Back
Abstract Session
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: Abstracts: Systemic Sclerosis and Related Disorders – Clinical II: Clinical Phenotypes (1657–1662)
1659: FAM13A (Family with Sequence Similarity 13 Member A) Polymorphism Is Associated with Presence of a Radiographic Usual Interstitial Pneumonia Pattern in Patients with Systemic Sclerosis-Associated Interstitial Lung Disease
Monday, November 14, 2022
9:30 AM – 9:40 AM Eastern Time
Location: Room 103
Elana Bernstein, MD, MSc
Columbia University
New York, NY, United States
Presenting Author(s)
Elana Bernstein1, Francesco Boin2, Brett Elicker3, Yawen Ren4, John Varga5 and Shervin Assassi6, 1Columbia University, New York, NY, 2Cedars-Sinai Medical Center, Los Angeles, CA, 3University of California San Francisco, San Francisco, CA, 4University of Texas Health Science Center at Houston, Houston, TX, 5University of Michigan, Ann Arbor, MI, 6McGovern Medical School, University of Texas, Houston, TX
Background/Purpose: The pathogenesis of SSc-associated interstitial lung disease (ILD) is incompletely understood. The MUC5B promoter gain-of-function single nucleotide polymorphism (SNP) rs35705950 has been associated with idiopathic pulmonary fibrosis (IPF), familial pulmonary fibrosis (FPF), and RA-ILD, but not with SSc-ILD. Overexpression of MUC5B has been found in honeycombed pulmonary tissue. Honeycombing is not a feature of nonspecific interstitial pneumonitis (NSIP), the most prevalent radiographic pattern in SSc-ILD; this may explain the lack of association between the MUC5B rs35705950 SNP and SSc-ILD. In contrast, honeycombing is the hallmark of usual interstitial pneumonia (UIP), a pattern characteristic of IPF, FPF, and RA-ILD. Therefore, we hypothesize that the MUC5B promoter polymorphism or other IPF susceptibility loci may be associated with an increased risk to develop the uncommon SSc-UIP endophenotype, rather than SSc-ILD in general.
Methods: We performed a cross-sectional study of SSc-ILD patients from 4 US scleroderma centers to investigate the frequency of MUC5B rs35705950 and 12 additional IPF susceptibility loci (Table 1) in SSc-ILD patients stratified by high resolution chest CT (HRCT) imaging findings into UIP and non-UIP groups. Genotyping of the 13 investigated SNPs was performed by TaqMan assays in a central laboratory. A comprehensive analysis of HRCT scans performed by a blinded expert thoracic radiologist classified each HRCT as definite UIP, probable UIP, indeterminate, or alternative diagnosis, according to American Thoracic Society criteria. Association analyses were performed using logistic regression. HRCT pattern was the primary outcome. All genetic inheritance modes (dominant, recessive, and additive) were considered.
Results: 489 SSc-ILD patients were included; 80% were female and 75% were white. Twenty-three (4.7%) patients had a definite UIP pattern on HRCT (Table 2). Patients who had 2 copies of the IPF risk gene FAM13A minor allele rs2609255 had significantly higher odds of a definite UIP pattern compared to a non-definite UIP pattern on HRCT (OR 3.40, 95% CI 1.19 to 9.70) and compared to an alternative diagnosis (OR 3.65, 95% CI 1.25 to 10.65), a category which included mainly NSIP and organizing pneumonia. This positive association remained significant, although weaker, when analyzing white participants only. In contrast, the MUC5B promoter polymorphism was not associated with a definite UIP pattern in SSc-ILD, either in the entire cohort or among whites (Table 3).
Conclusion: We demonstrated a novel association between FAM13A and SSc-UIP. The FAM13A protein is involved in small GTPase mediated signal transduction. In addition to IPF, polymorphisms in FAM13A have been implicated in other pulmonary diseases such as silicosis and COPD. Contrary to IPF and RA-ILD, the MUC5B promoter polymorphism was not associated with a definite UIP pattern in SSc-ILD.
