Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1481: Dementia in Adults with Systemic Lupus Erythematosus 65 Years of Age and Above: A National Administrative Claims Data Analysis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Sarah Lieber, MD, MS
Hospital for Special Surgery
New York, NY, United States
Abstract Poster Presenter(s)
Sarah Lieber1, Musarrat Nahid2, Iris Navarro-Millan2, Mangala Rajan2, Sebastian Sattui3, Robyn Lipschultz1, M. Carrington Reid2 and Lisa Mandl1, 1Hospital for Special Surgery, New York, NY, 2Weill Cornell Medicine, New York, NY, 3University of Pittsburgh, Pittsburgh, PA
Background/Purpose: Systemic lupus erythematosus (SLE) has been associated with increased risk of dementia relative to age-matched comparators without systemic rheumatic disease (SRD) in non-US-based samples including primarily young and mid-aged adults [1-4]. Dementia prevalence in aging adults with SLE in the US population is not well understood. Using a national administrative claims dataset, we sought to ascertain dementia prevalence in adults with SLE ≥65 years of age compared to age- and gender-matched non-SRD comparators and differences in clinical characteristics between these groups.
Methods: We identified patients with SLE ≥65 years of age enrolled in a 5% random sample of Centers for Medicare and Medicaid Services Medicare in 2006 based on ≥2 International Classification of Diseases, Ninth Revision (ICD-9) codes (710.0) from hospital discharge diagnoses or physician visit claims, with each claim separated by ≥30 days. Age- and gender-matched comparators with osteoarthritis (≥1 ICD-9 code of 715), but no SRD were identified in a 4:1 ratio. Dementia prevalence was determined using a previously validated algorithm [5]: ≥1 inpatient dementia claim (ICD-9 code of 290.xx, 294.1x, or 331.xx), ≥2 outpatient claims, or prescription of a dementia-specific medication (rivastigmine, galantamine, memantine, donepezil, or tacrine). Sociodemographic features, comorbid conditions, and medications were assessed for patients with SLE and non-SRD comparators.
Results: In this cross-sectional study, we identified 1338 patients with SLE and 5352 matched comparators without SRD. Participants were predominantly female (88.1%), with median age of 73.4 years. Patients with SLE had greater comorbidity burden, higher prevalence of cardiovascular disease (CVD) despite lower prevalence of traditional CVD risk factors (diabetes mellitus, hyperlipidemia), and higher proportion of hydroxychloroquine, glucocorticoid, and immunosuppressive medication use than non-SRD comparators (all p< 0.01). Dementia prevalence did not differ significantly between patients with SLE (4.8%) and non-SRD comparators (5.8%).
Conclusion: In contrast to prior studies of non-US-based samples including primarily young and mid-aged adults, dementia prevalence was similar between older adults with SLE and non-SRD comparators in this US-based sample. Further study is underway to examine secular trends in dementia prevalence among aging US adults with and without SLE.
References:
1. Lin et al. Arthritis Care Res 2016;68:1774-9.
2. Wotton and Goldacre. J Epidemiol Community Health 2017;71:576-83.
3. Gendelman et al. Int J Geriatr Psychiatry 2018;33:531-6.
4. Zhao et al. Dement Neuropsychol 2018;12:143-51.
5. Sattui et al. Semin Arthritis Rheum 2021;51:292-8.
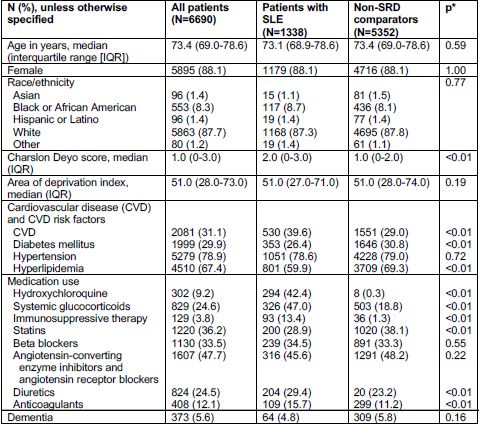 Table 1. Prevalence of dementia and sociodemographic and clinical characteristics in patients with systemic lupus erythematosus (SLE) and non-systemic rheumatic disease (SRD) comparators
Table 1. Prevalence of dementia and sociodemographic and clinical characteristics in patients with systemic lupus erythematosus (SLE) and non-systemic rheumatic disease (SRD) comparators
Disclosures: S. Lieber, None; M. Nahid, None; I. Navarro-Millan, Sweden Orphan Biovitrum (SOBI); M. Rajan, None; S. Sattui, AstraZeneca; R. Lipschultz, None; M. Reid, None; L. Mandl, Pfizer.
