Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1465: Clinical Profiling and Antiphospholipid Antibody (aPL) Associations in Indian Systemic Lupus Erythematosus (SLE) Cohort
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- VS
Vineeta Shobha, MD, DM
St. John's National Academy of Health Science
Bangalore, Karnataka, India
Abstract Poster Presenter(s)
Vineeta Shobha1, Liza Rajasekhar2, Sandra Manuel1, Chengappa Kavadichanda3, Ashish J Mathew4, Ranjan Gupta5, Manish Rathi6, Parasar Ghosh7, Saumya Ranjan Tripathy8, Avinash Jain9 and Amita Aggarwal10, 1St. John’s Medical College Hospital, Bangalore, India, 2Nizam's Institute of Medical Sciences, Madhapur, India, 3JIPMER, Pondicherry, Puducherry, India, 4Rigshospitalet, Copenhagen, Denmark, 5All India Institute of Medical Sciences, New Delhi, India, 6PGIMER Chandigarh, Chandigarh, India, 7Govt of West Bengal, Kolkata, India, Kolkata, West Bengal, India, 8SCB medical college, Cuttack, India, 9SMS Medical College, Lucknow, India, 10Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
Background/Purpose: Antiphospholipid Antibody (aPL) are described in 11-40% of patients with SLE. Whether the presence of any of the aPLs or combinations thereof, can accurately predict the risk of thrombosis, non-thrombotic events and obstetric outcome in SLE has been debatable. We report the prevalence, associations and outcomes in SLE patients with aPL.
Methods: From the ongoing prospective INdian SLE inception cohort (INSPIRE) data was extracted for SLE patients for whom complete data was available for all the five routinely performed aPL- lupus anticoagulant (LAC), IgG and IgM isotypes for anticardiolipin antibody(aCL) and anti-β2-glycoprotein-I (β2GPI) at enrolment. Patients were categorised into no aPL, triple positive [positive for all 3; LAC, aCL (IgG and or IgM), anti-β2-GPI (IgG and or IgM)], dual positive (any 2 of 3; LAC / aCL / β2-GPI) and isolated aPL positive. The aPL antibodies methodology and cut offs were as per recommendations (1,2). Patients with thrombotic, non-criteria/ non-thrombotic events (NTE) and obstetric outcomes were analysed for associations and compared against those who were negative for all aPL. Odds ratio (OR) adjusted for age, gender and SLEDAI was calculated for all variables except obstetric manifestations, where OR was adjusted for age and SLEDAI.
1.Update of the guidelines for lupus anticoagulant detection 7(10),1737–1740
2.International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome J.Thromb. Haemost. 2006,4,295–306
Results: We analysed 1023 patients (92.6% women), mean age 28.7 ± 10.1 years including 105(10.3%) children. 36 (3.5%) were identified as triple positive and at least one aPL antibody was detected in 358(35%). Overall, the aPL positive group had significant association with gangrene, myocardial infarction, stroke, 2nd trimester miscarriage, thrombocytopenia and autoimmune hemolytic anaemia (p< 0.05). Fig1
There were 82 thrombotic events in 66 patients (6.5%) in our cohort and thrombotic events were associated with presence of LAC [aOR 1.78(1.0,3.17)] and β2-GPI [aOR 2.23(1.04,4.78)]. Tab 1
There were 984 conceptions in 456 women, averaging 2.1 conceptions per woman. There were 194 obstetric events of interest and were significantly associated with at least one aPL positivity [aOR 1.473(0.98,2.19)]. Low birth weight had high odds with triple positivity [aOR 2.708(1.01,7.39)] and 2nd trimester miscarriages with presence of LAC [aOR 3.213(1.19,8.62)]. Tab 2
Amongst the non-criteria events, AIHA had higher odds of occurrence with LAC [aOR 1.80(1.09,2.97)], dual positivity [aOR 2.18(1.51,3.16)], thrombocytopenia with dual positivity [aOR 2.98(1.85,4.8)] and any NTE with LAC [aOR 1.63(1.01,2.65)]. Tab1
There were 44/1023(4.3%) deaths in this cohort, 22/358(6.1%) in the aPL group and 22/ 665(3.3%) in the non-APS group, hazard ratio being [1.91(1.04,3.51)] in those with at least one aPL positivity and [3.18(1.46,6.87)] in dual positives after adjusting for age, gender and SLEDAI.
