Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1192: Celiac Disease in Patients with Systemic Lupus Erythematosus: An Analysis of Nationwide Inpatient Sample
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JZ
Jiayi Zheng, MD
The Wright Center for Graduate Medical Education
Scranton, PA, United States
Abstract Poster Presenter(s)
Jiayi Zheng1, Ruoning Ni2, Guangchen Zou3, Yuhao Zeng4, Naeem ijaz1 and Yani Zhang5, 1The Wright Center for Graduate Medical Education, Scranton, PA, 2Ascension Saint Agnes Hospital, Iowa City, IA, 3Danbury Hospital, Danbury, CT, 4Cleveland Clinic Akron General, Akron, OH, 5MedStar Union Memorial Hospital, Baltimore, MD
Background/Purpose: Celiac disease is an autoimmune disease characterized by the immunologic reaction to gluten by lymphocytes. Although recent studies suggest an association between celiac disease and other autoimmune diseases, its relationship with systemic lupus erythematosus (SLE) remains to be elucidated. In this study, we aimed to determine the prevalence of celiac disease in patients with SLE using a US-based national database.
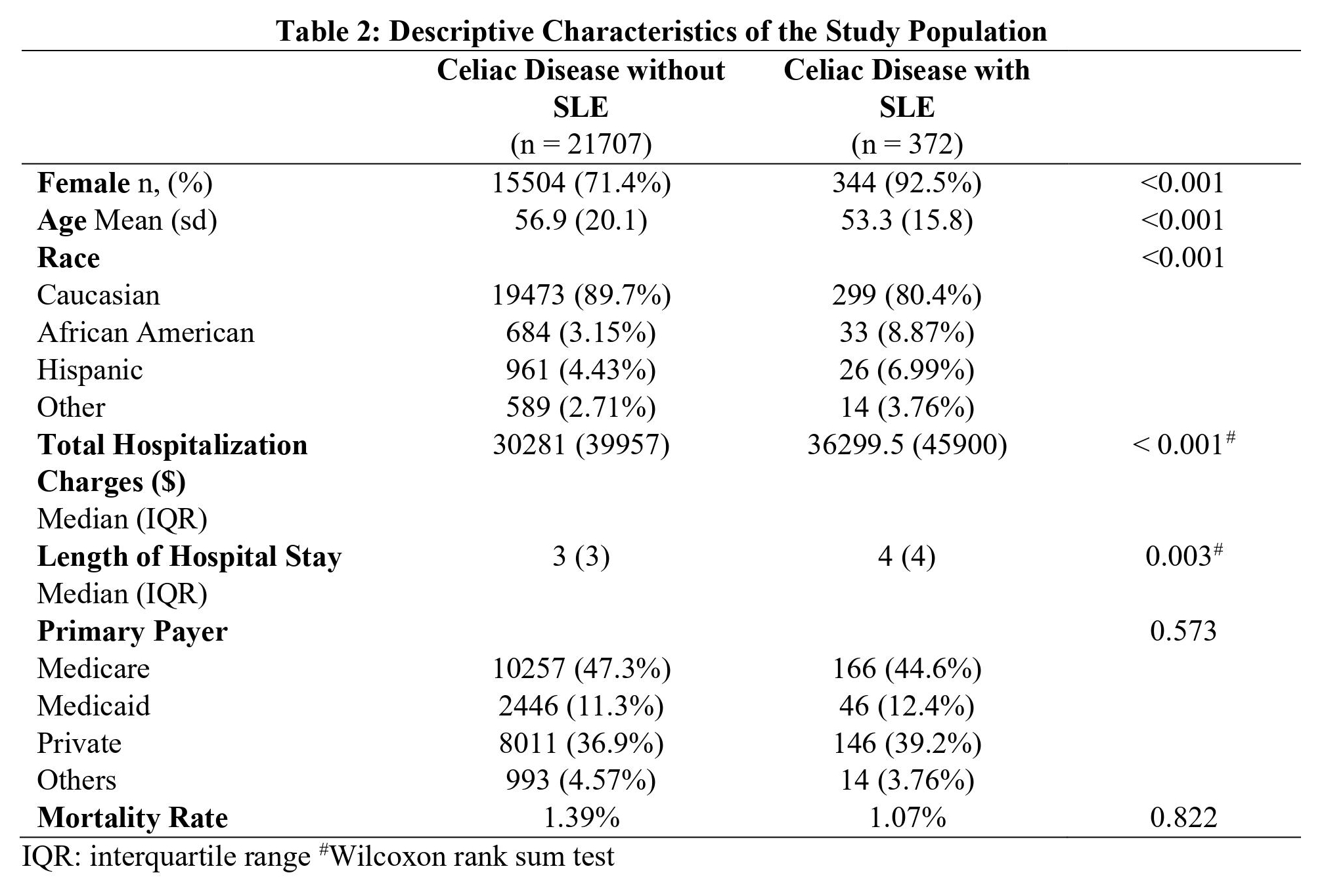
