Back
Poster Session A
Epidemiology, health policy and outcomes
Session: (0056–0084) Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
0082: Impact of the COVID-19 Pandemic on Healthcare Utilization Among Rheumatoid Arthritis, Psoriatic Arthritis and Systemic Lupus Erythematosus Patients
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JP
Jean Park, MD
CVS Health
Hartford, CT, United States
Abstract Poster Presenter(s)
Jean Park, W. Cliff Rutter, Will Cavers, Elisea Avalos-Reyes and Kjel Johnson, CVS Health, Lincoln, RI
Background/Purpose: Patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA) and systemic lupus erythematosus (SLE) are considered at risk for serious COVID infections due to their immunocompromised state resulting from their underlying immune conditions and the use of targeted immune-modulating therapies such as biologics. This study aims to examine how COVID-19 impacted healthcare utilization in these patients.
Methods: Adult patients with a visit for RA (International Classification of Diseases 10 (ICD-10) Diagnosis Code M05.x or M06.x), PsA (L40.5x) or SLE (M32.x) between 3/1/2019 and 3/1/2021 were eligible for inclusion in this retrospective cohort study. Patients were excluded if they did not maintain eligibility for the entire study period. Healthcare utilization was examined as an aggregate of emergency room (ER) visits, inpatient hospitalizations, mental health visits and DMARD prescriptions before and after 3/1/2020 as the pre-COVID and COVID periods, respectively. Monthly rates were compared between periods. P-values < 0.05 were significant.
Results: A total of 32,712 patients were included in the study with 24,613 (75.2%) having RA, 3,748 (11.5%) having PsA and 4,351 (13.3%) having SLE. Monthly ER visit rates (mean [standard deviation (SD)]: 62.6 [11.1] visits/1,000 patients vs. 34.1 [3.9] visits/1,000 patients in pre-COVID and COVID periods, respectively; p< 0.00001), inpatient stays (mean [SD]: 29.1 [4.9] stays/1,000 patients vs. 17.9 [2.0] stays/1,000 patients; p< 0.00001) and mental health visits (mean [SD]: 9.3 [2.1] visits/1,000 patients vs. 7.1 [0.5] visits/1,000 patients; p=0.002) were higher in the pre-COVID period. Figure 1 shows the rates for each type of utilization over the study period. The rates for ER visits and inpatient stays are significantly lower following the onset of the pandemic, while mental health visits appear to be stable at a lower rate. Additionally, the monthly average number of patients utilizing the ER (mean [SD]: 1056.1 [44.5] patients vs. 819.3 [104.2] patients; p< 0.00001) or inpatient services (mean [SD]: 502.2 [30.3] patient vs. 451.1 [66.2] patients; p=0.02) were significantly lower in the COVID period, while no difference was found in the number of mental health service utilizers between periods (mean [SD] 98.6 [9.6] patients vs. 91.5 [9.7] patients; p=0.09). The monthly number of DMARD prescriptions was significantly higher in the COVID period (mean [SD]: 8,791.7 [286.0] fills vs. 9,421.33 [472.0] fills; p=0.0007). The number of DMARD users was similarly elevated in the COVID period (mean [SD]: 7,079.2 [161.8] users vs. 7,554.3 [259.8] users; p=0.00002).
Conclusion: Healthcare utilization was significantly higher in the pre-COVID period on average. The beginning of the pandemic was characterized by lower utilization which rebounded to lower-than-average utilization for the remaining time of the COVID period.