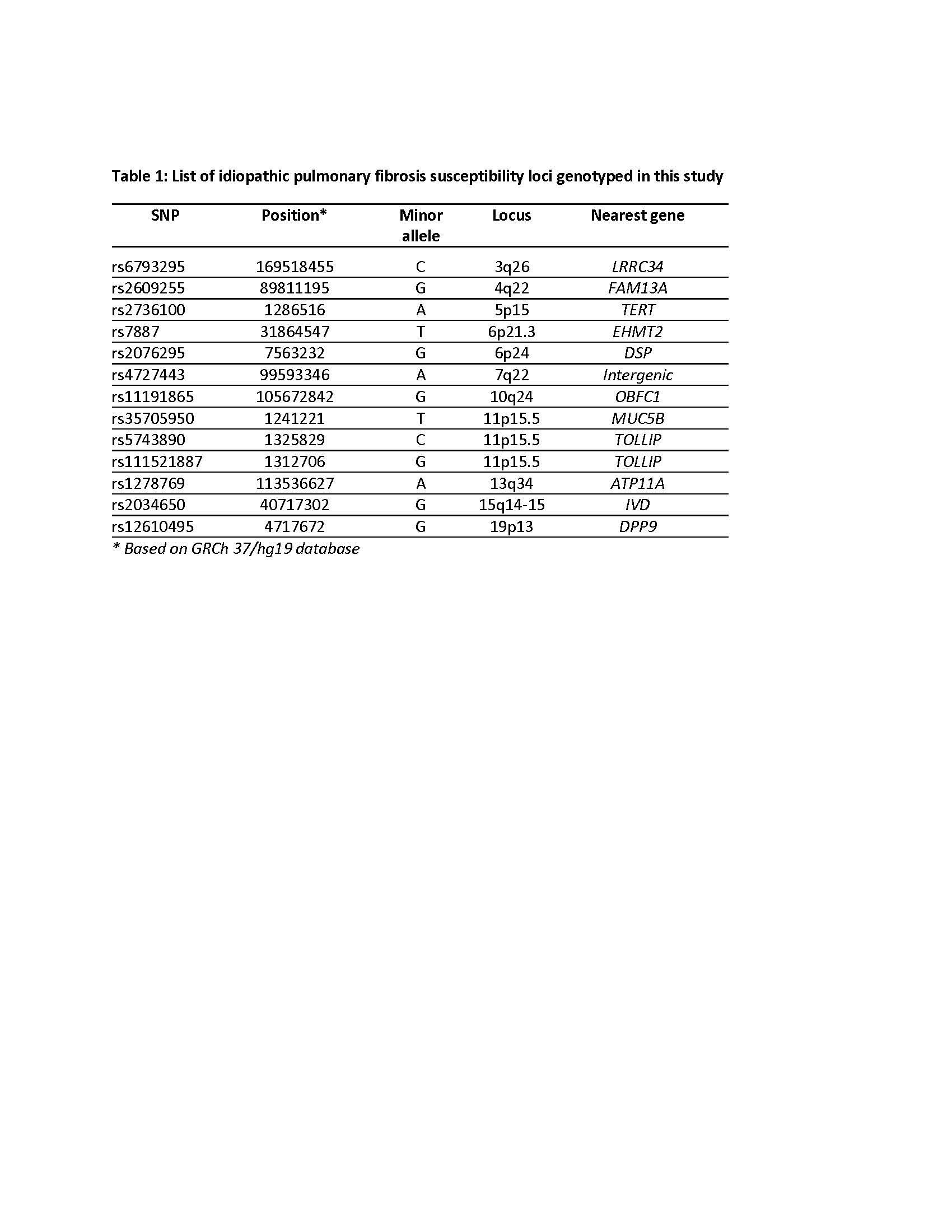 Table 1: List of idiopathic pulmonary fibrosis susceptibility loci genotyped in this study
Table 1: List of idiopathic