediction algorithm in cross validation. In the external validation dataset, ROC AUC was 88.2%, B-ACC 72.1% and F1 score 50.8%. On a patient-level, the model achieved an accuracy of 81.6% and 81.4% in the cross validation and external validation dataset, respectively.
Conclusion: We propose a fully automated ML pipeline for detection of BMO on MRI of the SI joints that has the potential to assist clinicians in early diagnosis and reliable quantification of inflammatory lesions in patients with (suspected) SpA.
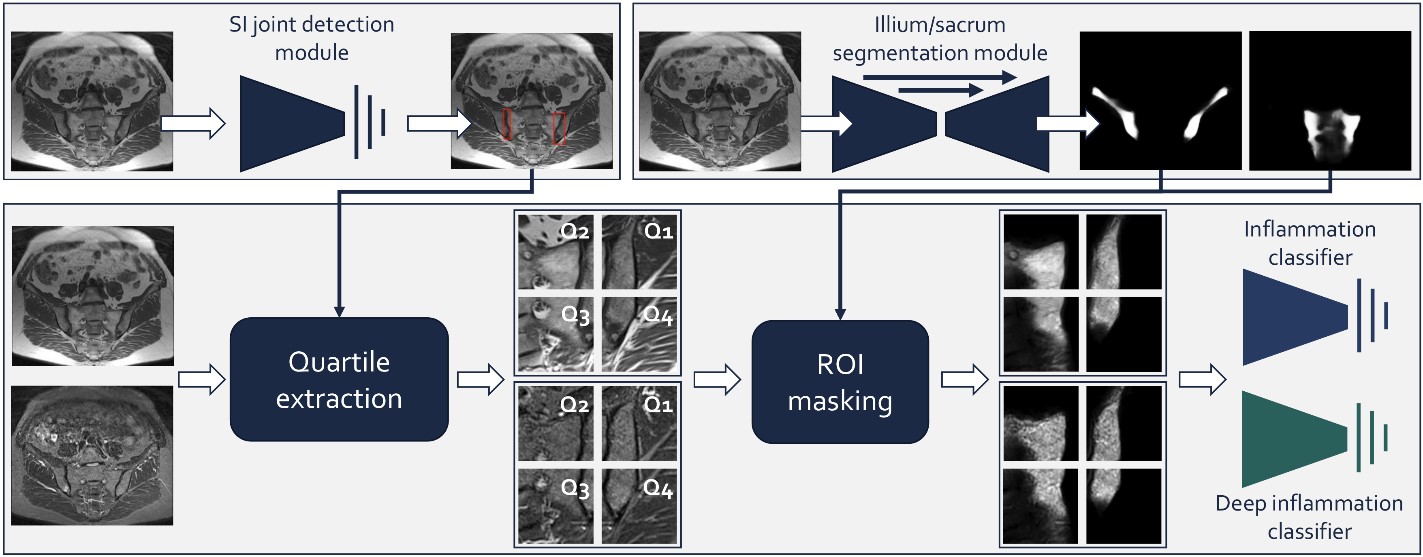 Figure 1: Proposed pipeline for automated scoring of the MRI data. The T1-weightes sequence is used for locating the SI joints and segmentation of the ilium/sacrum. Based on this, the SI regions of interest (ROI) are extracted, and (optionally) masked with the ilium/sacrum segments. These ROIs are then fed to a convolutional neural network to predict presence of (deep) inflammatory lesions.
Figure 1: Proposed pipeline for automated scoring of the MRI data. The T1-weightes sequence is used for locating the SI joints and segmentation of the ilium/sacrum. Based on this, the SI regions of interest (ROI) are extracted, and (optionally) masked with the ilium/sacrum segments. These ROIs are then fed to a convolutional neural network to predict presence of (deep) inflammatory lesions. Disclosures: J. Roels, None; A. De Craemer, None; T. Renson, None; M. de Hooge, None; A. Gevaert, None; L. Jans, None; N. Herregods, None; T. Van Den Berghe, None; P. Carron, Biogen, AbbVie/Abbott, Eli Lilly, Fresenius Kabi, Galapagos, Merck/MSD, Pfizer, Sanofi, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; Y. Saeys, None; D. Elewaut, AbbVie, Eli Lilly, Galapagos, Novartis, UCB Pharma.