Conclusion: Antiphospholipid antibodies are present in nearly one-third of patients in INSPIRE cohort and their presence increases the risk of thrombotic events, adverse foetal outcomes, non- thrombotic events and mortality.
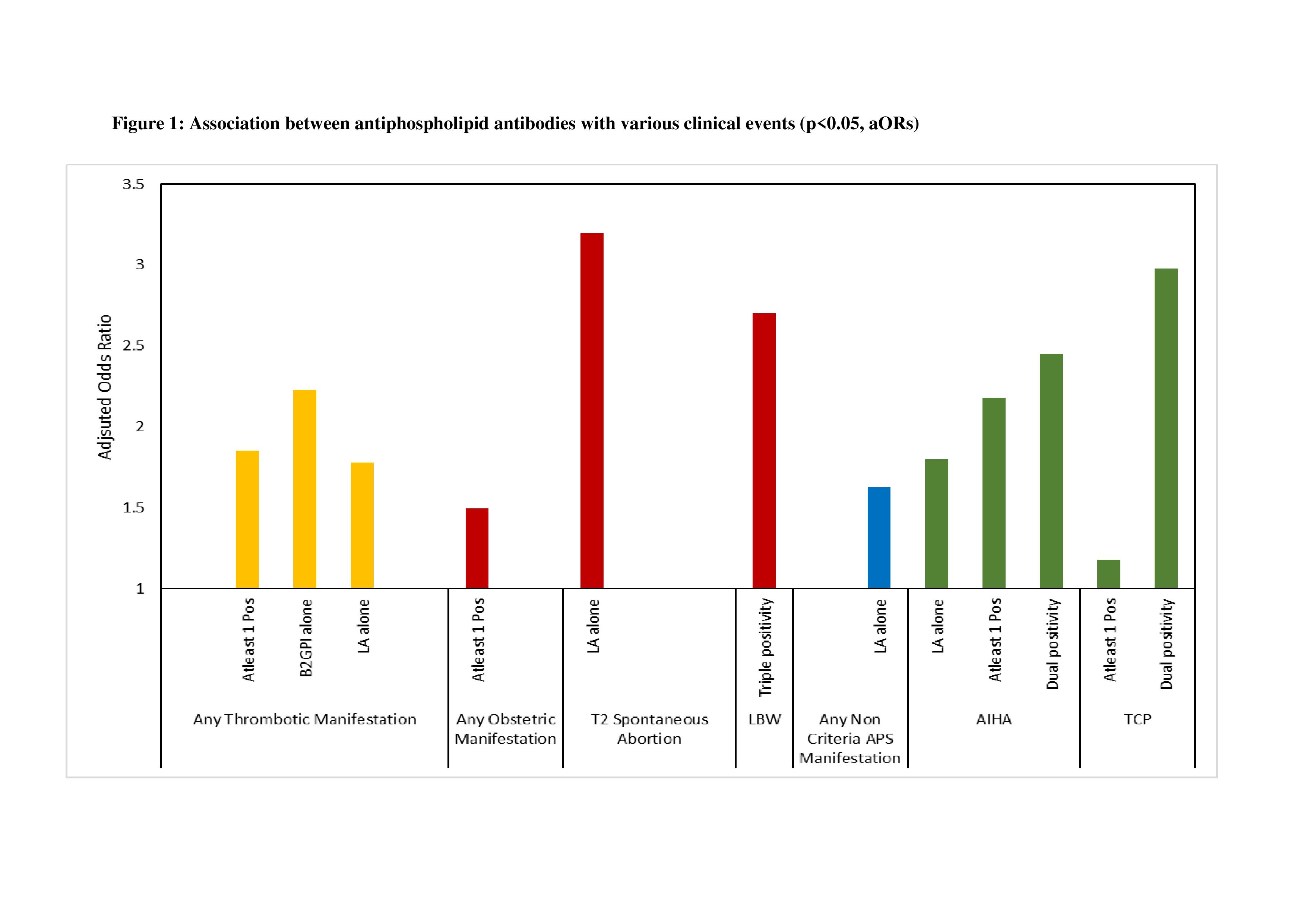 Figure 1: Association between Antiphospholipid Antibodies with various clinical events (p < 0.05, aORs).
Figure 1: Association between Antiphospholipid Antibodies with various clinical events (p < 0.05, aORs).
