Back
Abstract Session
Systemic lupus erythematosus (SLE)
Session: Abstracts: SLE – Diagnosis, Manifestations, and Outcomes II: Complications (1591–1596)
1592: Serious Infections in SLE- Incidence, Associated Factors, Impact and Trends over Two Decades
Sunday, November 13, 2022
3:15 PM – 3:25 PM Eastern Time
Location: Room 204
- AA
Amita Aggarwal, MD, MBBS, DM
Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
Lucknow, Uttar Pradesh, India
Presenting Author(s)
Rudrarpan Chatterjee, Sarit Sekhar Pattanaik, Durga P Misra, Vikas Agarwal, Able Lawrence and Amita Aggarwal, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
Background/Purpose: Infections are a major cause of morbidity and mortality in systemic lupus erythematosus (SLE). We assessed the incidence and risk factors for major infections in adult SLE.
Methods: We carried out a retrospective review of 1354 patients of SLE (ACR 1997 criteria) with age ≥18 years visiting the rheumatology clinic at a single centre between 2000 to 2020. Clinical details were retrieved from clinical case records and supplemented with data from the hospital electronic health records. Serious infection was defined as the need for hospitalization, or infection resulting in disability or death. Cox regression was used to determine factors associated with a serious infection and the effect of each serious infection on overall survival.
Results: Among the 1354 patients (1258 females) with a mean age of 30.32 ±9.42 years and a cumulative follow up of 7127.89 person-years. A total of 439 major infections occurred in 339 (25.03% of the cohort) individuals at a rate of 61.6 serious infections per 1000 person-years of follow-up. Recurrent infections occurred in 101 (7.45%) patients. The average number of infections increased from 9.9 to 23.7 per year from 2000-09 to 2010-19.
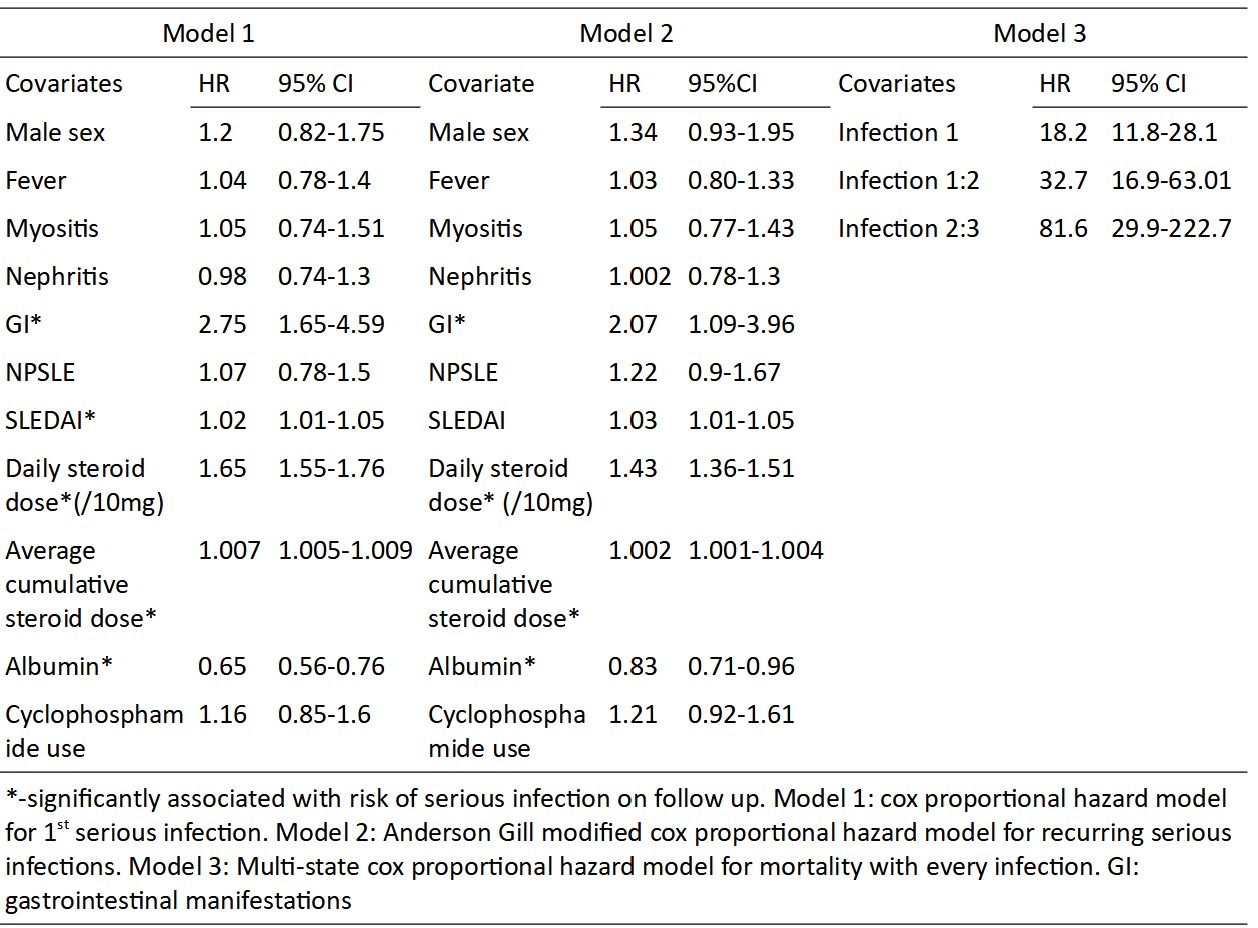
