Back
Poster Session C
Pain syndromes, fibromyalgia and regional musculoskeletal disorders
Session: (1215–1227) Fibromyalgia and Other Clinical Pain Syndromes Poster
1224: ‘No Route Map’: The Complex Healthcare Journeys of People with Fibromyalgia – a Record Linkage Study in the UK
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- RH
Rosemary Hollick, PhD, BSc, FRCP, MBChB
University of Aberdeen
Aberdeen, United Kingdom
Abstract Poster Presenter(s)
Rosemary Hollick, Ka-Kin Lam, Marcus Beasley, Gareth Jones, Corri Black and Gary Macfarlane, University of Aberdeen, Aberdeen, Scotland, United Kingdom
Background/Purpose: Healthcare services for persons with fibromyalgia (FM) lack co-ordination. Patients describe feeling 'invisible' within healthcare systems and often report poor experiences of care, particularly after diagnosis. As part of a program to design improved care models for people with FM within the UK National Health Service, we explored survey respondents' secondary healthcare referral history. Specifically, we aimed to determine incidence of outpatient visits to different specialties, and frequency and direction of "transition" from one specialty to another, before and after diagnosis.
Methods: A previous study mailed questionnaires to adults registered at 16 GP practices in Scotland. Respondents reporting FM features were re-surveyed in 2019 and asked if they had ever received a FM diagnosis, and if so, in what year. Outpatient secondary care attendance records for these patients were available from the population-based Scottish hospital registry for 2006 through 2019. Proportion of FM patients visiting each specialty in this period was calculated. Average number of annual specialty visits per person was calculated for FM patients, before and after diagnosis, and compared with respondents meeting criteria for FM but with no diagnosis. Incidence rates per 1000 person-years pre- and post-diagnosis were computed. Frequency of repeat consultations, and transition between specialties (i.e., when referral to Specialty A is followed by referral to Specialty B) was recorded and the proportion of patients having each transition calculated for 5 years pre- and post-diagnosis.
Results: 72 patients with a FM diagnosis were included (61 female, mean age 57 years). The most visited specialties were General Surgery, Trauma & Orthopaedic Surgery, Rheumatology, Neurology, and Gynaecology (Table 1). The average number of annual specialty visits per person in those with FM was 1.4 before and 1.0 after diagnosis, and 1.1 in those who met criteria but without a diagnosis. Specialties most visited immediately before diagnosis (i.e. highest incidence rate of last visit pre-diagnosis) were Rheumatology and Trauma & Orthopaedic Surgery (89.8 and 81.1 visits per 1000 person-years) (Fig. 1). Pre-diagnosis, repeat visits to Trauma & Orthopaedics were common (22.2%). Specialties most visited immediately post-diagnosis were General Surgery, Gynaecology, and Pain Management (87.1, 86.9, and 60.0 visits per 1000 person-years). Post-diagnosis, patients visited many different clinics, with repeat visits to Pain Management just as common as those to Gastroenterology or General Surgery (11.4%).
Conclusion: We have illustrated complex healthcare journeys of FM patients. Pre-diagnostic journeys often end with visits to Rheumatology. Referrals post-diagnosis are also common, particularly to Gynaecology and General Surgery. There is a need for clear care pathways to; enable general practitioners to make a timely diagnosis, reduce unnecessary referrals, raise awareness among commonly visited specialties, and provide guidance on when to refer to services such as rheumatology in case of diagnostic uncertainty. This provides a basis from which to assess service change and design services which focus on support for pain management.
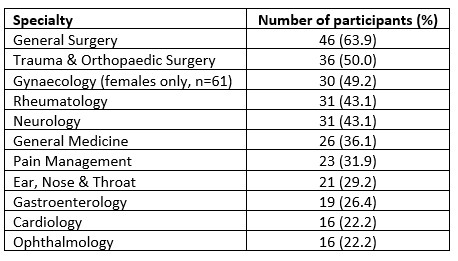 Table 1: Specialty referral in patients with an FM diagnosis in the period 2006 to 2019 (n=72)
Table 1: Specialty referral in patients with an FM diagnosis in the period 2006 to 2019 (n=72)
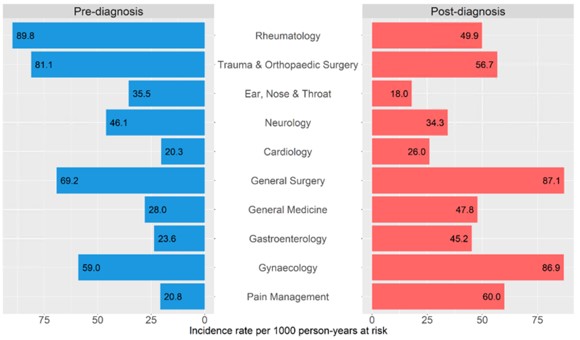 Figure 1: Specialty incidence rate per 1000 person-years at risk immediately pre- and post-diagnosis date
Figure 1: Specialty incidence rate per 1000 person-years at risk immediately pre- and post-diagnosis date
Disclosures: R. Hollick, None; K. Lam, None; M. Beasley, None; G. Jones, AbbVie/Abbott, Pfizer, UCB, Amgen, GlaxoSmithKlein(GSK), Janssen; C. Black, None; G. Macfarlane, AbbVie/Abbott, Pfizer, UCB, Amgen, GlaxoSmithKlein(GSK).
