Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1202: Clinical Profile and Trend of Vasculitis in Patients with Acute Coronary Syndrome – Insight from National Database 2010 to 2019
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- PS
Palak Shah, MD
Metropolitan Hospital Center, New York Medical College
Jersey City, NJ, United States
Abstract Poster Presenter(s)
Palak Shah1, Ana Arevalo2, Rasha Alaameri3, Brinda Basida4, Urja Nagadia5, Sanket Basida5, shobhana Chaudhari6 and Monil Majmundar7, 1Metropolitan Hospital Center, New York Medical College, New York, NY, 2University of Chicago, Chicago, IL, 3New York Medical College/ Metropolitan Program, New York, NY, 4DMC/Sinai Grace Hospital, Detroit, MI, 5University of Missouri, Columbia, MO, 6NYC Health and Hospital/Metropolitan Hospital, New York, NY, 7University of Kansas Medical Center, Kansas City, KS
Background/Purpose: Vasculitides are characterized by inflammation of vessel walls with reactive damage to mural structures leading to compromise of the lumen. Vasculitides also accelerate atherosclerosis of coronary arteries leading to acute coronary syndrome. However, very little is known about the prevalence, trend, and clinical characteristics of vasculitis in patients hospitalized with the acute coronary syndrome (ACS).
Methods: We used a nationwide inpatient sample database from January 2010 to December 2019. Patients with ACS were identified using appropriate international classification of diseases (ICD) 9th and 10th edition of codes in primary discharge diagnosis. ACS included ST-elevation myocardial infarction and non-ST elevation myocardial infarction. We identified vasculitis patients using appropriate ICD codes in secondary diagnosis fields. Vasculitis included Takayasu's arteritis (TA), giant-cell arteritis (GCA), granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, vasculitis secondary to rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and Behcet's disease. We divided ACS into patients with and without vasculitis and compared their demographic and comorbidities burden. We assessed the trend of vasculitis, individual diseases, and inhospital mortality from 2010 to 2019. We also compared inhospital mortality between vasculitis and non-vasculitis groups. Demographic and comorbidities were compared using a chi-square test for categorical variables and a Wilcoxon-rank sum test for age. Non-parametric trend test was applied to assess the trend p-value. The trend p-value was adjusted for age and sex. Multivariable logistic regression was applied for inhospital mortality.
Results: We identified 7,076,477 ACS hospitalizations from 2010 to 2019. Out of which 146,062 (2.1%) hospitalization were of vasculitis. Among vasculitis, the prevalence of TA was 0.08/1000 ACS, GCA was 0.6/1000 ACS, ANCA was 0.3/1000 ACS, RA was 16.1/1000 ACS, SLE was 4.1/1000 ACS, and Behcet's disease was 0.03/1000 ACS. Patients with vasculitis were older, had more females, hypertension, stroke, atrial fibrillation, prior myocardial infarction, heart failure, chronic liver disease, chronic lung disease, and anemia (Table 1). The trend of vasculitis in ACS increased from 2010 to 2019 (p for trend < 0.001). The trend of RA (p for trend< 0.001) and SLE (p for trend< 0.001) was also increased. Trend of GCA (p for trend=0.256) and ANCA-vasculitis (p for trend=0.736) did not change. However, the trend of TA was decreased (p for trend< 0.001) (Figure 1). The trend of inhospital mortality decreased in both vasculitis and non-vasculitis groups (p< 0.001); however, decreased was more in the vasculitis group (p for interaction< 0.001). Vasculitis group was associated with 11% lower inhospital mortality compared with non-vasculitis group (odds ratio: 0.89, 95% CI: 0.84-0.94, p< 0.001) (Figure 2).
Conclusion: There is a high prevalence of vasculitis in patients hospitalized for ACS, and its trend increased from 2010 to 2019. Vasculitis was associated with a protective effect for mortality in ACS.
