Back
Poster Session C
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1166–1185) Systemic Sclerosis and Related Disorders – Basic Science Poster
1180: Deficiency and Altered Phenotype of Mucosal-associated Invariant T Cells in Systemic Sclerosis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ML
Manon LESTURGIE-TALAREK, MD
Paris University
Paris, France
Abstract Poster Presenter(s)
Manon Lesturgie-Talarek1, Virginie Gonzalez1, Camelia Frantz2, Noémie Sénot1, Zouriatou Gouda1, Camille Rousseau1, Lucie Beaudoin1, Agnès Lehuen1, Jérôme Avouac3 and Yannick Allanore4, 1INSERM U1016, Institut Cochin, Paris, France, 2Hôpital Cochin, AP-HP Centre - Université Paris Cité, Paris, France, 3University of Paris, Paris, France, 4Department of Rheumatology A, Descartes University, APHP, Cochin Hospital, Paris, France, Paris, France
Background/Purpose: Systemic sclerosis (SSc) is an autoimmune disease characterized by fibrosis of the skin and internal organs such as the lung. Mucosal-associated invariant T (MAIT) cells are innate-like T lymphocytes able to produce various cytokines and cytotoxic mediators such as granzyme B. Decreased level and altered phenotype of MAIT cell have been shown in various autoimmune disease. Moreover, some data support a potential role in fibrotic disorders as highlighted in liver fibrosis. Therefore, we herein addressed the question as whether MAIT cells may have an altered profile in systemic sclerosis.
Our objective was to determine the implication of MAIT cells in SSc.
Methods: MAIT cell frequency was analyzed by flow cytometry, using fresh peripheral blood from 74 consecutive SSc patients compared to 44 healthy donors. In addition, in depth MAIT cell phenotype and function were analyzed using fresh peripheral blood from 29 women with SSc compared to 23 healthy women donors.
Results: Most of the healthy donors were female (95%) and the mean age was 45.6 years. Among the 74 SSc patients (89% were female, mean age: 57 years), the mean disease duration was 9 years, 42% had diffuse cutaneous SSc and 48% had an interstitial lung disease (ILD). Proportion of circulating MAIT cell frequency was significantly reduced by 55% in SSc compared to healthy donors (1.4 % vs. 3.1%, p< 0.0001) (Figure 1A). We next investigated whether MAIT cell frequency was associated with clinical variables in SSc patients. MAIT cell frequency was significantly reduced in patients with interstitial lung disease (SSc-ILD) (0.49% vs. 0.91% in patients without ILD, p=0.027) (Figure 1B) even lower in the patients with severe ILD and reduced forced vital capacity (FVC) (0.25% in patients with FVC < 75% vs. 0.94% in patients with FVC >75%). Deficiency of MAIT cells did not correlate with disease activity score, type of SSc (diffuse or limited), systemic inflammation, and current immunosuppressive therapy.
In SSc patients, MAIT cells displayed a strongly activated phenotype indicated by markedly increased CD69+ MAIT cell frequency compared to healthy donors (p=0.0015, Figure 2A). Decreased proportion of MAIT expressing the anti-apoptotic marker Bcl2 was also observed. Regarding the cytokine profile analysis, no difference was observed compared to healthy controls (Figure 2A). Interestingly, MAIT cells from SSc-ILD patients had a more pronounced altered phenotype compared to SSc without ILD, with a correlation between MAIT expressing CCR6+ and MAIT frequency and a decreased production of IFN-γ (Figure 2B).
Conclusion: Circulating MAIT cells were reduced and exhibited an activated and pro-apoptotic phenotype in SSc patients compared to healthy controls. This peripheral MAIT cell deficiency may be related to enhanced apoptosis and/or homing in inflamed tissue, in particular the lung in SSc-ILD patients. Indeed, peripheral MAIT decrease was even more pronounced in SSc-ILD patients, and correlated with the expression of the tissue-recruitment chemokine CCR6. MAIT cells study in lung tissue as well as functional studies are necessary to better understand the implication of MAIT cells in systemic sclerosis.
