Back
Abstract Session
Systemic lupus erythematosus (SLE)
Session: Abstracts: SLE – Diagnosis, Manifestations, and Outcomes II: Complications (1591–1596)
1596: The Role of Coronary Calcium Screening in Patients with Lupus Who Appear to Be at Low Cardiovascular Risk
Sunday, November 13, 2022
4:15 PM – 4:25 PM Eastern Time
Location: Room 204
- SS
Sarah Stoots, MD, BS
Rheumatology Associates
Philadelphia, PA, United States
Presenting Author(s)
Sarah Stoots1, Joshua Baker1 and Joan Von Feldt2, 1University of Pennsylvania, Philadelphia, PA, 2University of Pennsylvania, Wilmington, DE
Background/Purpose: Patients with Systemic Lupus Erythematosus (SLE) are at elevated cardiovascular risk. However, common risk calculators such as the atherosclerotic cardiovascular disease (ASCVD) risk estimator that are used to determine whether a patient would benefit from statin therapy (often when ASCVD risk ≥ 7.5%) do not incorporate non-traditional risk factors and may underestimate risk in SLE. Cardiac computed tomography (CT) for quantification of coronary artery calcifications (CAC) has been increasingly utilized as a non-invasive imaging modality to aid cardiovascular risk stratification. Published guidelines recommend statin initiation in patients with abnormal CAC. We aimed to determine how many lupus patients traditionally deemed 'low risk' by ASCVD scoring are found to have abnormal CAC and to determine factors associated with CAC in this population. The purpose of this research is to inform clinicians which SLE patients would benefit from CT coronary imaging in order to risk stratify and identify those who should receive statin therapy.
Methods: This is a post-hoc analysis of a prior cohort study.1 Female patients with SLE and matched controls were recruited; clinical and laboratory assessments were conducted, and CT of the coronary arteries was performed. We excluded patients with history of MI, CVA, DM, or LDL ≥190, because cardiology guidelines recommend statin use in these patients. We identified patients with SLE and controls with low ASCVD risk (defined by ASCVD < 7.5%) and determined rates of abnormal CAC within this low-risk category. We used two-sample t-test and two-sample Wilcoxon rank-sum tests in SLE patients with low ASCVD risk to compare various characteristics in those with normal and abnormal calcium scores.
Results: The original study included 165 SLE and 160 age- and sex-matched controls. After excluding those with MI (6), CVA (24), DM (23), or high LDL (11), 129 SLE patients and 141 controls remained. Among the 129 SLE patients, only 6 were high ASCVD risk, and all 6 had abnormal CAC scores (Figure 1). Among 122 SLE at low ASCVD risk, 34/122 (28%) had abnormal CAC (7 with mod-high values). Only 4/34 (12%) of low ASCVD risk with abnormal CAC were taking a statin. Among controls at low ASCVD risk, only 14/129 (11%) had abnormal CAC (none had mod-high values). Among all patients with low ASCVD risk, SLE patients were significantly more likely to have abnormal CAC compared with controls, adjusting for age and race [OR 3.61 (95% CI 1.76, 7.41), p< 0.001]. ASCVD-low risk SLE patients with abnormal CAC were older (47.2 vs 39.7, p=0.0003), with lower GFR (83.6 vs 98.3, p=0.02), longer disease duration (14.3 vs 6.15, p=0.005), higher LDL (117.5 vs 104.2, p=0.04) and total cholesterol (203.7 vs 180.5, p=0.004) compared to patients with normal CAC (Table 1).
Conclusion: Approximately one fourth of SLE patients at low ASVCD risk have abnormal CAC, a substantially higher rate than observed for healthy controls. These data support an approach of screening for CAC in older patients with long-standing SLE even if they are observed to have low ASCVD risk. A low rate of statin use in this population suggests a missed opportunity to improve cardiovascular health through primary prevention.