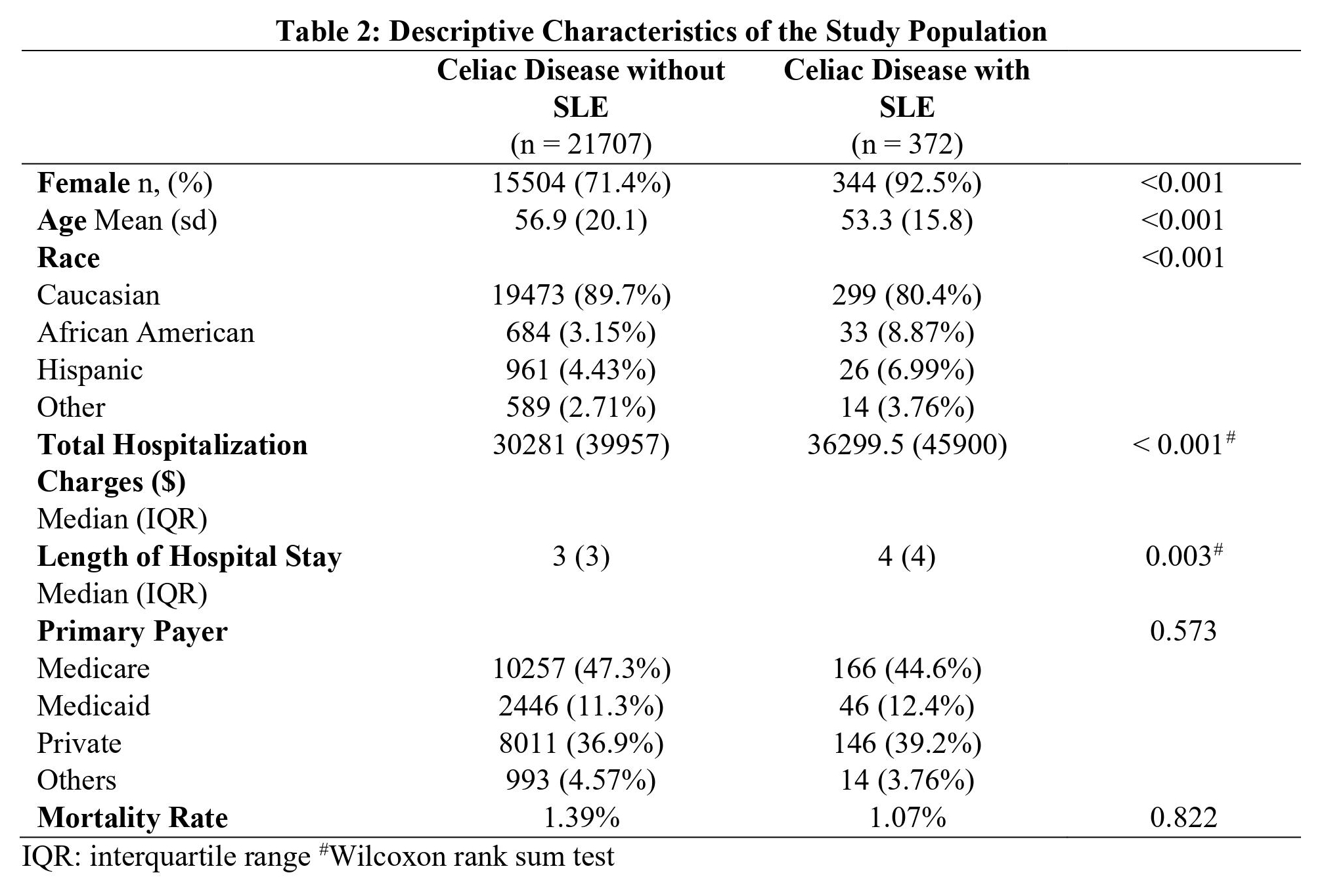
Methods: This is a cross-sectional study using Nationwide Inpatient Sample (NIS) from 2016 to 2018. We included hospitalizations of patients aged 18 or older, and with complete demographic information of gender, age, and race. Primary or secondary diagnoses of SLE and celiac disease were identified using International Classification of Diseases 10th edition (ICD-10). The prevalence odds ratio (OR) of celiac disease in SLE patients was assessed. Covariates for multivariate regression analysis were age, gender, race, calendar year, primary payer, household income, and comorbidities including diabetes mellitus, inflammatory bowel disease, chronic kidney disease, and metastatic malignancy. Utilization of healthcare resources including length of hospital stay and total hospitalization charges in patients with celiac disease were also examined. Categorical variables were analyzed using Chi-square test, and continuous variables using Student t-test or Wilcoxon rank-sum test. p < 0.05 was considered statistically significant. All the statistical analyses were performed using R (version 4.1.2).