Abbreviation: LA - Lupus Anticoagulant, Pos – Positive, T2 Spontaneous Abortion - Spontaneous Abortion in 2nd Trimester, LBW- Low Birth Weight, APS- Antiphospholipid Syndrome, AIHA- Autoimmune Hemolytic Anemia, TCP- Thrombocytopenia.
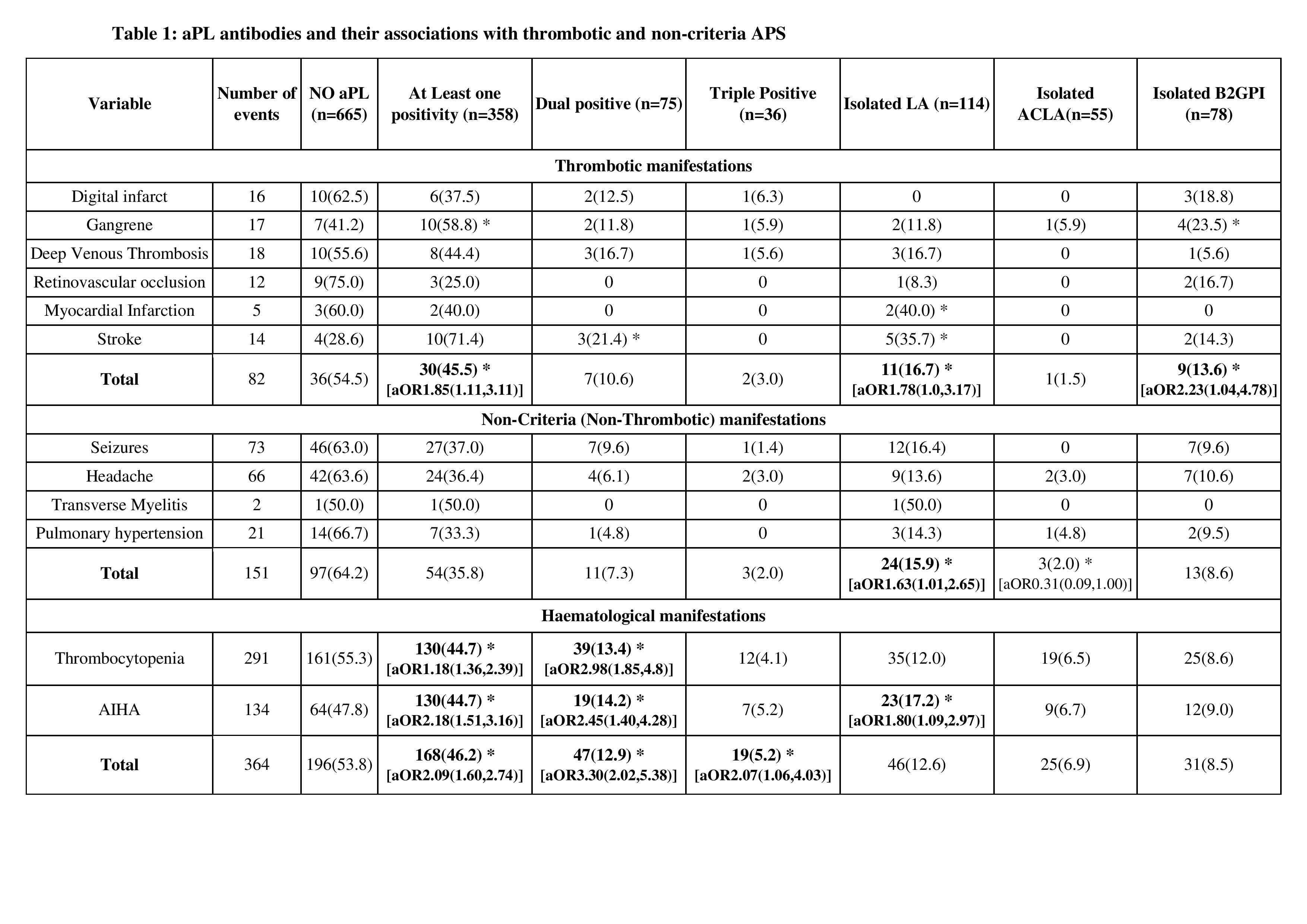 Table 1: aPL Antibodies and their associations with thrombotic and non-criteria APS manifestations .
Table 1: aPL Antibodies and their associations with thrombotic and non-criteria APS manifestations .