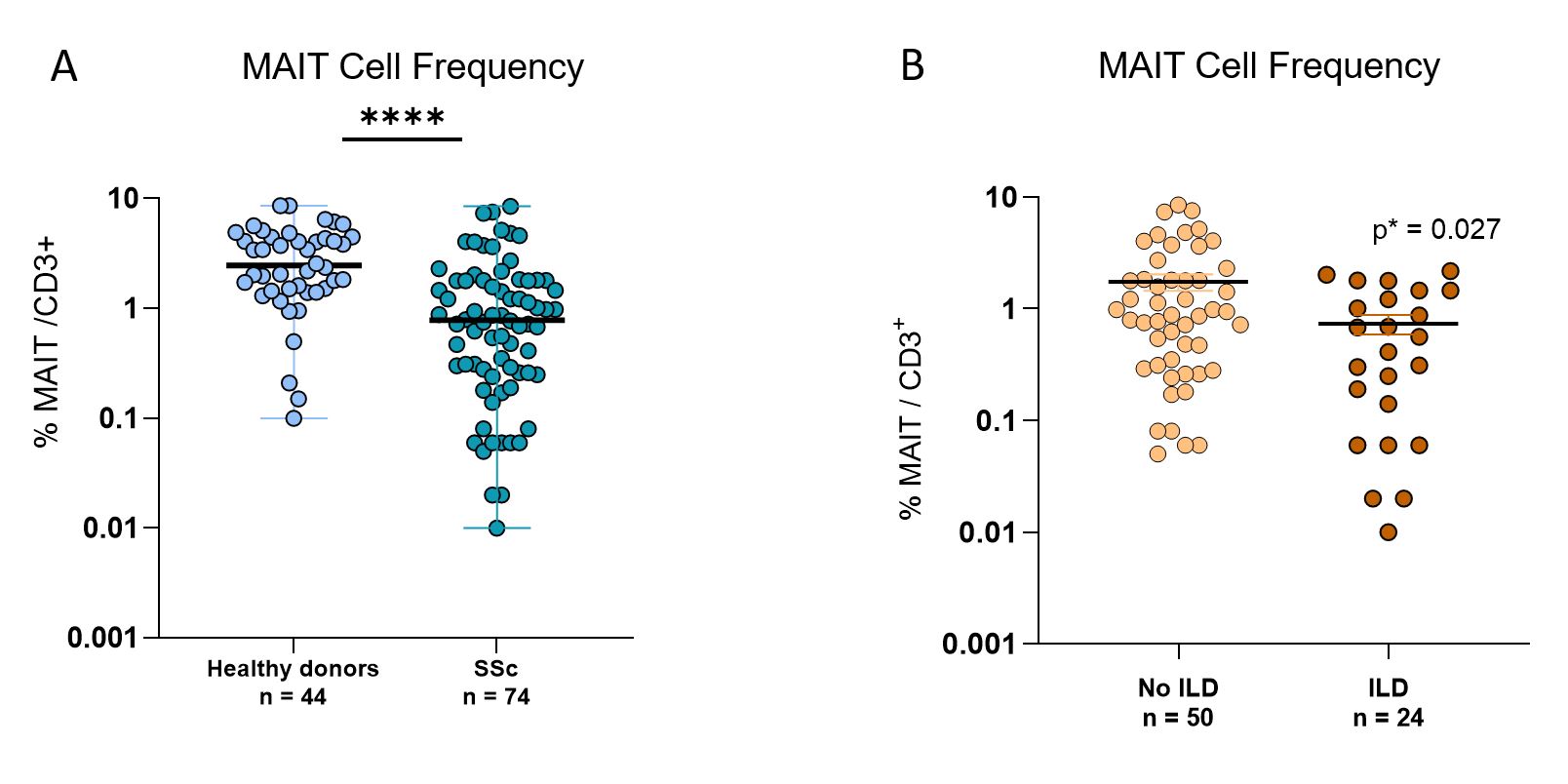 MAIT cell frequency. (A) MAIT cell frequency in SSc (n=74) compared to healthy donors (n=44). (B) MAIT cell frequency in SSc with ILD (n=24) compared to SSc without ILD (n=50). ILD: interstitial lung disease. SSc: systemic sclerosis. Test: Mann-Whitney. **** p < 0.0001.
MAIT cell frequency. (A) MAIT cell frequency in SSc (n=74) compared to healthy donors (n=44). (B) MAIT cell frequency in SSc with ILD (n=24) compared to SSc without ILD (n=50). ILD: interstitial lung disease. SSc: systemic sclerosis. Test: Mann-Whitney. **** p < 0.0001.