Among the microbiologically confirmed cases (79.9% of cases) Tuberculosis (81) was the most common organism followed by S. aureus (65), E. coli (51), K. pneumoniae (29), P. aeruginosa (29), S. pneumoniae (20), Acinetobacter spp. (9), E. fecalis (9), Nocardia (4), Salmonella (3), Proteus (1) and Listeria (1). Forty (9.1%) opportunistic infections occurred: Cytomegalovirus (11), disseminated Herpes zoster (10), invasive candidiasis (5), cryptococcal meningitis (5), histoplasmosis (2), and 1 each of Aspergillus flavus pneumonia, CNS toxoplasmosis and Giardia lamblia. On multivariate analysis SLEDAI-2K(HR 1.02, 1.01-1.05), gastrointestinal involvement (HR 2.75, 1.65-4.69), current steroid dose (HR 1.65,1.55-1.76), average cumulative steroid dose per year (HR 1.007, 1.005-1.009) were associated with serious infection and higher albumin (HR 0.65, 0.56-0.76) was protective.
Serious infection led to more damage accrual (1 vs 0). Serious infection-free survival at 1 year and 5 years was 82.9% (80.8-85) and 73.8% (71.1-76.6). There were 119 deaths with infection attributable mortality in 65 (54.6%). Hazard ratio for mortality was 18.2, 32.7, and 81.6 for the first, second, and third serious infection.
Conclusion: Serious infections remain a major cause of mortality and damage accrual in SLE and are associated with higher disease activity, gastrointestinal involvement, hypoalbuminemia, current and cumulative steroid dose. TB prophylaxis in patients with SLE should be considered in endemic areas, especially when using high-dose steroid therapy.
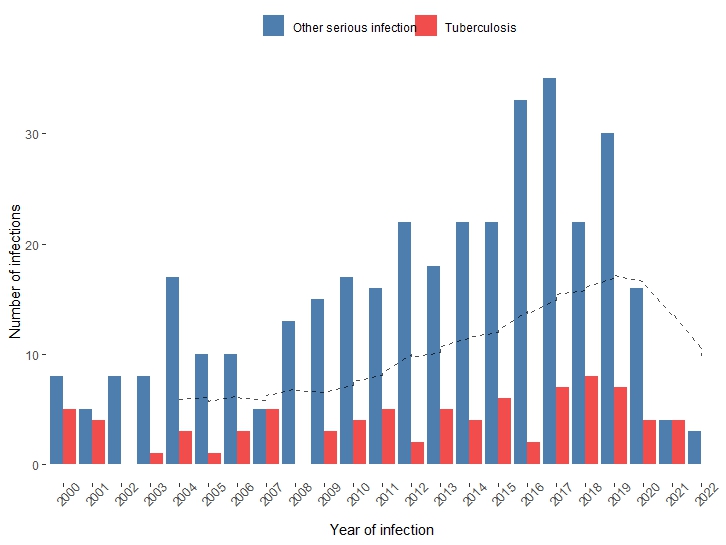 The bar diagram depicts the number of instances of tuberculosis per year compared to other serious infections from the year 200 to 2022. The dashed line represents the 10 year moving average of all serious infections in the cohort and shows a consistently increasing trend.
