Back
Abstract Session
Vasculitis
Session: Abstracts: Vasculitis – Non-ANCA-Associated and Related Disorders I (1615–1620)
1618: Combined Orbital and Cranial Vessel Wall MRI for Diagnosis and Longitudinal Monitoring of Giant Cell Arteritis
Sunday, November 13, 2022
5:15 PM – 5:25 PM Eastern Time
Location: Ballroom AB
- RR
Rennie Rhee, MD, MS
University of Pennsylvania
Philadelphia, PA, United States
Presenting Author(s)
Rennie Rhee, Shubhasree Banerjee, Vatsal Bhatt, Madhura Tamhankar, Quy Cao, Naomi Amudala, Sherry Chou, Morgan Burke, Laurie Loevner, Peter Merkel and Jae Song, University of Pennsylvania, Philadelphia, PA
Background/Purpose: In giant cell arteritis (GCA), there is a critical need to identify patients at risk for vision loss ("ocular GCA"). MRI evaluates neurovascular anatomy posterior to the ocular globe, an area not visualized by ophthalmologic exam. This study aimed to determine the diagnostic utility of combined orbital and cranial vessel wall MRI in GCA (with or without visual symptoms) and evaluate longitudinal changes in imaging with treatment.
Methods: Patients with suspected new or relapsing cranial GCA who underwent orbital and brain vessel wall MRI were included. Nine patients had repeat imaging at months 1, 6, and 12 to assess changes over time. A clinical diagnosis of ocular or non-ocular GCA was determined by a