Background/Purpose: Healthcare services for persons with fibromyalgia (FM) lack co-ordination. Patients describe feeling 'invisible' within healthcare systems and often report poor experiences of care, particularly after diagnosis. As part of a program to design improved care models for people with FM within the UK National Health Service, we explored survey respondents' secondary healthcare referral history. Specifically, we aimed to determine incidence of outpatient visits to different specialties, and frequency and direction of "transition" from one specialty to another, before and after diagnosis.
Methods: A previous study mailed questionnaires to adults registered at 16 GP practices in Scotland. Respondents reporting FM features were re-surveyed in 2019 and asked if they had ever received a FM diagnosis, and if so, in what year. Outpatient secondary care attendance records for these patients were available from the population-based Scottish hospital registry for 2006 through 2019. Proportion of FM patients visiting each specialty in this period was calculated. Average number of annual specialty visits per person was calculated for FM patients, before and after diagnosis, and compared with respondents meeting criteria for FM but with no diagnosis. Incidence rates per 1000 person-years pre- and post-diagnosis were computed. Frequency of repeat consultations, and transition between specialties (i.e., when referral to Specialty A is followed by referral to Specialty B) was recorded and the proportion of patients having each transition calculated for 5 years pre- and post-diagnosis.
Results: 72 patients with a FM diagnosis were included (61 female, mean age 57 years). The most visited specialties were General Surgery, Trauma & Orthopaedic Surgery, Rheumatology, Neurology, and Gynaecology (Table 1). The average number of annual specialty visits per person in those with FM was 1.4 before and 1.0 after diagnosis, and 1.1 in those who met criteria but without a diagnosis. Specialties most visited immediately before diagnosis (i.e. highest incidence rate of last visit pre-diagnosis) were Rheumatology and Trauma & Orthopaedic Surgery (89.8 and 81.1 visits per 1000 person-years) (Fig. 1). Pre-diagnosis, repeat visits to Trauma & Orthopaedics were common (22.2%). Specialties most visited immediately post-diagnosis were General Surgery, Gynaecology, and Pain Management (87.1, 86.9, and 60.0 visits per 1000 person-years). Post-diagnosis, patients visited many different clinics, with repeat visits to Pain Management just as common as those to Gastroenterology or General Surgery (11.4%).
Conclusion: We have illustrated complex healthcare journeys of FM patients. Pre-diagnostic journeys often end with visits to Rheumatology. Referrals post-diagnosis are also common, particularly to Gynaecology and General Surgery. There is a need for clear care pathways to; enable general practitioners to make a timely diagnosis, reduce unnecessary referrals, raise awareness among commonly visited specialties, and provide guidance on when to refer to services such as rheumatology in case of diagnostic uncertainty. This provides a basis from which to assess service change and design services which focus on support for pain management.
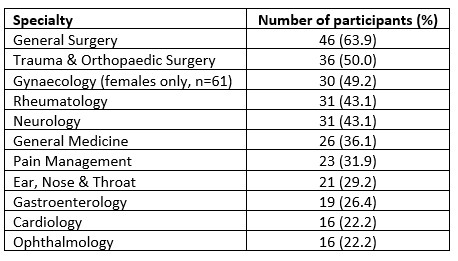 Table 1: Specialty referral in patients with an FM diagnosis in the period 2006 to 2019 (n=72)
Table 1: Specialty referral in patients with an FM diagnosis in the period 2006 to 2019 (n=72)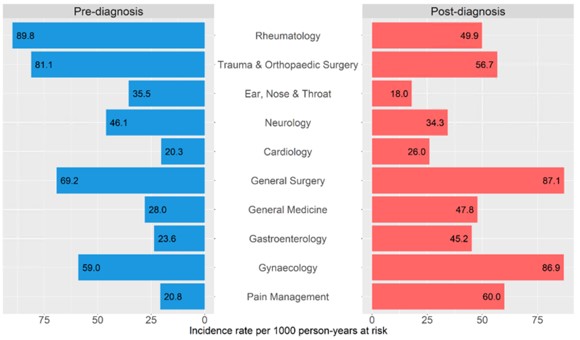 Figure 1: Specialty incidence rate per 1000 person-years at risk immediately pre- and post-diagnosis date
Figure 1: Specialty incidence rate per 1000 person-years at risk immediately pre- and post-diagnosis dateDisclosures: R. Hollick, None; K. Lam, None; M. Beasley, None; G. Jones, AbbVie/Abbott, Pfizer, UCB, Amgen, GlaxoSmithKlein(GSK), Janssen; C. Black, None; G. Macfarlane, AbbVie/Abbott, Pfizer, UCB, Amgen, GlaxoSmithKlein(GSK).