The bar diagram depicts the number of instances of tuberculosis per year compared to other serious infections from the year 200 to 2022. The dashed line represents the 10 year moving average of all serious infections in the cohort and shows a consistently increasing trend.
Disclosures: R. Chatterjee, None; S. Pattanaik, None; D. Misra, None; V. Agarwal, None; A. Lawrence, None; A. Aggarwal, None.
Background/Purpose: Infections are a major cause of morbidity and mortality in systemic lupus erythematosus (SLE). We assessed the incidence and risk factors for major infections in adult SLE.
Methods: We carried out a retrospective review of 1354 patients of SLE (ACR 1997 criteria) with age ≥18 years visiting the rheumatology clinic at a single centre between 2000 to 2020. Clinical details were retrieved from clinical case records and supplemented with data from the hospital electronic health records. Serious infection was defined as the need for hospitalization, or infection resulting in disability or death. Cox regression was used to determine factors associated with a serious infection and the effect of each serious infection on overall survival.
Results: Among the 1354 patients (1258 females) with a mean age of 30.32 ±9.42 years and a cumulative follow up of 7127.89 person-years. A total of 439 major infections occurred in 339 (25.03% of the cohort) individuals at a rate of 61.6 serious infections per 1000 person-years of follow-up. Recurrent infections occurred in 101 (7.45%) patients. The average number of infections increased from 9.9 to 23.7 per year from 2000-09 to 2010-19.
Among the microbiologically confirmed cases (79.9% of cases) Tuberculosis (81) was the most common organism followed by S. aureus (65), E. coli (51), K. pneumoniae (29), P. aeruginosa (29), S. pneumoniae (20), Acinetobacter spp. (9), E. fecalis (9), Nocardia (4), Salmonella (3), Proteus (1) and Listeria (1). Forty (9.1%) opportunistic infections occurred: Cytomegalovirus (11), disseminated Herpes zoster (10), invasive candidiasis (5), cryptococcal meningitis (5), histoplasmosis (2), and 1 each of Aspergillus flavus pneumonia, CNS toxoplasmosis and Giardia lamblia. On multivariate analysis SLEDAI-2K(HR 1.02, 1.01-1.05), gastrointestinal involvement (HR 2.75, 1.65-4.69), current steroid dose (HR 1.65,1.55-1.76), average cumulative steroid dose per year (HR 1.007, 1.005-1.009) were associated with serious infection and higher albumin (HR 0.65, 0.56-0.76) was protective.
Serious infection led to more damage accrual (1 vs 0). Serious infection-free survival at 1 year and 5 years was 82.9% (80.8-85) and 73.8% (71.1-76.6). There were 119 deaths with infection attributable mortality in 65 (54.6%). Hazard ratio for mortality was 18.2, 32.7, and 81.6 for the first, second, and third serious infection.
Conclusion: Serious infections remain a major cause of mortality and damage accrual in SLE and are associated with higher disease activity, gastrointestinal involvement, hypoalbuminemia, current and cumulative steroid dose. TB prophylaxis in patients with SLE should be considered in endemic areas, especially when using high-dose steroid therapy.
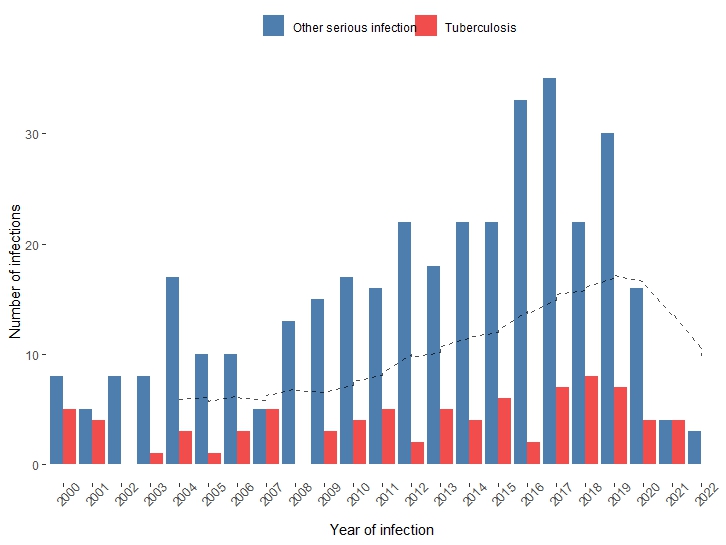 The bar diagram depicts the number of instances of tuberculosis per year compared to other serious infections from the year 200 to 2022. The dashed line represents the 10 year moving average of all serious infections in the cohort and shows a consistently increasing trend.