rheumatologist and/or ophthalmologist and confirmed retrospectively. All MR images were scored by a single radiologist blinded to clinical data. Semi-quantitative integer scores of MRI enhancement were determined: 8 orbital structures were each scored 0, 1, or 2 (score 1-2 defined as abnormal) and included bilateral optic nerve sheath, optic nerve, intraconal orbital fat, and retrobulbar fat of posterior globe; 8 cranial arteries were each scored 0, 1, 2, or 3 (score 2-3 defined as abnormal) and included bilateral temporal arteries (stem, frontal, and parietal branches) and occipital arteries. MRI was considered diagnostic for GCA if at least 1 orbital or cranial artery had abnormal enhancement. Test characteristics were determined. Mixed-effects models were used to compare changes in scores over time between arteries that were abnormal vs normal at baseline.
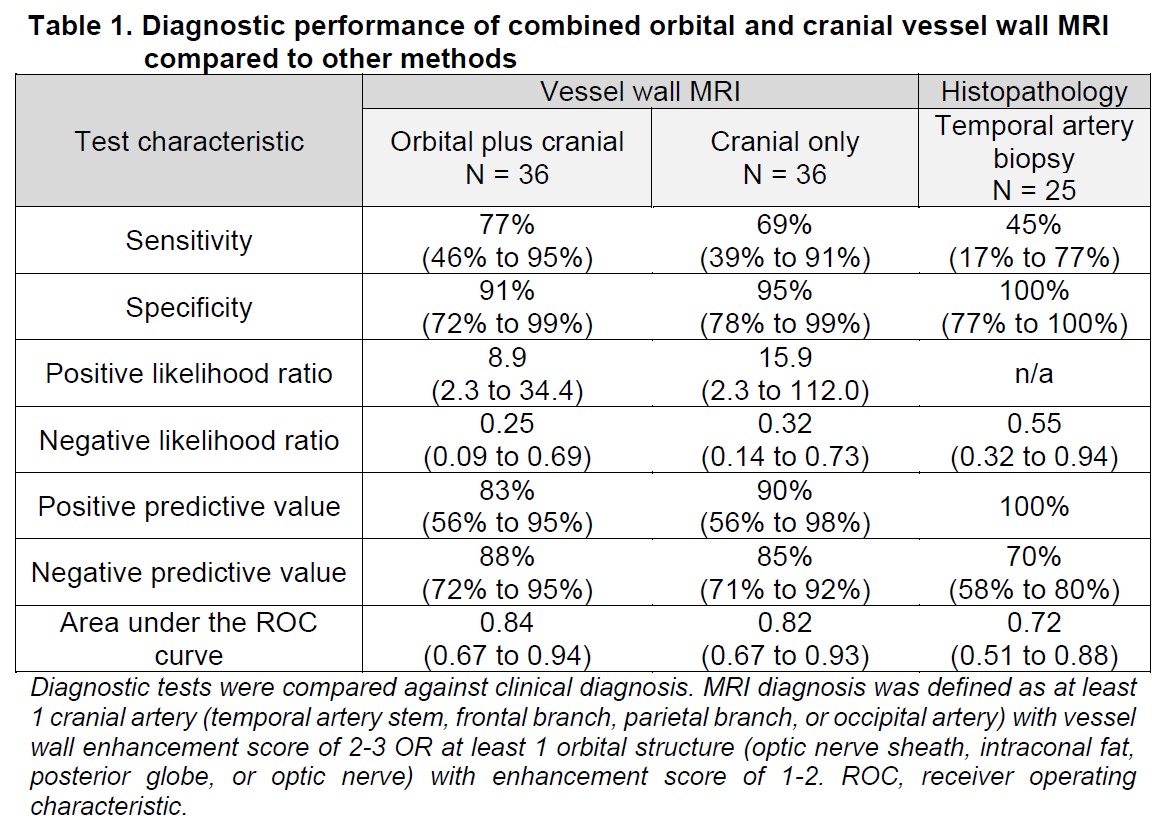
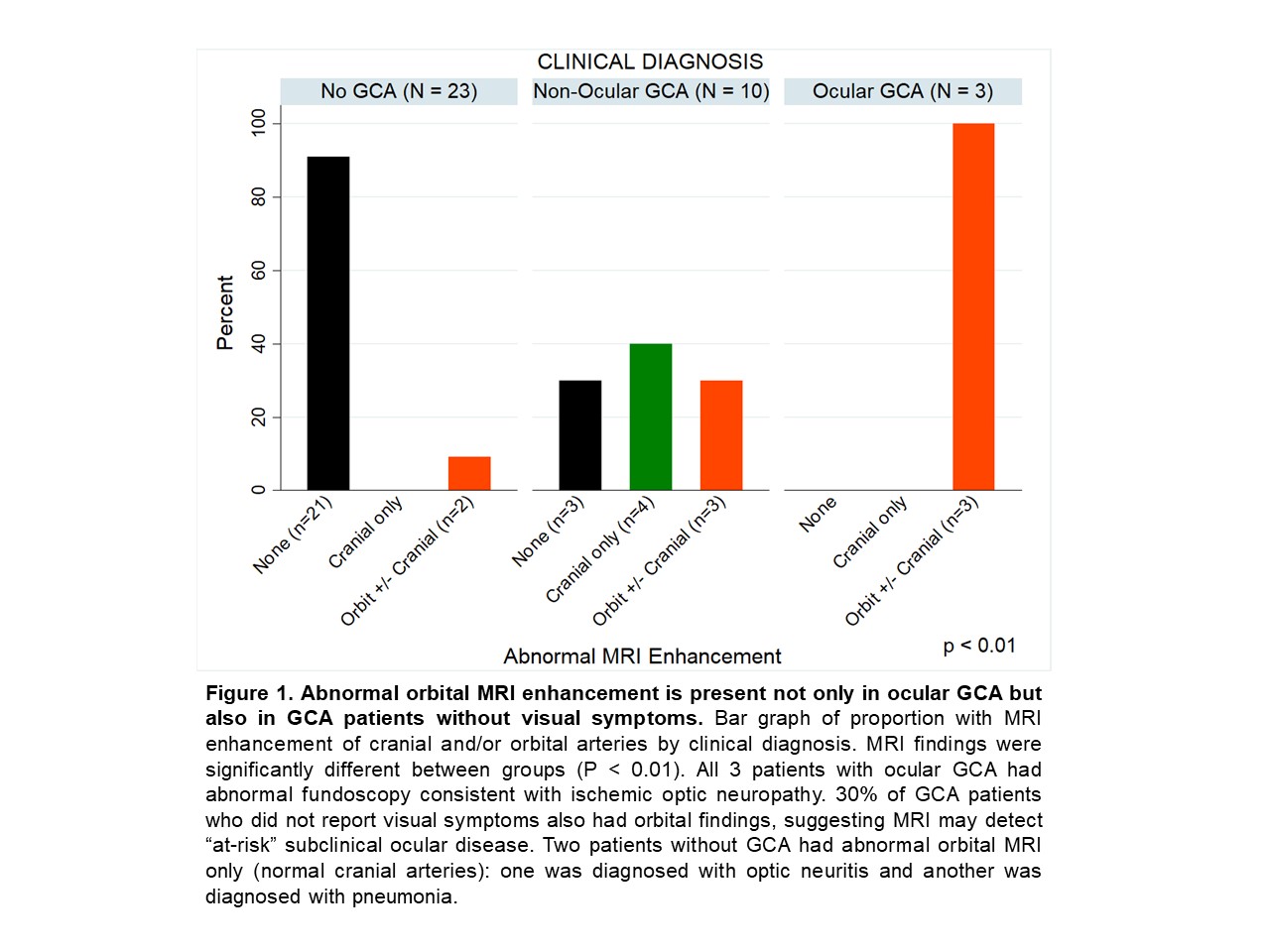
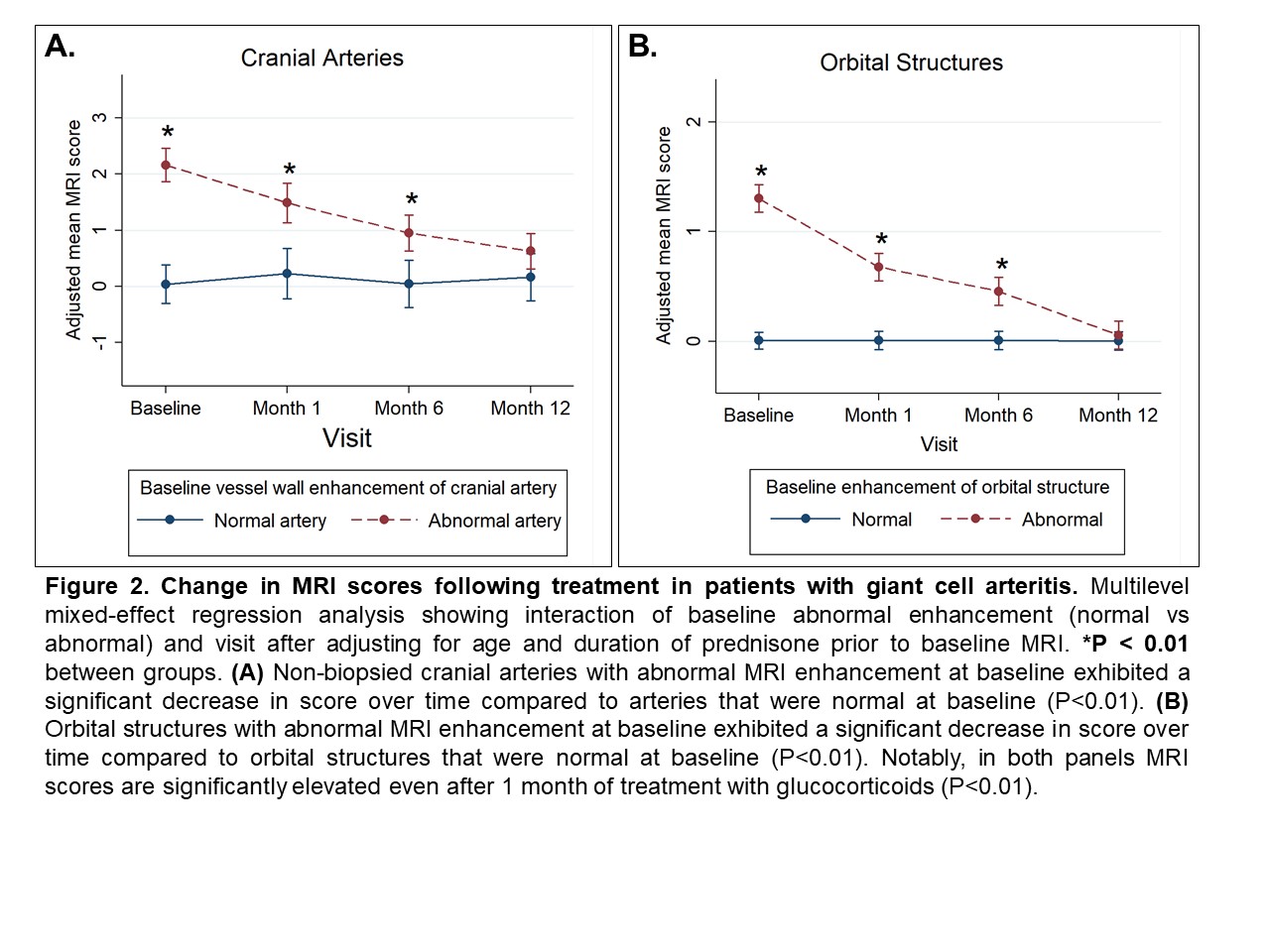
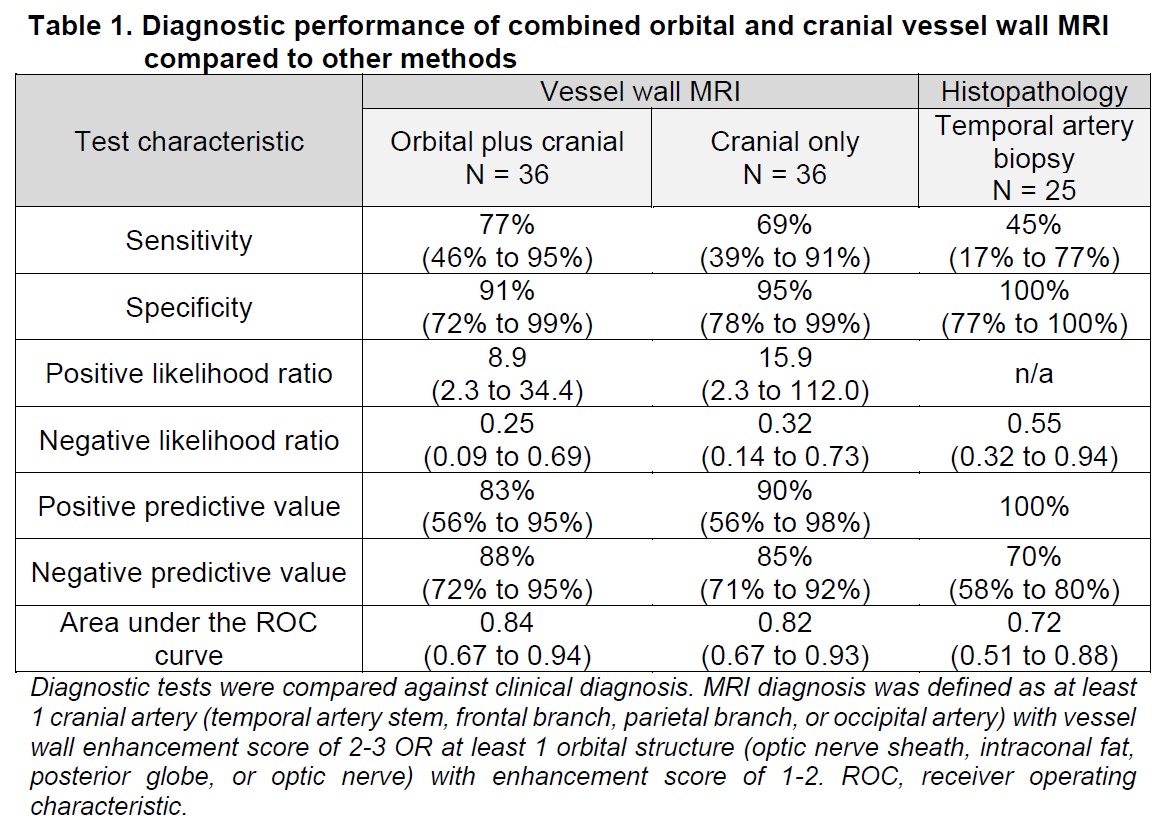
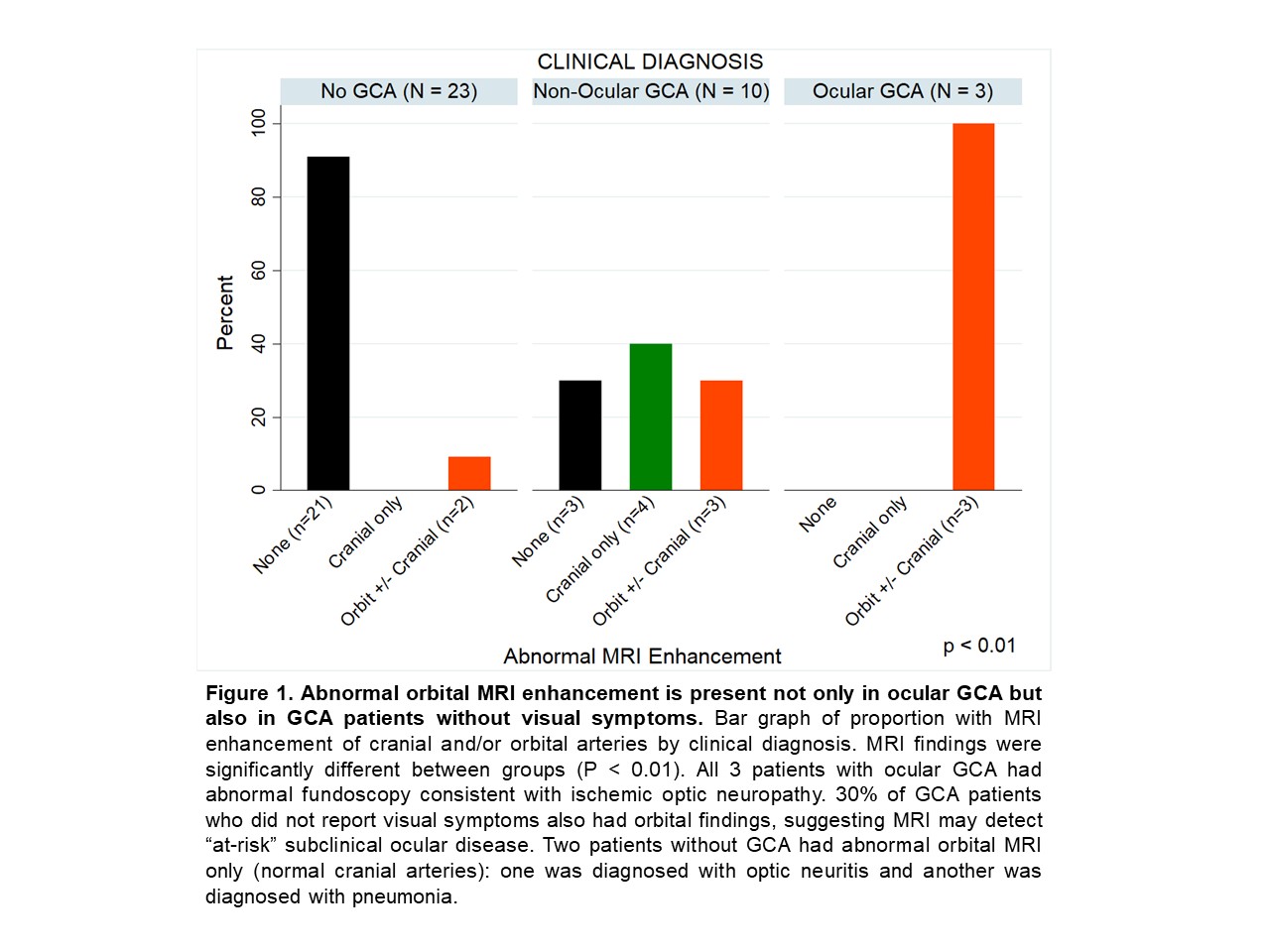
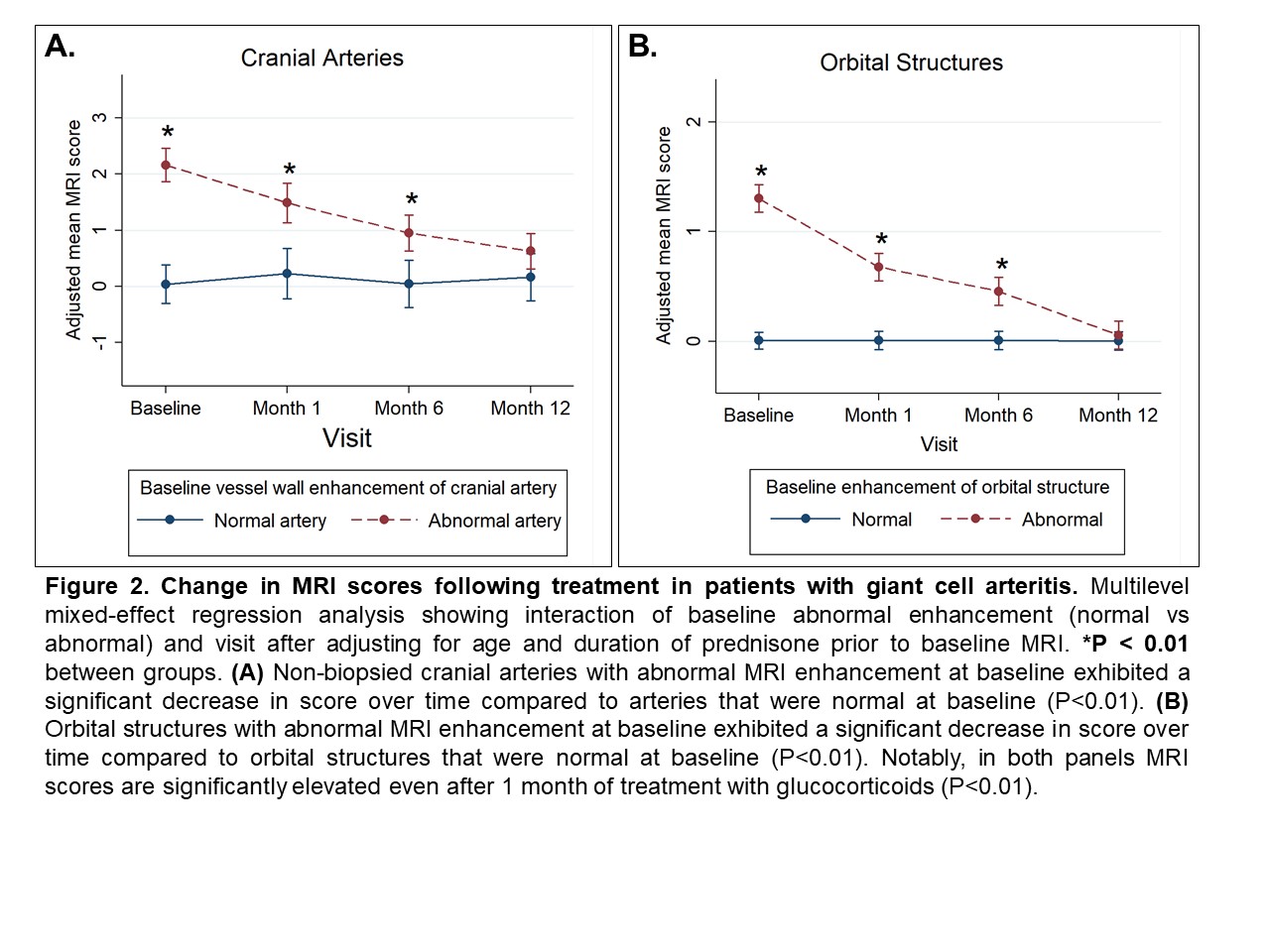
Results: The study included 36 patients with suspected cranial GCA: 31 new and 5 relapsing GCA. GCA was diagnosed in 13 patients: 10 non-ocular and 3 ocular GCA. The addition of orbital imaging to cranial vessel wall MRI had strong diagnostic performance with improved sensitivity compared to cranial MRI alone and temporal artery biopsy (Table 1). Orbital enhancement on MRI was observed in 100% of patients with ocular GCA and in 30% of GCA patients without visual symptoms (Figure 1). During follow-up, non-biopsied cranial arteries with abnormal MRI enhancement at baseline had a decrease in MRI score over time (P < 0.01, Figure 2A). Similarly, orbital MRI scores significantly decreased over time (P < 0.01, Figure 2B). Arteries with abnormal enhancement at baseline continued to have persistently elevated MRI scores even after 1 month of treatment (P< 0.01).
Conclusion: Combined orbital with cranial vessel wall MRI has very good diagnostic accuracy for GCA and may have the added value of identifying ocular GCA. This study is the first to demonstrate orbital MRI abnormalities in GCA patients without visual symptoms, suggesting that orbital MRI detects "at-risk" subclinical ocular disease. Imaging abnormalities persist even after 1 month of treatment, indicating flexibility in timing of MRI and potential translation to real-world settings. Decrease in MRI enhancement after treatment supports the possibility of using MRI for longitudinal disease surveillance. Future studies may determine if MRI identifies low-risk groups (e.g., those with normal orbital MRI) who can initiate a lower dose of glucocorticoids.