Only significant values are reported, * denotes p < 0.05, Adjusted Odds Ratio with confidence Interval denoted as [aOR(C.I)]; adjusted for age and gender and SLEDAI. Abbreviation: AIHA - Autoimmune Hemolytic anaemia, APS - antiphospholipid syndrome.
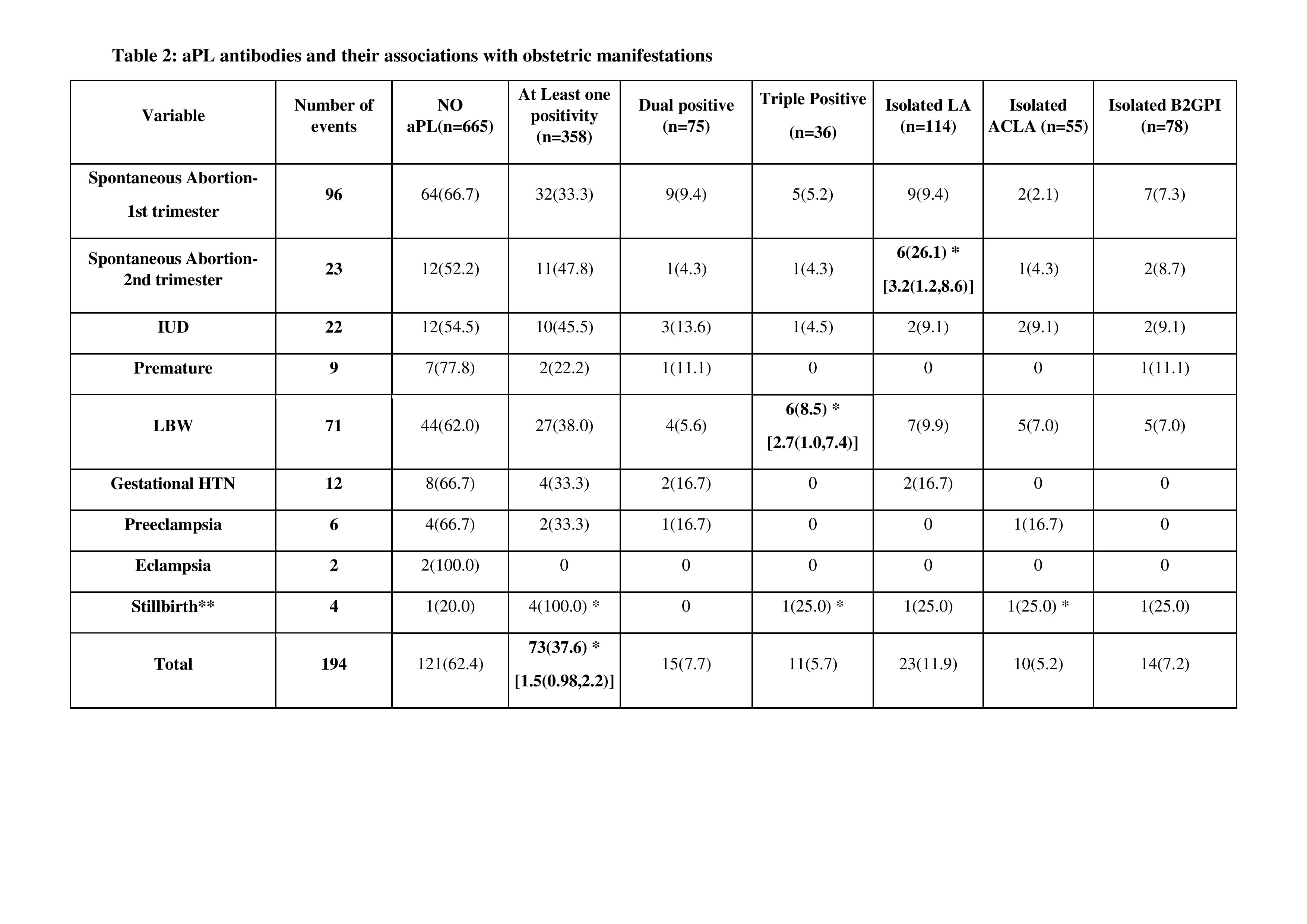 Table 2: aPL Antibodies and their associations with obstetric manifestations.
Table 2: aPL Antibodies and their associations with obstetric manifestations.