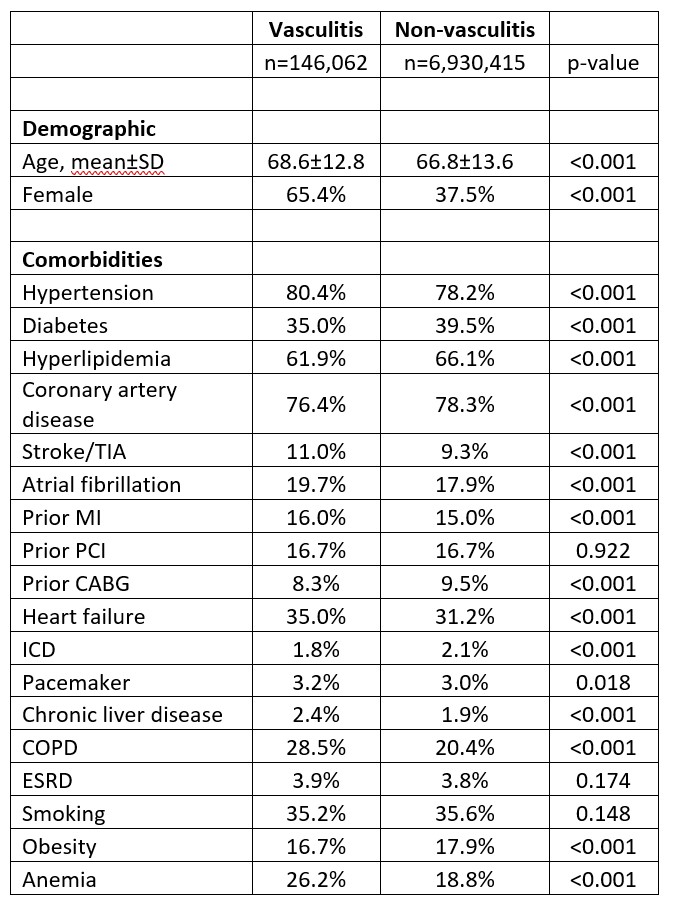 Table 1. Baseline characteristics of patients with acute coronary syndrome stratified based on vasculitis.
Table 1. Baseline characteristics of patients with acute coronary syndrome stratified based on vasculitis.
Abbreviations: CABG: coronary artery bypass graft, COPD: chronic lung disease, ESRD: end-stage renal disease, ICD: implantable cardioverter-defibrillator, MI: myocardial infarction, PCI: percutaneous coronary intervention, SD: standard deviation, TIA: transient ischemic attack,
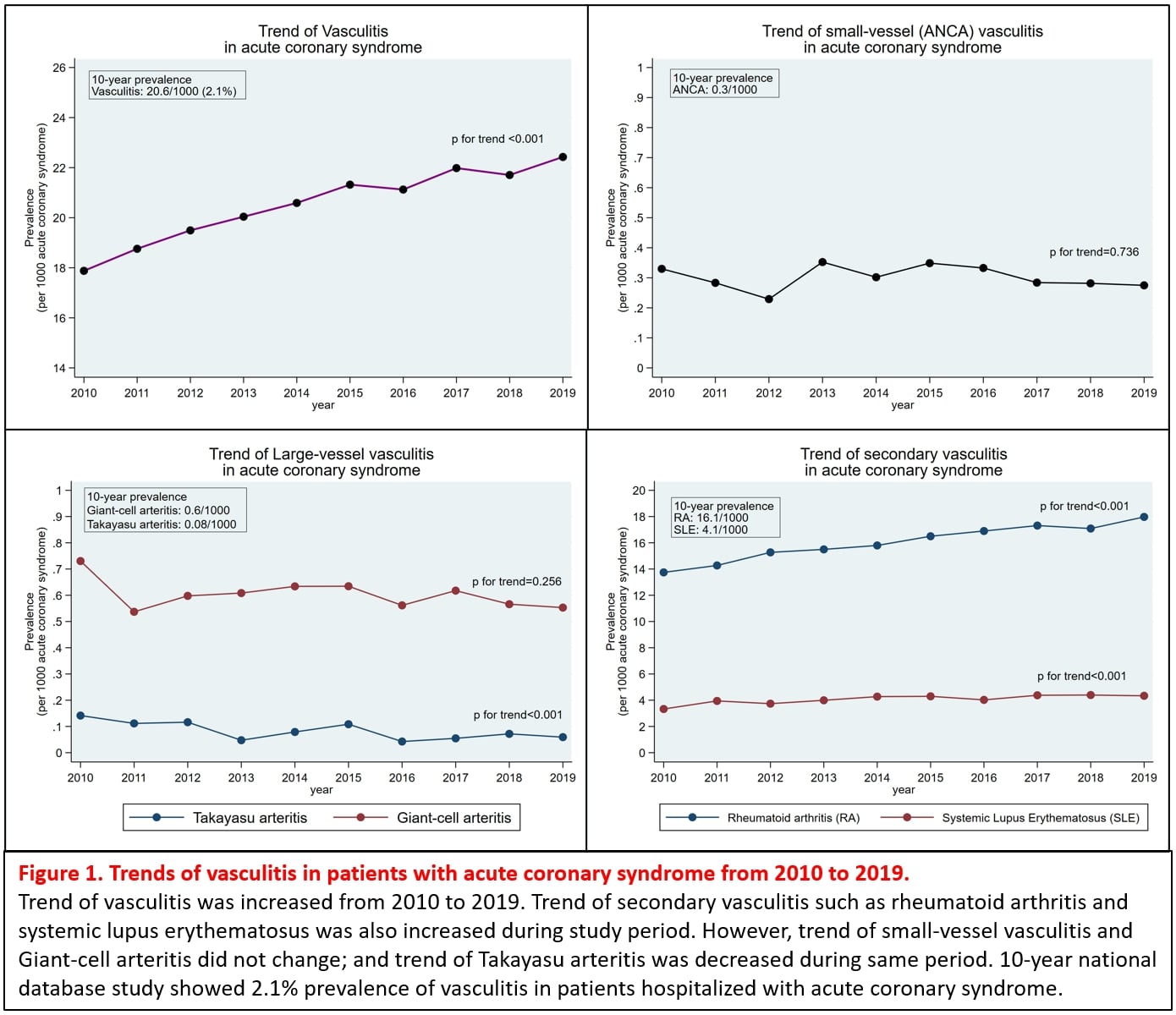 Figure 1. Trend of vasculitis in patients with acute coronary syndrome from 2010 to 2019.
Figure 1. Trend of vasculitis in patients with acute coronary syndrome from 2010 to 2019.
Trend of vasculitis increased from 2010 to 2019. Trend of secondary vasculitis such as rheumatoid arthritis and systemic lupus erythematosus was also increased during study period. However, trend of small-vessel vasculitis and Giant-cell arteritis did not change; and trend of Takayasu arteritis decreased during the same period. 10-year national database study showed 2.1% prevalence of vasculitis in patients hospitalized with acute coronary syndrome.