.jpg) Phenotype and function analysis of MAIT cells. The phenotype analysis included the study of activation (CD69, CD25, CD27), exhaustion (PD1, Tim3), recruitment (CD56, CCR6), survival (Bcl2, CD127) and proliferation (Ki67). The function analysis included the study of granzyme B (GzB) and cytokines (IFN, IL2, IL4, IL10, IL17, TNF) secretion. (A) Phenotype and function analysis of MAIT cells in SSc compared to controls. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc (n=29) and healthy donors (n = 23). Red dashed circles represent p values. (B) Phenotype and function analysis of MAIT cells in SSc with ILD compared to SSc without ILD. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc with ILD (n=24) and SSc without ILD (n=50). Red dashed circles represent p values.
Phenotype and function analysis of MAIT cells. The phenotype analysis included the study of activation (CD69, CD25, CD27), exhaustion (PD1, Tim3), recruitment (CD56, CCR6), survival (Bcl2, CD127) and proliferation (Ki67). The function analysis included the study of granzyme B (GzB) and cytokines (IFN, IL2, IL4, IL10, IL17, TNF) secretion. (A) Phenotype and function analysis of MAIT cells in SSc compared to controls. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc (n=29) and healthy donors (n = 23). Red dashed circles represent p values. (B) Phenotype and function analysis of MAIT cells in SSc with ILD compared to SSc without ILD. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc with ILD (n=24) and SSc without ILD (n=50). Red dashed circles represent p values.
Test: Mann-Whitney. * p ≤ 0, 05, ** p ≤ 0, 01, *** p ≤ 0, 001. SSc: Systemic Sclerosis. ILD: Interstitial Lung Disease . Bcl: B-cell lymphoma. CD: Cluster de Différentiation. CCR: C-C Motif Chemokine Receptor. IFN: Interferon. IL: Interleukine. GzB: Granzyme B. PD1: Programmed cell Death protein 1. TNF: Tumor Necrosis Factor.
Disclosures: M. Lesturgie-Talarek, None; V. Gonzalez, None; C. Frantz, None; N. Sénot, None; Z. Gouda, None; C. Rousseau, None; L. Beaudoin, None; A. Lehuen, None; J. Avouac, Galapagos, AbbVie, Lilly, Pfizer, Bristol Myers Squibb, Novartis, Fresenius-Kabi, Sanofi, Sandoz, Nordic Pharma, Biogen, Medac, Janssen, Roche-Chugai; Y. Allanore, Boehringer Ingelheim, Sanofi, Janssen, AbbVie/Abbott, Menarini, Curzion, Medsenic, Prometheus, AstraZeneca.
Background/Purpose: Systemic sclerosis (SSc) is an autoimmune disease characterized by fibrosis of the skin and internal organs such as the lung. Mucosal-associated invariant T (MAIT) cells are innate-like T lymphocytes able to produce various cytokines and cytotoxic mediators such as granzyme B. Decreased level and altered phenotype of MAIT cell have been shown in various autoimmune disease. Moreover, some data support a potential role in fibrotic disorders as highlighted in liver fibrosis. Therefore, we herein addressed the question as whether MAIT cells may have an altered profile in systemic sclerosis.
Our objective was to determine the implication of MAIT cells in SSc.
Methods: MAIT cell frequency was analyzed by flow cytometry, using fresh peripheral blood from 74 consecutive SSc patients compared to 44 healthy donors. In addition, in depth MAIT cell phenotype and function were analyzed using fresh peripheral blood from 29 women with SSc compared to 23 healthy women donors.
Results: Most of the healthy donors were female (95%) and the mean age was 45.6 years. Among the 74 SSc patients (89% were female, mean age: 57 years), the mean disease duration was 9 years, 42% had diffuse cutaneous SSc and 48% had an interstitial lung disease (ILD). Proportion of circulating MAIT cell frequency was significantly reduced by 55% in SSc compared to healthy donors (1.4 % vs. 3.1%, p< 0.0001) (Figure 1A). We next investigated whether MAIT cell frequency was associated with clinical variables in SSc patients. MAIT cell frequency was significantly reduced in patients with interstitial lung disease (SSc-ILD) (0.49% vs. 0.91% in patients without ILD, p=0.027) (Figure 1B) even lower in the patients with severe ILD and reduced forced vital capacity (FVC) (0.25% in patients with FVC < 75% vs. 0.94% in patients with FVC >75%). Deficiency of MAIT cells did not correlate with disease activity score, type of SSc (diffuse or limited), systemic inflammation, and current immunosuppressive therapy.