The bar diagram depicts the number of instances of tuberculosis per year compared to other serious infections from the year 200 to 2022. The dashed line represents the 10 year moving average of all serious infections in the cohort and shows a consistently increasing trend. 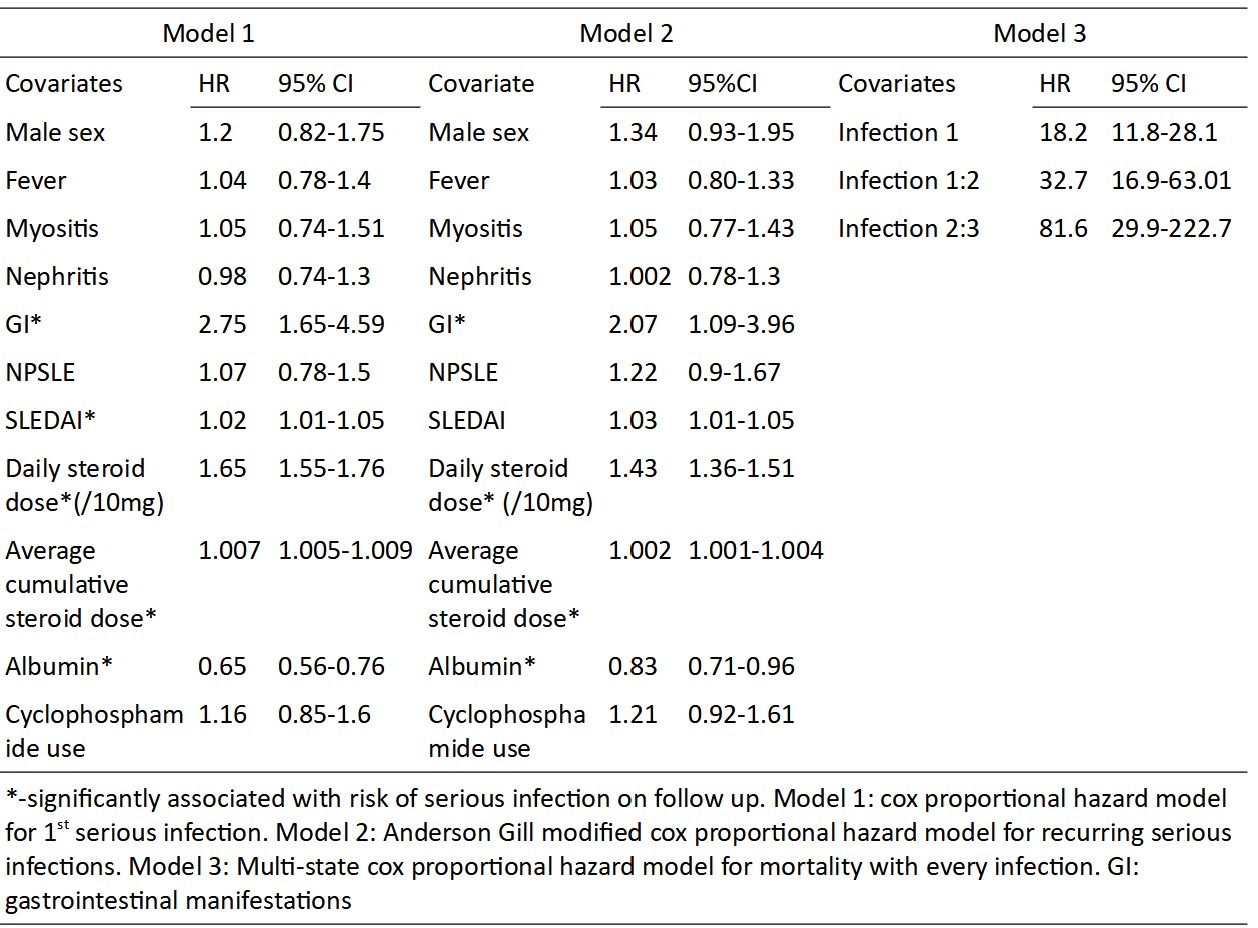
Disclosures: R. Chatterjee, None; S. Pattanaik, None; D. Misra, None; V. Agarwal, None; A. Lawrence, None; A. Aggarwal, None.