Only significant values are reported, * denotes p < 0.05, Adjusted Odds Ratio with confidence Interval denoted as [aOR (C.I)]; adjusted for age and SLEDAI.
**For Stillbirth, aOR is not calculated due to small sample size.
Abbreviation: IUD - Intrauterine death, LBW - Low birth weight, Gestational HTN - Gestational hypertension.
Disclosures: V. Shobha, None; L. Rajasekhar, None; S. Manuel, None; C. Kavadichanda, None; A. Mathew, None; R. Gupta, None; M. Rathi, None; P. Ghosh, None; S. Tripathy, None; A. Jain, None; A. Aggarwal, None.
Background/Purpose: Antiphospholipid Antibody (aPL) are described in 11-40% of patients with SLE. Whether the presence of any of the aPLs or combinations thereof, can accurately predict the risk of thrombosis, non-thrombotic events and obstetric outcome in SLE has been debatable. We report the prevalence, associations and outcomes in SLE patients with aPL.
Methods: From the ongoing prospective INdian SLE inception cohort (INSPIRE) data was extracted for SLE patients for whom complete data was available for all the five routinely performed aPL- lupus anticoagulant (LAC), IgG and IgM isotypes for anticardiolipin antibody(aCL) and anti-β2-glycoprotein-I (β2GPI) at enrolment. Patients were categorised into no aPL, triple positive [positive for all 3; LAC, aCL (IgG and or IgM), anti-β2-GPI (IgG and or IgM)], dual positive (any 2 of 3; LAC / aCL / β2-GPI) and isolated aPL positive. The aPL antibodies methodology and cut offs were as per recommendations (1,2). Patients with thrombotic, non-criteria/ non-thrombotic events (NTE) and obstetric outcomes were analysed for associations and compared against those who were negative for all aPL. Odds ratio (OR) adjusted for age, gender and SLEDAI was calculated for all variables except obstetric manifestations, where OR was adjusted for age and SLEDAI.
1.Update of the guidelines for lupus anticoagulant detection 7(10),1737–1740
2.International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome J.Thromb. Haemost. 2006,4,295–306
Results: We analysed 1023 patients (92.6% women), mean age 28.7 ± 10.1 years including 105(10.3%) children. 36 (3.5%) were identified as triple positive and at least one aPL antibody was detected in 358(35%). Overall, the aPL positive group had significant association with gangrene, myocardial infarction, stroke, 2nd trimester miscarriage, thrombocytopenia and autoimmune hemolytic anaemia (p< 0.05). Fig1
There were 82 thrombotic events in 66 patients (6.5%) in our cohort and thrombotic events were associated with presence of LAC [aOR 1.78(1.0,3.17)] and β2-GPI [aOR 2.23(1.04,4.78)]. Tab 1
There were 984 conceptions in 456 women, averaging 2.1 conceptions per woman. There were 194 obstetric events of interest and were significantly associated with at least one aPL positivity [aOR 1.473(0.98,2.19)]. Low birth weight had high odds with triple positivity [aOR 2.708(1.01,7.39)] and 2nd trimester miscarriages with presence of LAC [aOR 3.213(1.19,8.62)]. Tab 2
Amongst the non-criteria events, AIHA had higher odds of occurrence with LAC [aOR 1.80(1.09,2.97)], dual positivity [aOR 2.18(1.51,3.16)], thrombocytopenia with dual positivity [aOR 2.98(1.85,4.8)] and any NTE with LAC [aOR 1.63(1.01,2.65)]. Tab1
There were 44/1023(4.3%) deaths in this cohort, 22/358(6.1%) in the aPL group and 22/ 665(3.3%) in the non-APS group, hazard ratio being [1.91(1.04,3.51)] in those with at least one aPL positivity and [3.18(1.46,6.87)] in dual positives after adjusting for age, gender and SLEDAI.
Conclusion: Antiphospholipid antibodies are present in nearly one-third of patients in INSPIRE cohort and their presence increases the risk of thrombotic events, adverse foetal outcomes, non- thrombotic events and mortality.