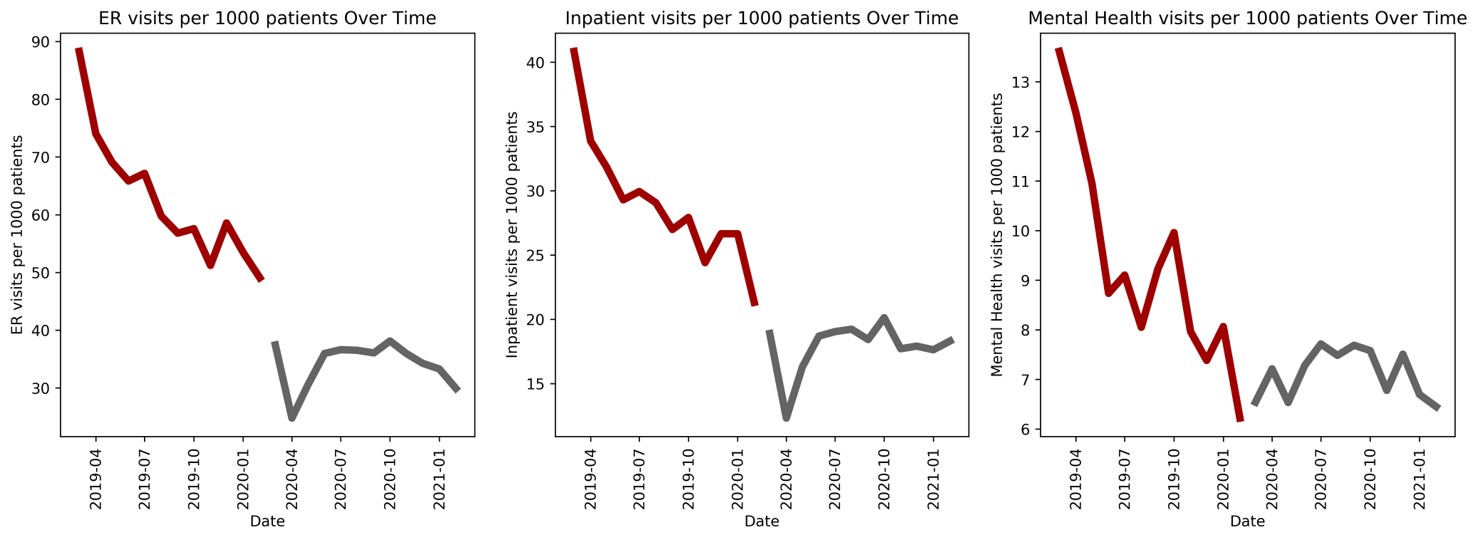 Figure 1: Monthly healthcare utilization rates
Figure 1: Monthly healthcare utilization rates
Disclosures: J. Park, CVS Health; W. Rutter, CVS Health; W. Cavers, CVS Health, Amedisys Inc., Baxter International, Conmed Corp; E. Avalos-Reyes, CVS Health, Novartis, Pfizer, Moderna, Johnson & Johnson, AstraZeneca, GlaxoSmithKlein(GSK), Viatris; K. Johnson, CVS Health, IQVia.
Background/Purpose: Patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA) and systemic lupus erythematosus (SLE) are considered at risk for serious COVID infections due to their immunocompromised state resulting from their underlying immune conditions and the use of targeted immune-modulating therapies such as biologics. This study aims to examine how COVID-19 impacted healthcare utilization in these patients.
Methods: Adult patients with a visit for RA (International Classification of Diseases 10 (ICD-10) Diagnosis Code M05.x or M06.x), PsA (L40.5x) or SLE (M32.x) between 3/1/2019 and 3/1/2021 were eligible for inclusion in this retrospective cohort study. Patients were excluded if they did not maintain eligibility for the entire study period. Healthcare utilization was examined as an aggregate of emergency room (ER) visits, inpatient hospitalizations, mental health visits and DMARD prescriptions before and after 3/1/2020 as the pre-COVID and COVID periods, respectively. Monthly rates were compared between periods. P-values < 0.05 were significant.
Results: A total of 32,712 patients were included in the study with 24,613 (75.2%) having RA, 3,748 (11.5%) having PsA and 4,351 (13.3%) having SLE. Monthly ER visit rates (mean [standard deviation (SD)]: 62.6 [11.1] visits/1,000 patients vs. 34.1 [3.9] visits/1,000 patients in pre-COVID and COVID periods, respectively; p< 0.00001), inpatient stays (mean [SD]: 29.1 [4.9] stays/1,000 patients vs. 17.9 [2.0] stays/1,000 patients; p< 0.00001) and mental health visits (mean [SD]: 9.3 [2.1] visits/1,000 patients vs. 7.1 [0.5] visits/1,000 patients; p=0.002) were higher in the pre-COVID period. Figure 1 shows the rates for each type of utilization over the study period. The rates for ER visits and inpatient stays are significantly lower following the onset of the pandemic, while mental health visits appear to be stable at a lower rate. Additionally, the monthly average number of patients utilizing the ER (mean [SD]: 1056.1 [44.5] patients vs. 819.3 [104.2] patients; p< 0.00001) or inpatient services (mean [SD]: 502.2 [30.3] patient vs. 451.1 [66.2] patients; p=0.02) were significantly lower in the COVID period, while no difference was found in the number of mental health service utilizers between periods (mean [SD] 98.6 [9.6] patients vs. 91.5 [9.7] patients; p=0.09). The monthly number of DMARD prescriptions was significantly higher in the COVID period (mean [SD]: 8,791.7 [286.0] fills vs. 9,421.33 [472.0] fills; p=0.0007). The number of DMARD users was similarly elevated in the COVID period (mean [SD]: 7,079.2 [161.8] users vs. 7,554.3 [259.8] users; p=0.00002).