In SSc patients, MAIT cells displayed a strongly activated phenotype indicated by markedly increased CD69+ MAIT cell frequency compared to healthy donors (p=0.0015, Figure 2A). Decreased proportion of MAIT expressing the anti-apoptotic marker Bcl2 was also observed. Regarding the cytokine profile analysis, no difference was observed compared to healthy controls (Figure 2A). Interestingly, MAIT cells from SSc-ILD patients had a more pronounced altered phenotype compared to SSc without ILD, with a correlation between MAIT expressing CCR6+ and MAIT frequency and a decreased production of IFN-γ (Figure 2B).
Conclusion: Circulating MAIT cells were reduced and exhibited an activated and pro-apoptotic phenotype in SSc patients compared to healthy controls. This peripheral MAIT cell deficiency may be related to enhanced apoptosis and/or homing in inflamed tissue, in particular the lung in SSc-ILD patients. Indeed, peripheral MAIT decrease was even more pronounced in SSc-ILD patients, and correlated with the expression of the tissue-recruitment chemokine CCR6. MAIT cells study in lung tissue as well as functional studies are necessary to better understand the implication of MAIT cells in systemic sclerosis.
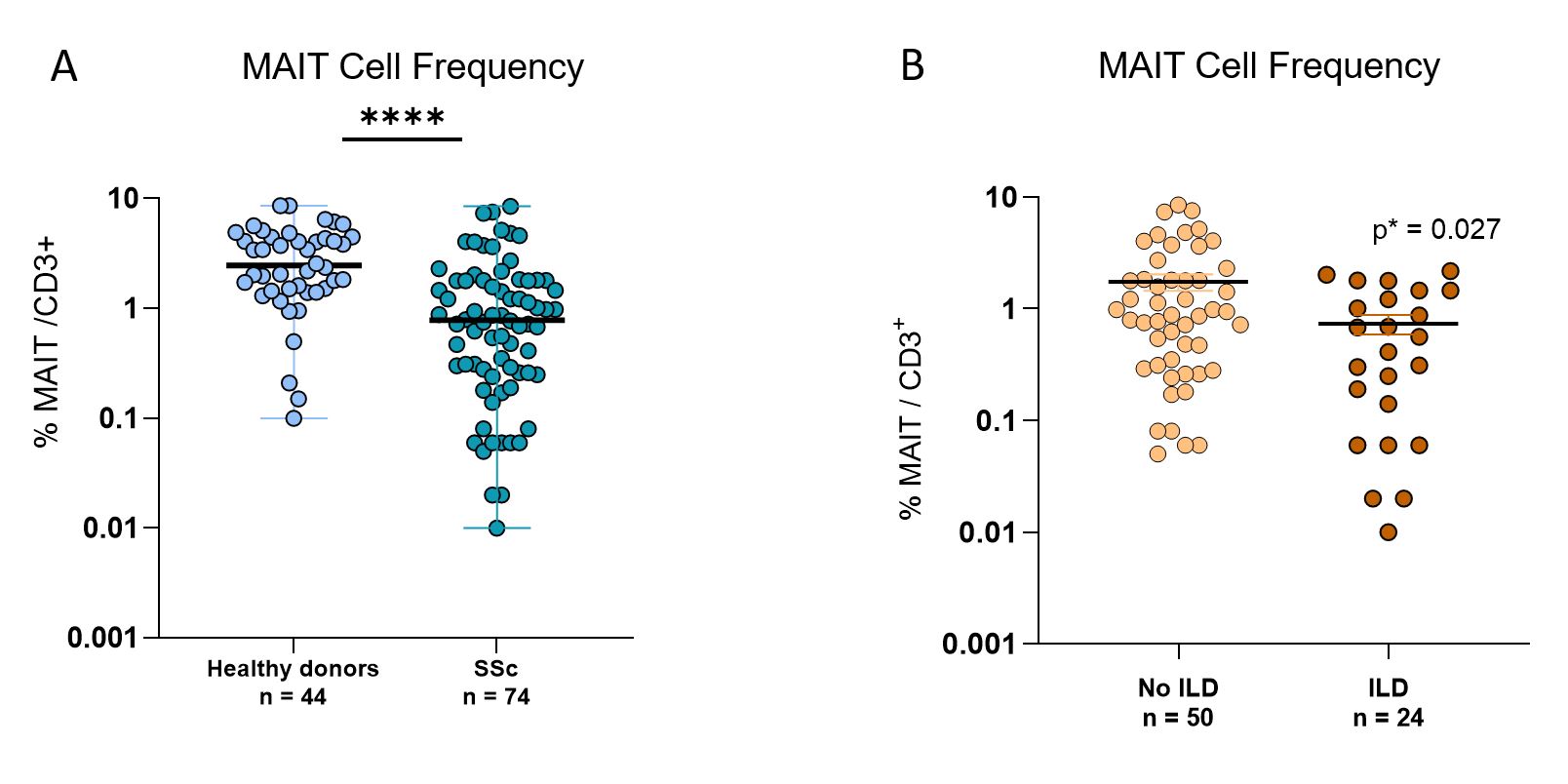 MAIT cell frequency. (A) MAIT cell frequency in SSc (n=74) compared to healthy donors (n=44). (B) MAIT cell frequency in SSc with ILD (n=24) compared to SSc without ILD (n=50). ILD: interstitial lung disease. SSc: systemic sclerosis. Test: Mann-Whitney. **** p < 0.0001.