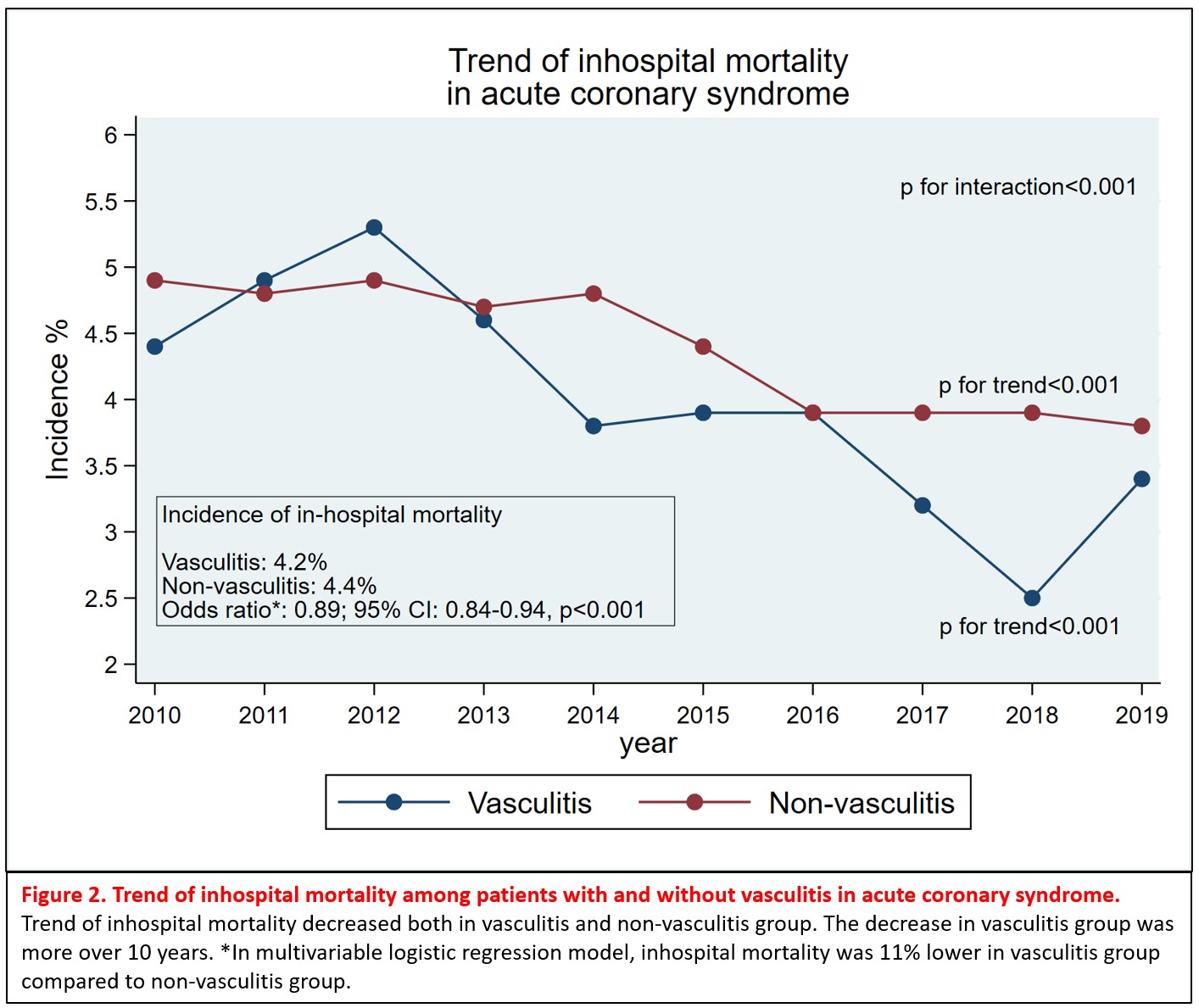 Figure 2. Trend of inhospital mortality among patients with and without vasculitis in acute coronary syndrome.
Figure 2. Trend of inhospital mortality among patients with and without vasculitis in acute coronary syndrome.
Trend of inhospital mortality decreased both in vasculitis and non-vasculitis groups. The decrease in vasculitis group was more over 10 years. *In multivariable logistic regression model, inhospital mortality was 11% lower in vasculitis group compared to non-vasculitis group.
Disclosures: P. Shah, None; A. Arevalo, None; R. Alaameri, None; B. Basida, None; U. Nagadia, None; S. Basida, None; s. Chaudhari, None; M. Majmundar, None.
Background/Purpose: Vasculitides are characterized by inflammation of vessel walls with reactive damage to mural structures leading to compromise of the lumen. Vasculitides also accelerate atherosclerosis of coronary arteries leading to acute coronary syndrome. However, very little is known about the prevalence, trend, and clinical characteristics of vasculitis in patients hospitalized with the acute coronary syndrome (ACS).
Methods: We used a nationwide inpatient sample database from January 2010 to December 2019. Patients with ACS were identified using appropriate international classification of diseases (ICD) 9th and 10th edition of codes in primary discharge diagnosis. ACS included ST-elevation myocardial infarction and non-ST elevation myocardial infarction. We identified vasculitis patients using appropriate ICD codes in secondary diagnosis fields. Vasculitis included Takayasu's arteritis (TA), giant-cell arteritis (GCA), granulomatosis with polyangiitis, eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, vasculitis secondary to rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and Behcet's disease. We divided ACS into patients with and without vasculitis and compared their demographic and comorbidities burden. We assessed the trend of vasculitis, individual diseases, and inhospital mortality from 2010 to 2019. We also compared inhospital mortality between vasculitis and non-vasculitis groups. Demographic and comorbidities were compared using a chi-square test for categorical variables and a Wilcoxon-rank sum test for age. Non-parametric trend test was applied to assess the trend p-value. The trend p-value was adjusted for age and sex. Multivariable logistic regression was applied for inhospital mortality.