Conclusion: Healthcare utilization was significantly higher in the pre-COVID period on average. The beginning of the pandemic was characterized by lower utilization which rebounded to lower-than-average utilization for the remaining time of the COVID period.
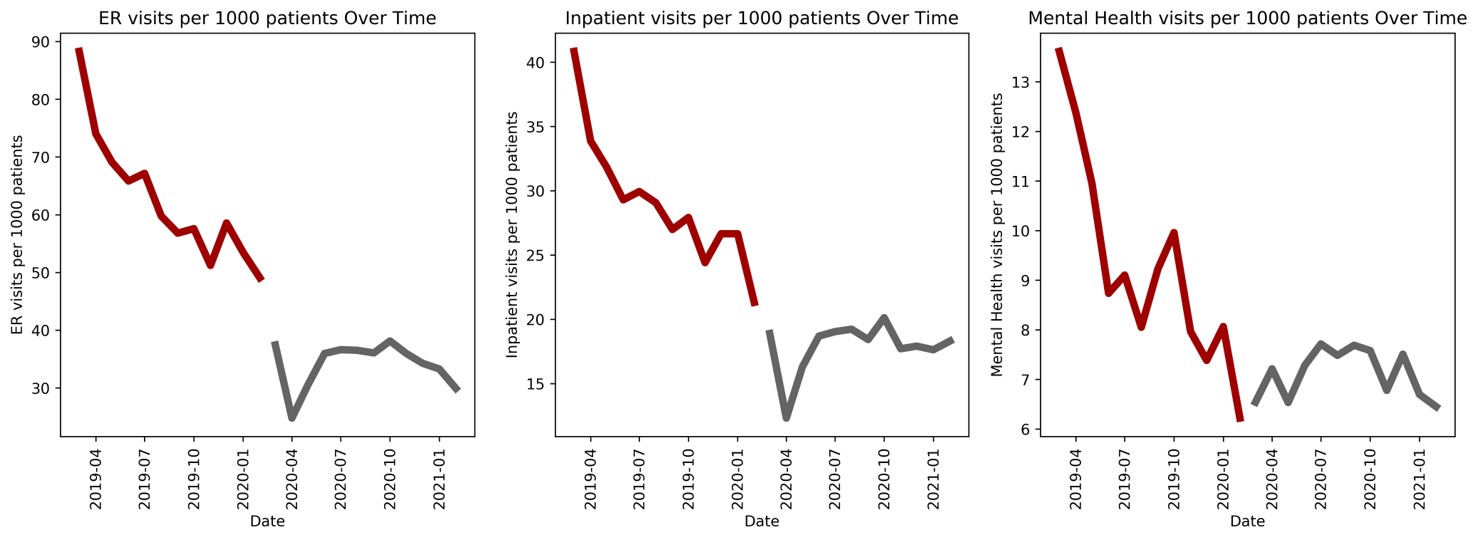 Figure 1: Monthly healthcare utilization rates
Figure 1: Monthly healthcare utilization ratesDisclosures: J. Park, CVS Health; W. Rutter, CVS Health; W. Cavers, CVS Health, Amedisys Inc., Baxter International, Conmed Corp; E. Avalos-Reyes, CVS Health, Novartis, Pfizer, Moderna, Johnson & Johnson, AstraZeneca, GlaxoSmithKlein(GSK), Viatris; K. Johnson, CVS Health, IQVia.