Disclosures: R. Rhee, None; S. Banerjee, None; V. Bhatt, None; M. Tamhankar, None; Q. Cao, None; N. Amudala, None; S. Chou, None; M. Burke, None; L. Loevner, Guerbet; P. Merkel, AbbVie, AstraZeneca, Boeringher-Ingelheim, Bristol-Myers Squibb, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Neutrolis, Takeda, CSL Behring, Dynacure, EMDSerono, Immagene, Jannsen, Kiniksa, Magenta, Novartis, Pfizer, Q32, Regeneron, Sparrow, Eicos, Electra, Kyverna, UpToDate; J. Song, None.
Background/Purpose: In giant cell arteritis (GCA), there is a critical need to identify patients at risk for vision loss ("ocular GCA"). MRI evaluates neurovascular anatomy posterior to the ocular globe, an area not visualized by ophthalmologic exam. This study aimed to determine the diagnostic utility of combined orbital and cranial vessel wall MRI in GCA (with or without visual symptoms) and evaluate longitudinal changes in imaging with treatment.
Methods: Patients with suspected new or relapsing cranial GCA who underwent orbital and brain vessel wall MRI were included. Nine patients had repeat imaging at months 1, 6, and 12 to assess changes over time. A clinical diagnosis of ocular or non-ocular GCA was determined by a rheumatologist and/or ophthalmologist and confirmed retrospectively. All MR images were scored by a single radiologist blinded to clinical data. Semi-quantitative integer scores of MRI enhancement were determined: 8 orbital structures were each scored 0, 1, or 2 (score 1-2 defined as abnormal) and included bilateral optic nerve sheath, optic nerve, intraconal orbital fat, and retrobulbar fat of posterior globe; 8 cranial arteries were each scored 0, 1, 2, or 3 (score 2-3 defined as abnormal) and included bilateral temporal arteries (stem, frontal, and parietal branches) and occipital arteries. MRI was considered diagnostic for GCA if at least 1 orbital or cranial artery had abnormal enhancement. Test characteristics were determined. Mixed-effects models were used to compare changes in scores over time between arteries that were abnormal vs normal at baseline.
Results: The study included 36 patients with suspected cranial GCA: 31 new and 5 relapsing GCA. GCA was diagnosed in 13 patients: 10 non-ocular and 3 ocular GCA. The addition of orbital imaging to cranial vessel wall MRI had strong diagnostic performance with improved sensitivity compared to cranial MRI alone and temporal artery biopsy (Table 1). Orbital enhancement on MRI was observed in 100% of patients with ocular GCA and in 30% of GCA patients without visual symptoms (Figure 1). During follow-up, non-biopsied cranial arteries with abnormal MRI enhancement at baseline had a decrease in MRI score over time (P < 0.01, Figure 2A). Similarly, orbital MRI scores significantly decreased over time (P < 0.01, Figure 2B). Arteries with abnormal enhancement at baseline continued to have persistently elevated MRI scores even after 1 month of treatment (P< 0.01).
Conclusion: Combined orbital with cranial vessel wall MRI has very good diagnostic accuracy for GCA and may have the added value of identifying ocular GCA. This study is the first to demonstrate orbital MRI abnormalities in GCA patients without visual symptoms, suggesting that orbital MRI detects "at-risk" subclinical ocular disease. Imaging abnormalities persist even after 1 month of treatment, indicating flexibility in timing of MRI and potential translation to real-world settings. Decrease in MRI enhancement after treatment supports the possibility of using MRI for longitudinal disease surveillance. Future studies may determine if MRI identifies low-risk groups (e.g., those with normal orbital MRI) who can initiate a lower dose of glucocorticoids.
Disclosures: R. Rhee, None; S. Banerjee, None; V. Bhatt, None; M. Tamhankar, None; Q. Cao, None; N. Amudala, None; S. Chou, None; M. Burke, None; L. Loevner, Guerbet; P. Merkel, AbbVie, AstraZeneca, Boeringher-Ingelheim, Bristol-Myers Squibb, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Neutrolis, Takeda, CSL Behring, Dynacure, EMDSerono, Immagene, Jannsen, Kiniksa, Magenta, Novartis, Pfizer, Q32, Regeneron, Sparrow, Eicos, Electra, Kyverna, UpToDate; J. Song, None.