1Von Feldt JM, et al. Arthritis & Rheumatism 2006
.jpg) Figure 1: Coronary Calcium Scores Amongst SLE Patients and Controls Stratified by ASCVD Risk
Figure 1: Coronary Calcium Scores Amongst SLE Patients and Controls Stratified by ASCVD Risk
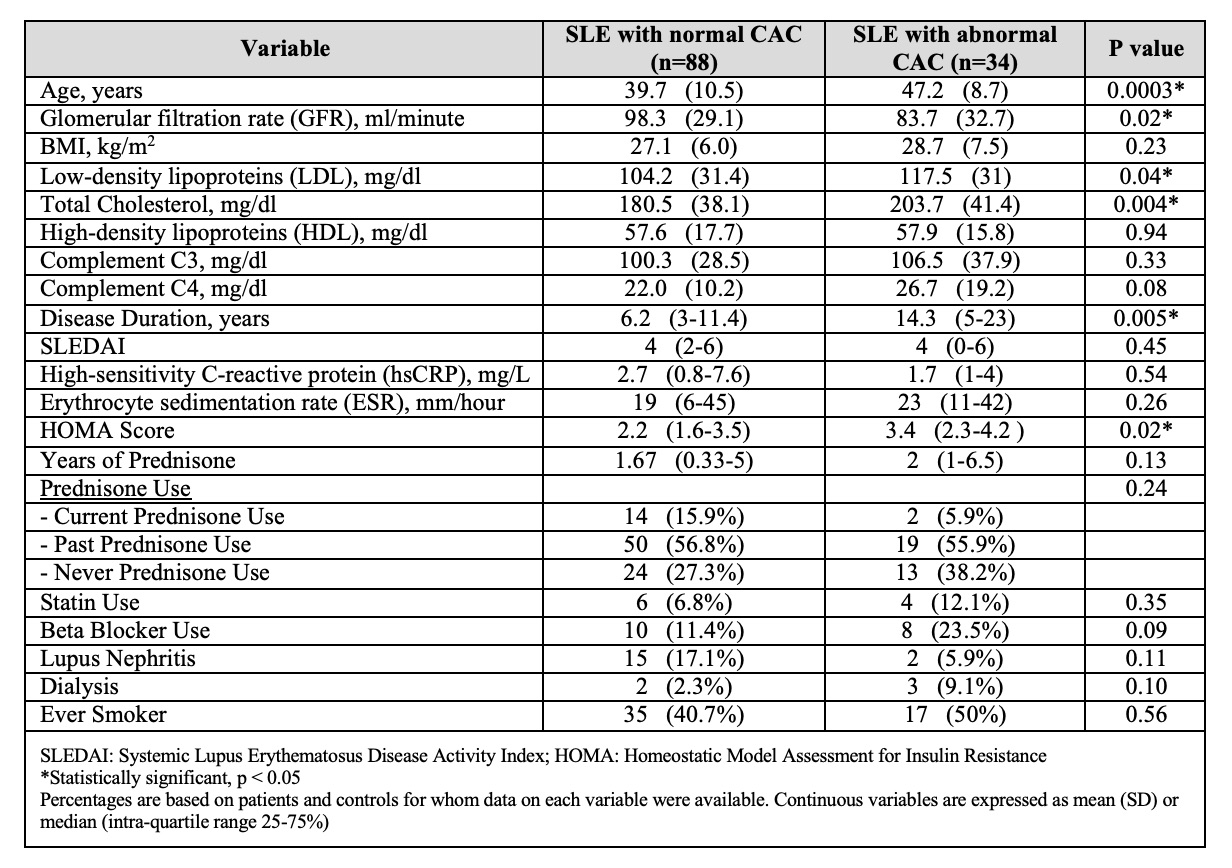 Table 1: Characteristics of SLE Patients at Low ASCVD Risk with CAC and without CAC
Table 1: Characteristics of SLE Patients at Low ASCVD Risk with CAC and without CAC
Disclosures: S. Stoots, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; J. Von Feldt, None.
Background/Purpose: Patients with Systemic Lupus Erythematosus (SLE) are at elevated cardiovascular risk. However, common risk calculators such as the atherosclerotic cardiovascular disease (ASCVD) risk estimator that are used to determine whether a patient would benefit from statin therapy (often when ASCVD risk ≥ 7.5%) do not incorporate non-traditional risk factors and may underestimate risk in SLE. Cardiac computed tomography (CT) for quantification of coronary artery calcifications (CAC) has been increasingly utilized as a non-invasive imaging modality to aid cardiovascular risk stratification. Published guidelines recommend statin initiation in patients with abnormal CAC. We aimed to determine how many lupus patients traditionally deemed 'low risk' by ASCVD scoring are found to have abnormal CAC and to determine factors associated with CAC in this population. The purpose of this research is to inform clinicians which SLE patients would benefit from CT coronary imaging in order to risk stratify and identify those who should receive statin therapy.
Methods: This is a post-hoc analysis of a prior cohort study.1 Female patients with SLE and matched controls were recruited; clinical and laboratory assessments were conducted, and CT of the coronary arteries was performed. We excluded patients with history of MI, CVA, DM, or LDL ≥190, because cardiology guidelines recommend statin use in these patients. We identified patients with SLE and controls with low ASCVD risk (defined by ASCVD < 7.5%) and determined rates of abnormal CAC within this low-risk category. We used two-sample t-test and two-sample Wilcoxon rank-sum tests in SLE patients with low ASCVD risk to compare various characteristics in those with normal and abnormal calcium scores.