MAIT cell frequency. (A) MAIT cell frequency in SSc (n=74) compared to healthy donors (n=44). (B) MAIT cell frequency in SSc with ILD (n=24) compared to SSc without ILD (n=50). ILD: interstitial lung disease. SSc: systemic sclerosis. Test: Mann-Whitney. **** p < 0.0001. .jpg) Phenotype and function analysis of MAIT cells. The phenotype analysis included the study of activation (CD69, CD25, CD27), exhaustion (PD1, Tim3), recruitment (CD56, CCR6), survival (Bcl2, CD127) and proliferation (Ki67). The function analysis included the study of granzyme B (GzB) and cytokines (IFN, IL2, IL4, IL10, IL17, TNF) secretion. (A) Phenotype and function analysis of MAIT cells in SSc compared to controls. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc (n=29) and healthy donors (n = 23). Red dashed circles represent p values. (B) Phenotype and function analysis of MAIT cells in SSc with ILD compared to SSc without ILD. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc with ILD (n=24) and SSc without ILD (n=50). Red dashed circles represent p values.
Phenotype and function analysis of MAIT cells. The phenotype analysis included the study of activation (CD69, CD25, CD27), exhaustion (PD1, Tim3), recruitment (CD56, CCR6), survival (Bcl2, CD127) and proliferation (Ki67). The function analysis included the study of granzyme B (GzB) and cytokines (IFN, IL2, IL4, IL10, IL17, TNF) secretion. (A) Phenotype and function analysis of MAIT cells in SSc compared to controls. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc (n=29) and healthy donors (n = 23). Red dashed circles represent p values. (B) Phenotype and function analysis of MAIT cells in SSc with ILD compared to SSc without ILD. Circular bar plot represents negative logarithmic p values of MAIT cell phenotype and function differences between SSc with ILD (n=24) and SSc without ILD (n=50). Red dashed circles represent p values.Test: Mann-Whitney. * p ≤ 0, 05, ** p ≤ 0, 01, *** p ≤ 0, 001. SSc: Systemic Sclerosis. ILD: Interstitial Lung Disease . Bcl: B-cell lymphoma. CD: Cluster de Différentiation. CCR: C-C Motif Chemokine Receptor. IFN: Interferon. IL: Interleukine. GzB: Granzyme B. PD1: Programmed cell Death protein 1. TNF: Tumor Necrosis Factor.
Disclosures: M. Lesturgie-Talarek, None; V. Gonzalez, None; C. Frantz, None; N. Sénot, None; Z. Gouda, None; C. Rousseau, None; L. Beaudoin, None; A. Lehuen, None; J. Avouac, Galapagos, AbbVie, Lilly, Pfizer, Bristol Myers Squibb, Novartis, Fresenius-Kabi, Sanofi, Sandoz, Nordic Pharma, Biogen, Medac, Janssen, Roche-Chugai; Y. Allanore, Boehringer Ingelheim, Sanofi, Janssen, AbbVie/Abbott, Menarini, Curzion, Medsenic, Prometheus, AstraZeneca.

