Back
Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes II: Cardiovascular and Other Comorbidities (1646–1650)
1647: Increased Risk of Lung Cancer in Rheumatoid Arthritis and Rheumatoid Arthritis-Associated Interstitial Lung Disease: A Matched Cohort Study with Cancer Registry Linkage
Monday, November 14, 2022
9:15 AM – 9:25 AM Eastern Time
Location: Terrace Ballroom IV

Rebecca Brooks, BS
University of Nebraska Medical Center
Omaha, NE, United States
Presenting Author(s)
Rebecca Brooks1, Yangyuna Yang1, Punyasha Roul2, Brent Luedders1, Namrata Singh3, Brian Sauer4, Grant Cannon5, Joshua Baker6, Ted Mikuls7 and Bryant England1, 1University of Nebraska Medical Center, Omaha, NE, 2UNMC, Omaha, NE, 3University of Washington, Bellevue, WA, 4Salt Lake City VA/University of Utah, Salt Lake City, UT, 5Retired, Salt Lake City, UT, 6University of Pennsylvania, Philadelphia, PA, 7Division of Rheumatology, University of Nebraska Medical Center, Omaha, NE
Background/Purpose: While patients with RA are predisposed to developing lung cancer, prior epidemiologic studies have been limited in their ability to account for potential confounders including cigarette smoking, and mendelian randomization studies have not found a causal link between RA-related genes and lung cancer risk. Interestingly, recent studies of patients with RA-interstitial lung disease (RA-ILD) have observed lung cancer to be a common cause of death. Therefore, we evaluated lung cancer risk in RA adjusting for relevant confounders and evaluated whether RA-ILD may be responsible for excess lung cancer risk in RA.
Methods: We performed a retrospective matched cohort study of patients with RA and RA-ILD within the Veterans Health Administration (VA) Corporate Data Warehouse between 2000-2019. RA patients were identified by a validated administrative-based algorithm requiring multiple diagnostic codes, rheumatologist diagnosis, and DMARD receipt or positive autoantibody ( >90% PPV). Nested within this RA cohort, RA-ILD patients were identified by an administrative-based algorithm requiring multiple ILD diagnostic codes and a pulmonologist diagnosis or ILD diagnostic testing ( >75% PPV). RA patients were matched with up to 10 randomly selected individuals without RA on age, gender, and VA enrollment year. Lung cancers were collected by linking to a VA cancer registry and the National Death Index, and individuals with a history of lung cancer were excluded. Conditional Cox regression models assessed the risk of incident lung cancer adjusting for race, ethnicity, cigarette smoking status, Agent Orange exposure, and comorbidity burden.
Results: We matched 73,338 RA to 642,148 non-RA patients, with a mean age of 63 years and 87% being male. Over 4,526,619 patient-years (mean follow-up 6.3 years), 18,301 incident lung cancers occurred. RA patients had a higher rate of incident lung cancer than non-RA (60.1 [58.0, 62.2] vs. 37.9 [37.3, 38.5] per 10,000 PY) (Table 1, Figure 1). After adjusting for potential confounders, RA was associated with an increased risk of lung cancer (aHR 1.53 [1.47,1.60). This association persisted in analyses limited to non-smokers (aHR 1.66 [1.24, 2.22]) and incident RA (aHR 1.49 [1.39, 1.59). In subgroup analyses by prevalent RA-ILD status, RA-ILD was more strongly associated with lung cancer risk (aHR 3.06 [2.05, 4.57]) than RA without ILD (aHR 1.53 [1.47, 1.59]) (Table 1). Analyses accounting for RA-ILD occurring during follow-up found a similar association between RA-ILD and lung cancer (aHR 2.75 [2.35, 3.22]) (Table 1, Figure 1).
Conclusion: RA was associated with a >50% increased risk of lung cancer after adjusting for potential confounders and in analyses restricted to non-smokers. Those with RA-ILD represented a particularly high-risk group with an approximate 3-fold increased risk of lung cancer, though lung cancer risk was also increased in RA patients without ILD. These findings suggest that increased lung cancer surveillance in RA, and especially RA-ILD, may be a useful strategy for reducing the burden posed by the leading cause of cancer death.