Results: 372 records of patients with concurrent SLE and celiac disease were identified. The weight-adjusted inpatient prevalence of celiac disease in SLE was 0.36%, compared with 0.13% in patients without SLE. The adjusted OR of celiac disease in patients with SLE was 2.88 (95% CI: 2.60 – 3.31). The prevalence of celiac disease was higher in Caucasians, female patients, and those aged between 41 to 75. Among patients with celiac disease, patients with SLE were younger (53.3 vs 56.9%, p < 0.001), and more likely to be female (92.5% vs 71.4%, p < 0.001), and they were also associated with higher total hospitalization charges ($36299.5 vs $30281, p < 0.001) and slightly longer hospital stays (p = 0.003).
Conclusion: Patients with SLE had a higher prevalence of celiac disease than those without SLE. Among patients with celiac disease, those with SLE were associated with higher hospitalization charges and longer hospital stays.

Disclosures: J. Zheng, None; R. Ni, None; G. Zou, None; Y. Zeng, None; N. ijaz, None; Y. Zhang, None.
Background/Purpose: Celiac disease is an autoimmune disease characterized by the immunologic reaction to gluten by lymphocytes. Although recent studies suggest an association between celiac disease and other autoimmune diseases, its relationship with systemic lupus erythematosus (SLE) remains to be elucidated. In this study, we aimed to determine the prevalence of celiac disease in patients with SLE using a US-based national database.
Methods: This is a cross-sectional study using Nationwide Inpatient Sample (NIS) from 2016 to 2018. We included hospitalizations of patients aged 18 or older, and with complete demographic information of gender, age, and race. Primary or secondary diagnoses of SLE and celiac disease were identified using International Classification of Diseases 10th edition (ICD-10). The prevalence odds ratio (OR) of celiac disease in SLE patients was assessed. Covariates for multivariate regression analysis were age, gender, race, calendar year, primary payer, household income, and comorbidities including diabetes mellitus, inflammatory bowel disease, chronic kidney disease, and metastatic malignancy. Utilization of healthcare resources including length of hospital stay and total hospitalization charges in patients with celiac disease were also examined. Categorical variables were analyzed using Chi-square test, and continuous variables using Student t-test or Wilcoxon rank-sum test. p < 0.05 was considered statistically significant. All the statistical analyses were performed using R (version 4.1.2).
Results: 372 records of patients with concurrent SLE and celiac disease were identified. The weight-adjusted inpatient prevalence of celiac disease in SLE was 0.36%, compared with 0.13% in patients without SLE. The adjusted OR of celiac disease in patients with SLE was 2.88 (95% CI: 2.60 – 3.31). The prevalence of celiac disease was higher in Caucasians, female patients, and those aged between 41 to 75. Among patients with celiac disease, patients with SLE were younger (53.3 vs 56.9%, p < 0.001), and more likely to be female (92.5% vs 71.4%, p < 0.001), and they were also associated with higher total hospitalization charges ($36299.5 vs $30281, p < 0.001) and slightly longer hospital stays (p = 0.003).
Conclusion: Patients with SLE had a higher prevalence of celiac disease than those without SLE. Among patients with celiac disease, those with SLE were associated with higher hospitalization charges and longer hospital stays.

Disclosures: J. Zheng, None; R. Ni, None; G. Zou, None; Y. Zeng, None; N. ijaz, None; Y. Zhang, None.