Results: The original study included 165 SLE and 160 age- and sex-matched controls. After excluding those with MI (6), CVA (24), DM (23), or high LDL (11), 129 SLE patients and 141 controls remained. Among the 129 SLE patients, only 6 were high ASCVD risk, and all 6 had abnormal CAC scores (Figure 1). Among 122 SLE at low ASCVD risk, 34/122 (28%) had abnormal CAC (7 with mod-high values). Only 4/34 (12%) of low ASCVD risk with abnormal CAC were taking a statin. Among controls at low ASCVD risk, only 14/129 (11%) had abnormal CAC (none had mod-high values). Among all patients with low ASCVD risk, SLE patients were significantly more likely to have abnormal CAC compared with controls, adjusting for age and race [OR 3.61 (95% CI 1.76, 7.41), p< 0.001]. ASCVD-low risk SLE patients with abnormal CAC were older (47.2 vs 39.7, p=0.0003), with lower GFR (83.6 vs 98.3, p=0.02), longer disease duration (14.3 vs 6.15, p=0.005), higher LDL (117.5 vs 104.2, p=0.04) and total cholesterol (203.7 vs 180.5, p=0.004) compared to patients with normal CAC (Table 1).
Conclusion: Approximately one fourth of SLE patients at low ASVCD risk have abnormal CAC, a substantially higher rate than observed for healthy controls. These data support an approach of screening for CAC in older patients with long-standing SLE even if they are observed to have low ASCVD risk. A low rate of statin use in this population suggests a missed opportunity to improve cardiovascular health through primary prevention.
1Von Feldt JM, et al. Arthritis & Rheumatism 2006
.jpg) Figure 1: Coronary Calcium Scores Amongst SLE Patients and Controls Stratified by ASCVD Risk
Figure 1: Coronary Calcium Scores Amongst SLE Patients and Controls Stratified by ASCVD Risk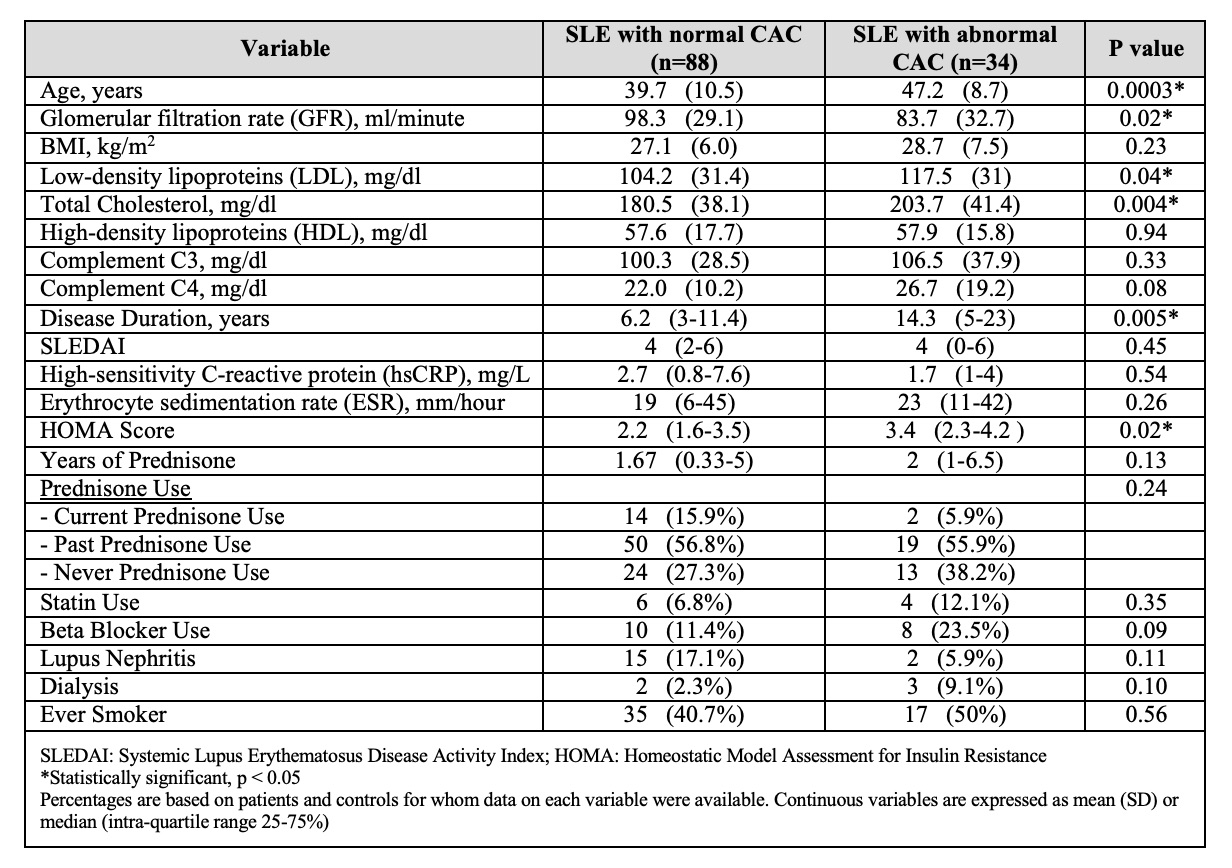 Table 1: Characteristics of SLE Patients at Low ASCVD Risk with CAC and without CAC
Table 1: Characteristics of SLE Patients at Low ASCVD Risk with CAC and without CACDisclosures: S. Stoots, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; J. Von Feldt, None.