.jpg) Table 1. Associations of RA and RA-ILD with Lung Cancer
Table 1. Associations of RA and RA-ILD with Lung Cancer
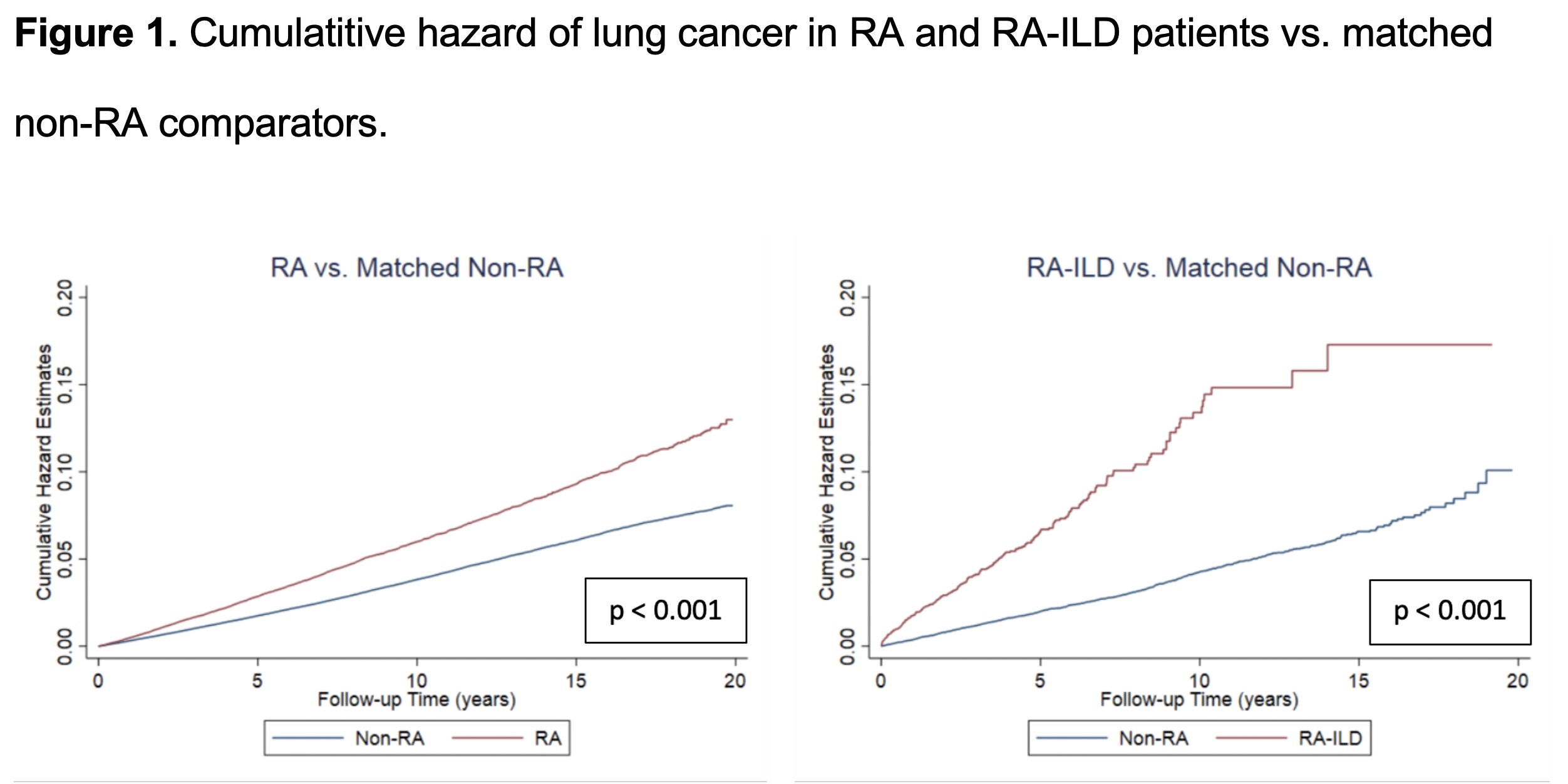 Figure 1. Cumulative hazard of lung cancer in RA and RA-ILD patients vs. matched non-RA comparators
Figure 1. Cumulative hazard of lung cancer in RA and RA-ILD patients vs. matched non-RA comparators
Disclosures: R. Brooks, None; Y. Yang, None; P. Roul, None; B. Luedders, None; N. Singh, None; B. Sauer, None; G. Cannon, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.