Results: We identified 7,076,477 ACS hospitalizations from 2010 to 2019. Out of which 146,062 (2.1%) hospitalization were of vasculitis. Among vasculitis, the prevalence of TA was 0.08/1000 ACS, GCA was 0.6/1000 ACS, ANCA was 0.3/1000 ACS, RA was 16.1/1000 ACS, SLE was 4.1/1000 ACS, and Behcet's disease was 0.03/1000 ACS. Patients with vasculitis were older, had more females, hypertension, stroke, atrial fibrillation, prior myocardial infarction, heart failure, chronic liver disease, chronic lung disease, and anemia (Table 1). The trend of vasculitis in ACS increased from 2010 to 2019 (p for trend < 0.001). The trend of RA (p for trend< 0.001) and SLE (p for trend< 0.001) was also increased. Trend of GCA (p for trend=0.256) and ANCA-vasculitis (p for trend=0.736) did not change. However, the trend of TA was decreased (p for trend< 0.001) (Figure 1). The trend of inhospital mortality decreased in both vasculitis and non-vasculitis groups (p< 0.001); however, decreased was more in the vasculitis group (p for interaction< 0.001). Vasculitis group was associated with 11% lower inhospital mortality compared with non-vasculitis group (odds ratio: 0.89, 95% CI: 0.84-0.94, p< 0.001) (Figure 2).
Conclusion: There is a high prevalence of vasculitis in patients hospitalized for ACS, and its trend increased from 2010 to 2019. Vasculitis was associated with a protective effect for mortality in ACS.
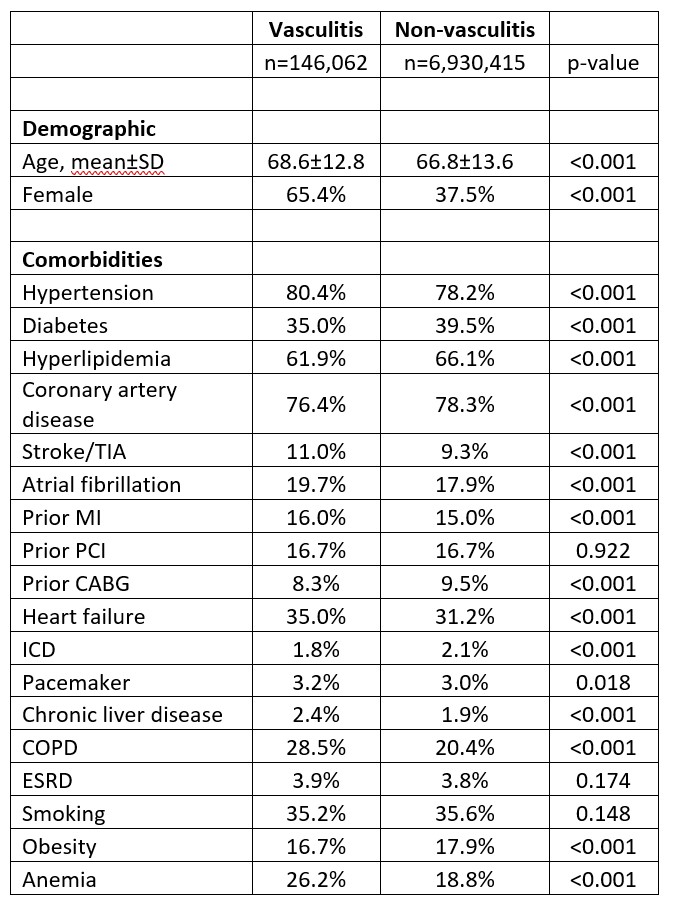 Table 1. Baseline characteristics of patients with acute coronary syndrome stratified based on vasculitis.