Background/Purpose: Systemic lupus erythematosus (SLE) has been associated with increased risk of dementia relative to age-matched comparators without systemic rheumatic disease (SRD) in non-US-based samples including primarily young and mid-aged adults [1-4]. Dementia prevalence in aging adults with SLE in the US population is not well understood. Using a national administrative claims dataset, we sought to ascertain dementia prevalence in adults with SLE ≥65 years of age compared to age- and gender-matched non-SRD comparators and differences in clinical characteristics between these groups.
Methods: We identified patients with SLE ≥65 years of age enrolled in a 5% random sample of Centers for Medicare and Medicaid Services Medicare in 2006 based on ≥2 International Classification of Diseases, Ninth Revision (ICD-9) codes (710.0) from hospital discharge diagnoses or physician visit claims, with each claim separated by ≥30 days. Age- and gender-matched comparators with osteoarthritis (≥1 ICD-9 code of 715), but no SRD were identified in a 4:1 ratio. Dementia prevalence was determined using a previously validated algorithm [5]: ≥1 inpatient dementia claim (ICD-9 code of 290.xx, 294.1x, or 331.xx), ≥2 outpatient claims, or prescription of a dementia-specific medication (rivastigmine, galantamine, memantine, donepezil, or tacrine). Sociodemographic features, comorbid conditions, and medications were assessed for patients with SLE and non-SRD comparators.
Results: In this cross-sectional study, we identified 1338 patients with SLE and 5352 matched comparators without SRD. Participants were predominantly female (88.1%), with median age of 73.4 years. Patients with SLE had greater comorbidity burden, higher prevalence of cardiovascular disease (CVD) despite lower prevalence of traditional CVD risk factors (diabetes mellitus, hyperlipidemia), and higher proportion of hydroxychloroquine, glucocorticoid, and immunosuppressive medication use than non-SRD comparators (all p< 0.01). Dementia prevalence did not differ significantly between patients with SLE (4.8%) and non-SRD comparators (5.8%).
Conclusion: In contrast to prior studies of non-US-based samples including primarily young and mid-aged adults, dementia prevalence was similar between older adults with SLE and non-SRD comparators in this US-based sample. Further study is underway to examine secular trends in dementia prevalence among aging US adults with and without SLE.
References:
1. Lin et al. Arthritis Care Res 2016;68:1774-9.
2. Wotton and Goldacre. J Epidemiol Community Health 2017;71:576-83.
3. Gendelman et al. Int J Geriatr Psychiatry 2018;33:531-6.
4. Zhao et al. Dement Neuropsychol 2018;12:143-51.
5. Sattui et al. Semin Arthritis Rheum 2021;51:292-8.
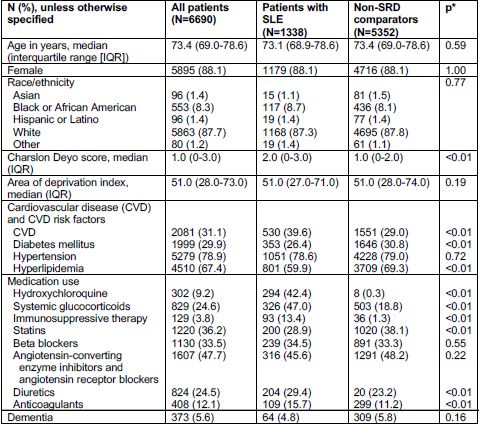 Table 1. Prevalence of dementia and sociodemographic and clinical characteristics in patients with systemic lupus erythematosus (SLE) and non-systemic rheumatic disease (SRD) comparators
Table 1. Prevalence of dementia and sociodemographic and clinical characteristics in patients with systemic lupus erythematosus (SLE) and non-systemic rheumatic disease (SRD) comparatorsDisclosures: S. Lieber, None; M. Nahid, None; I. Navarro-Millan, Sweden Orphan Biovitrum (SOBI); M. Rajan, None; S. Sattui, AstraZeneca; R. Lipschultz, None; M. Reid, None; L. Mandl, Pfizer.