Background/Purpose: While patients with RA are predisposed to developing lung cancer, prior epidemiologic studies have been limited in their ability to account for potential confounders including cigarette smoking, and mendelian randomization studies have not found a causal link between RA-related genes and lung cancer risk. Interestingly, recent studies of patients with RA-interstitial lung disease (RA-ILD) have observed lung cancer to be a common cause of death. Therefore, we evaluated lung cancer risk in RA adjusting for relevant confounders and evaluated whether RA-ILD may be responsible for excess lung cancer risk in RA.
Methods: We performed a retrospective matched cohort study of patients with RA and RA-ILD within the Veterans Health Administration (VA) Corporate Data Warehouse between 2000-2019. RA patients were identified by a validated administrative-based algorithm requiring multiple diagnostic codes, rheumatologist diagnosis, and DMARD receipt or positive autoantibody ( >90% PPV). Nested within this RA cohort, RA-ILD patients were identified by an administrative-based algorithm requiring multiple ILD diagnostic codes and a pulmonologist diagnosis or ILD diagnostic testing ( >75% PPV). RA patients were matched with up to 10 randomly selected individuals without RA on age, gender, and VA enrollment year. Lung cancers were collected by linking to a VA cancer registry and the National Death Index, and individuals with a history of lung cancer were excluded. Conditional Cox regression models assessed the risk of incident lung cancer adjusting for race, ethnicity, cigarette smoking status, Agent Orange exposure, and comorbidity burden.
Results: We matched 73,338 RA to 642,148 non-RA patients, with a mean age of 63 years and 87% being male. Over 4,526,619 patient-years (mean follow-up 6.3 years), 18,301 incident lung cancers occurred. RA patients had a higher rate of incident lung cancer than non-RA (60.1 [58.0, 62.2] vs. 37.9 [37.3, 38.5] per 10,000 PY) (Table 1, Figure 1). After adjusting for potential confounders, RA was associated with an increased risk of lung cancer (aHR 1.53 [1.47,1.60). This association persisted in analyses limited to non-smokers (aHR 1.66 [1.24, 2.22]) and incident RA (aHR 1.49 [1.39, 1.59). In subgroup analyses by prevalent RA-ILD status, RA-ILD was more strongly associated with lung cancer risk (aHR 3.06 [2.05, 4.57]) than RA without ILD (aHR 1.53 [1.47, 1.59]) (Table 1). Analyses accounting for RA-ILD occurring during follow-up found a similar association between RA-ILD and lung cancer (aHR 2.75 [2.35, 3.22]) (Table 1, Figure 1).
Conclusion: RA was associated with a >50% increased risk of lung cancer after adjusting for potential confounders and in analyses restricted to non-smokers. Those with RA-ILD represented a particularly high-risk group with an approximate 3-fold increased risk of lung cancer, though lung cancer risk was also increased in RA patients without ILD. These findings suggest that increased lung cancer surveillance in RA, and especially RA-ILD, may be a useful strategy for reducing the burden posed by the leading cause of cancer death.