Table 1. Baseline characteristics of patients with acute coronary syndrome stratified based on vasculitis.Abbreviations: CABG: coronary artery bypass graft, COPD: chronic lung disease, ESRD: end-stage renal disease, ICD: implantable cardioverter-defibrillator, MI: myocardial infarction, PCI: percutaneous coronary intervention, SD: standard deviation, TIA: transient ischemic attack,
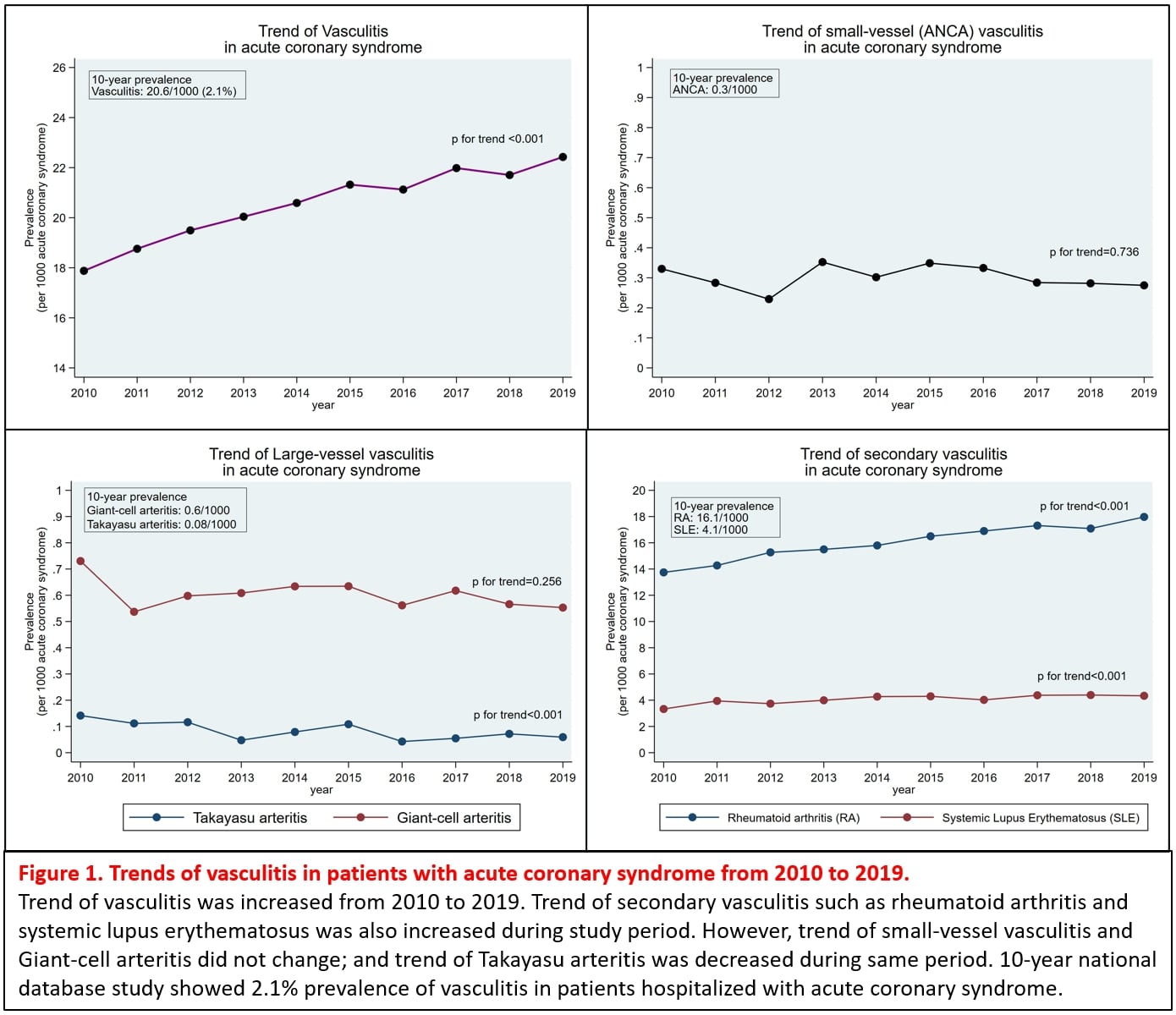 Figure 1. Trend of vasculitis in patients with acute coronary syndrome from 2010 to 2019.
Figure 1. Trend of vasculitis in patients with acute coronary syndrome from 2010 to 2019.Trend of vasculitis increased from 2010 to 2019. Trend of secondary vasculitis such as rheumatoid arthritis and systemic lupus erythematosus was also increased during study period. However, trend of small-vessel vasculitis and Giant-cell arteritis did not change; and trend of Takayasu arteritis decreased during the same period. 10-year national database study showed 2.1% prevalence of vasculitis in patients hospitalized with acute coronary syndrome.