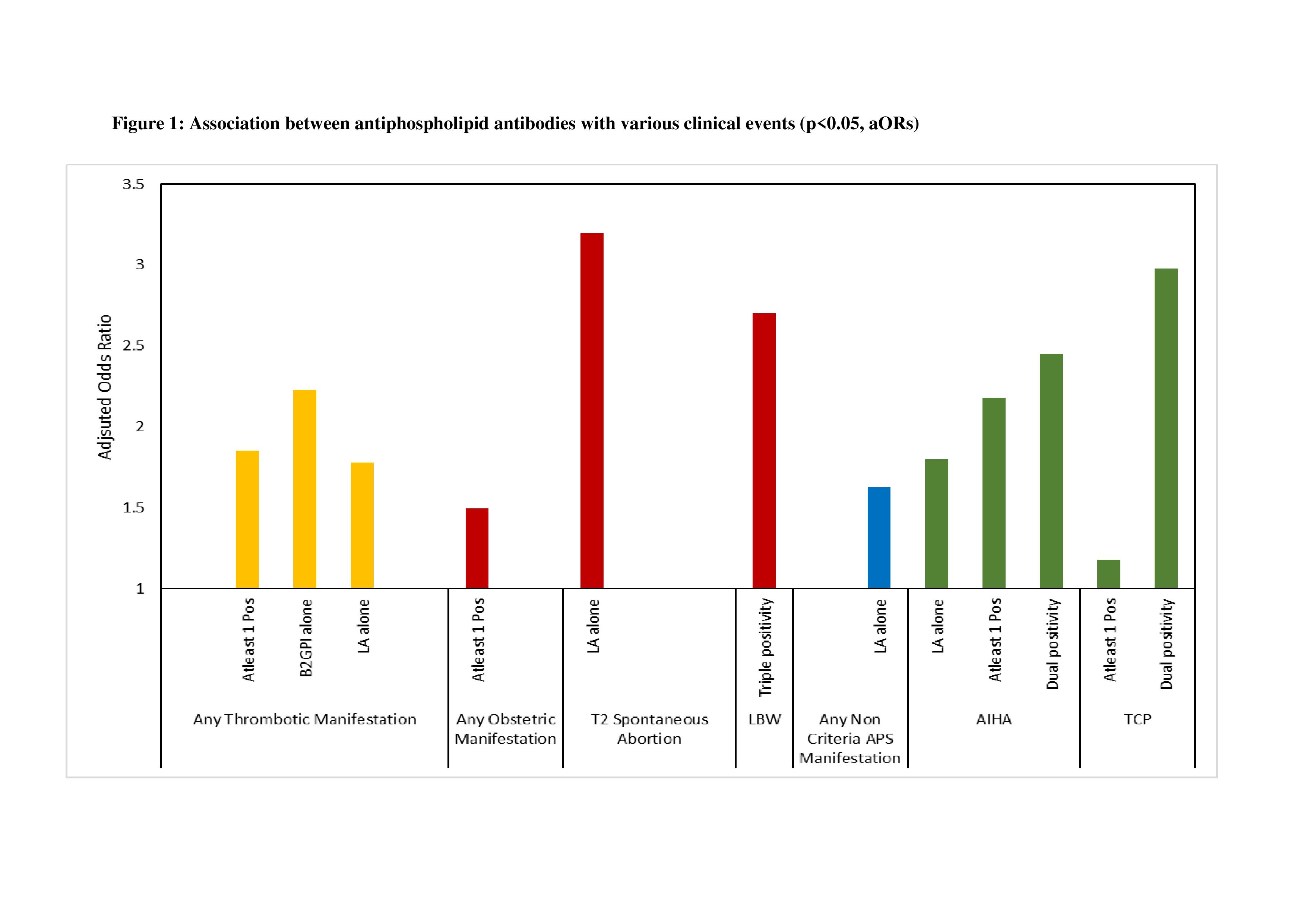 Figure 1: Association between Antiphospholipid Antibodies with various clinical events (p < 0.05, aORs).
Figure 1: Association between Antiphospholipid Antibodies with various clinical events (p < 0.05, aORs).Abbreviation: LA - Lupus Anticoagulant, Pos – Positive, T2 Spontaneous Abortion - Spontaneous Abortion in 2nd Trimester, LBW- Low Birth Weight, APS- Antiphospholipid Syndrome, AIHA- Autoimmune Hemolytic Anemia, TCP- Thrombocytopenia.