.jpg) Table 1. Associations of RA and RA-ILD with Lung Cancer
Table 1. Associations of RA and RA-ILD with Lung Cancer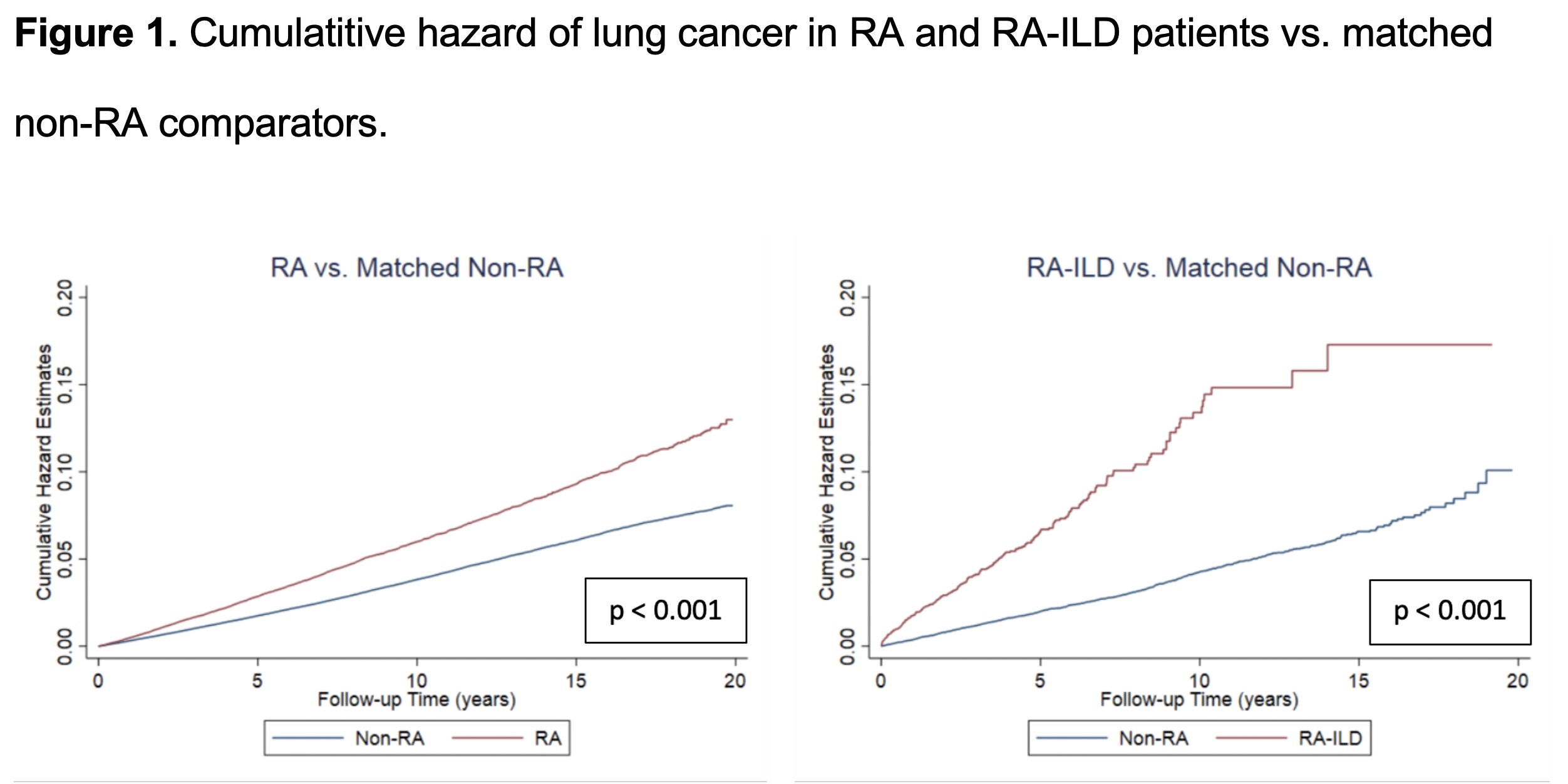 Figure 1. Cumulative hazard of lung cancer in RA and RA-ILD patients vs. matched non-RA comparators
Figure 1. Cumulative hazard of lung cancer in RA and RA-ILD patients vs. matched non-RA comparatorsDisclosures: R. Brooks, None; Y. Yang, None; P. Roul, None; B. Luedders, None; N. Singh, None; B. Sauer, None; G. Cannon, None; J. Baker, Bristol-Myers Squibb(BMS), RediTrex, Pfizer; T. Mikuls, Gilead Sciences, Bristol-Myers Squibb, Horizon, Sanofi, Pfizer Inc; B. England, Boehringer-Ingelheim.