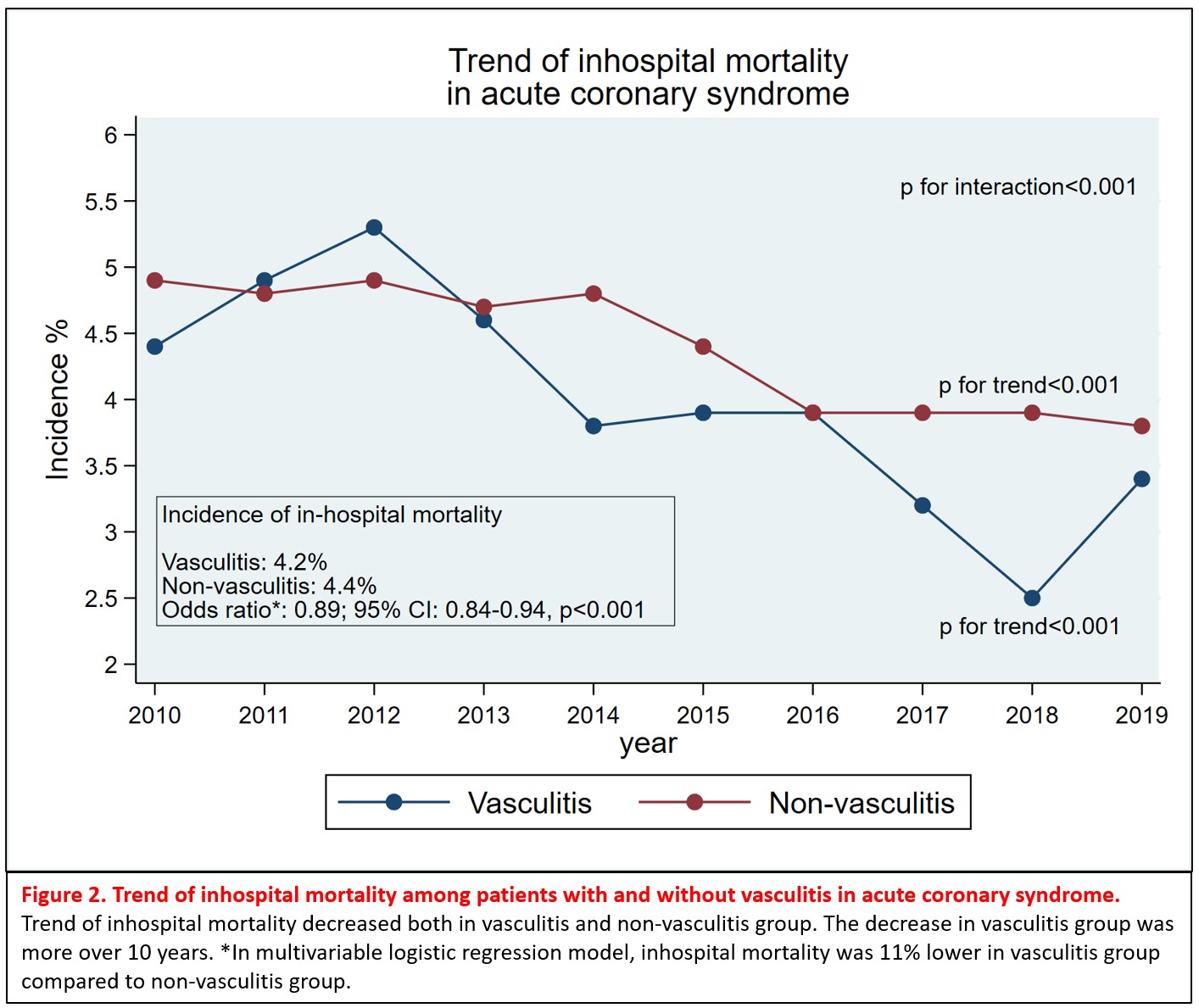 Figure 2. Trend of inhospital mortality among patients with and without vasculitis in acute coronary syndrome.
Figure 2. Trend of inhospital mortality among patients with and without vasculitis in acute coronary syndrome.Trend of inhospital mortality decreased both in vasculitis and non-vasculitis groups. The decrease in vasculitis group was more over 10 years. *In multivariable logistic regression model, inhospital mortality was 11% lower in vasculitis group compared to non-vasculitis group.
Disclosures: P. Shah, None; A. Arevalo, None; R. Alaameri, None; B. Basida, None; U. Nagadia, None; S. Basida, None; s. Chaudhari, None; M. Majmundar, None.