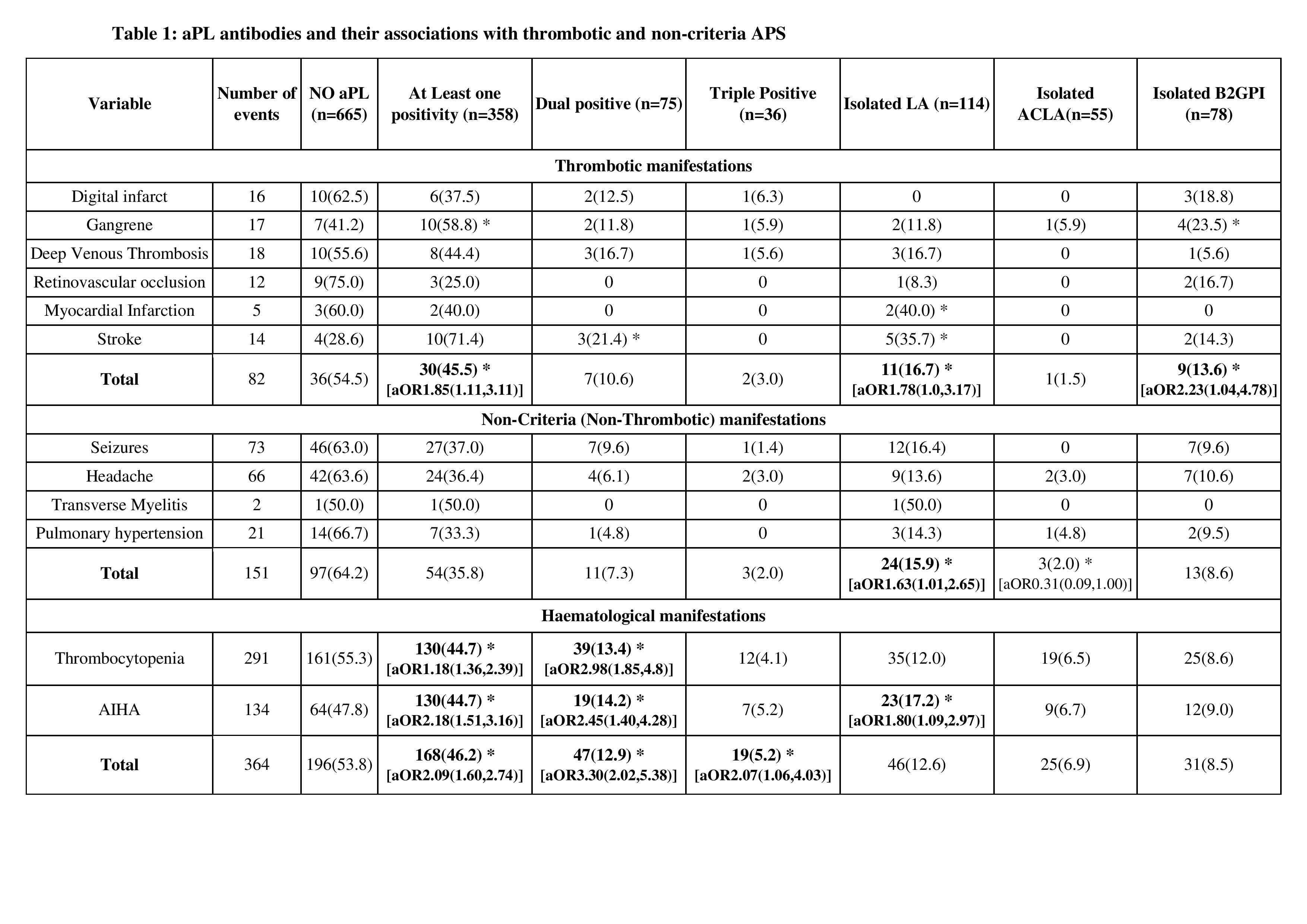 Table 1: aPL Antibodies and their associations with thrombotic and non-criteria APS manifestations .
Table 1: aPL Antibodies and their associations with thrombotic and non-criteria APS manifestations .Only significant values are reported, * denotes p < 0.05, Adjusted Odds Ratio with confidence Interval denoted as [aOR(C.I)]; adjusted for age and gender and SLEDAI. Abbreviation: AIHA - Autoimmune Hemolytic anaemia, APS - antiphospholipid syndrome.
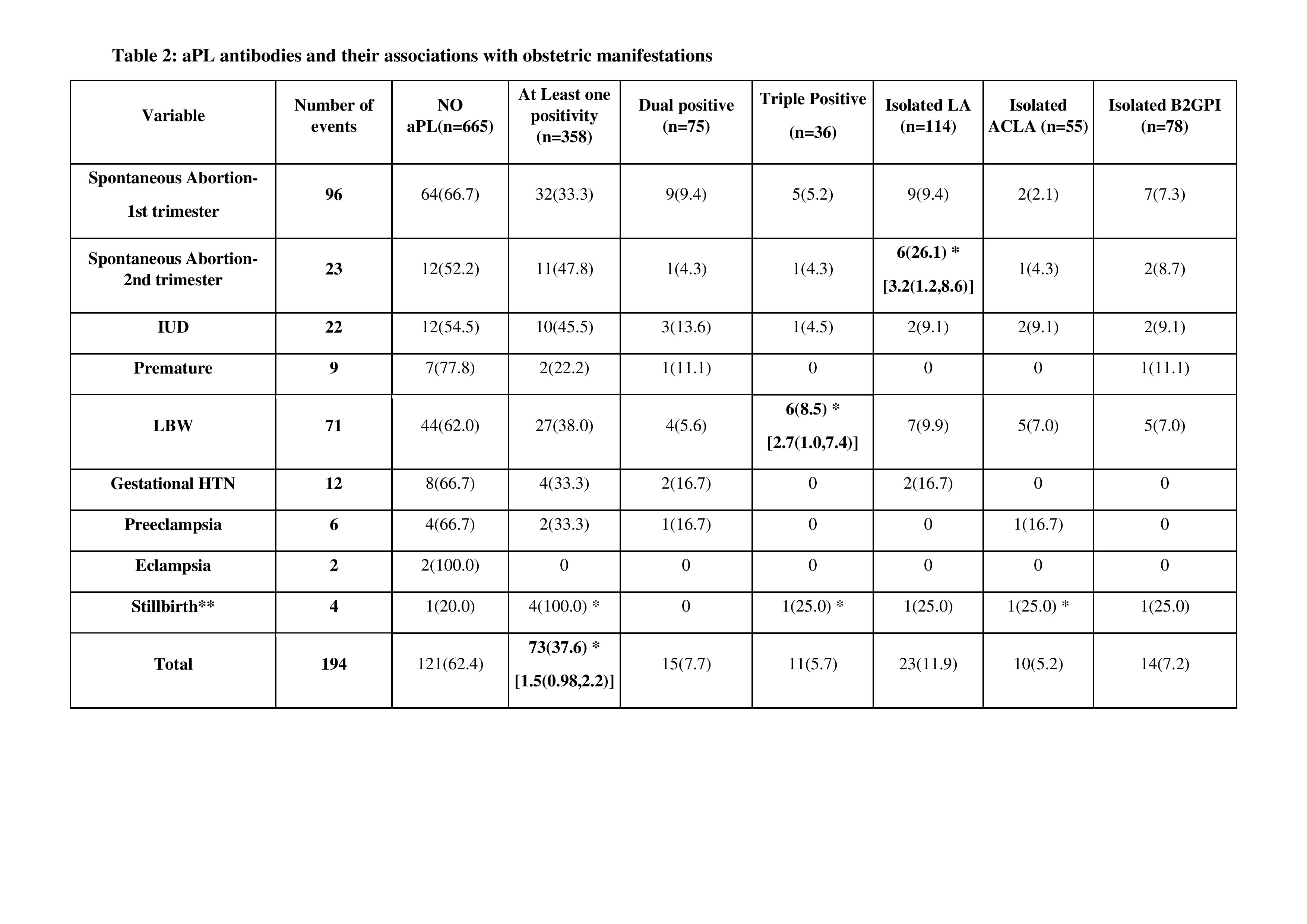 Table 2: aPL Antibodies and their associations with obstetric manifestations.
Table 2: aPL Antibodies and their associations with obstetric manifestations.Only significant values are reported, * denotes p < 0.05, Adjusted Odds Ratio with confidence Interval denoted as [aOR (C.I)]; adjusted for age and SLEDAI.
**For Stillbirth, aOR is not calculated due to small sample size.
Abbreviation: IUD - Intrauterine death, LBW - Low birth weight, Gestational HTN - Gestational hypertension.
Disclosures: V. Shobha, None; L. Rajasekhar, None; S. Manuel, None; C. Kavadichanda, None; A. Mathew, None; R. Gupta, None; M. Rathi, None; P. Ghosh, None; S. Tripathy, None; A. Jain, None; A. Aggarwal, None.