pulmonary fibrosis susceptibility loci genotyped in this study
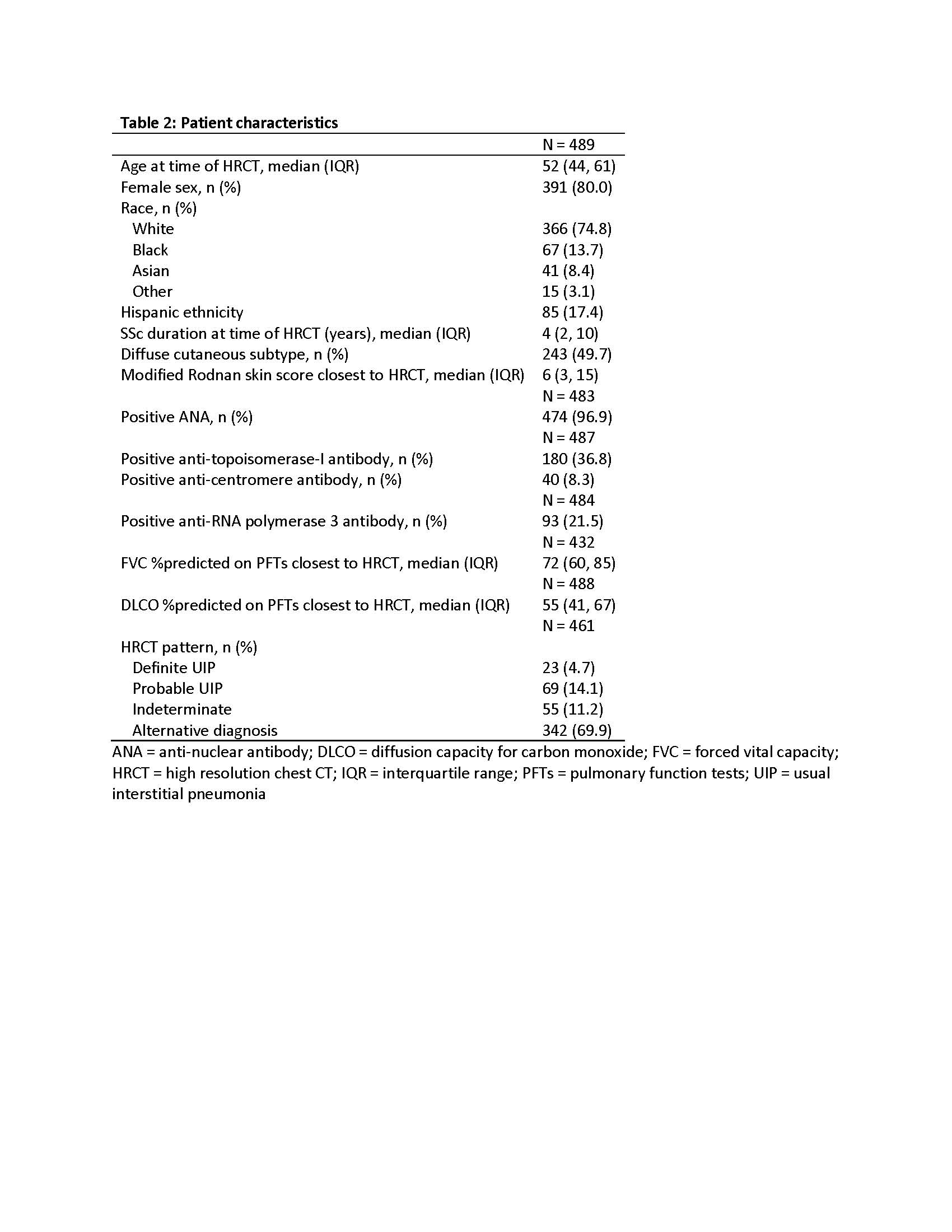 Table 2: Patient characteristics
Table 2: Patient characteristics
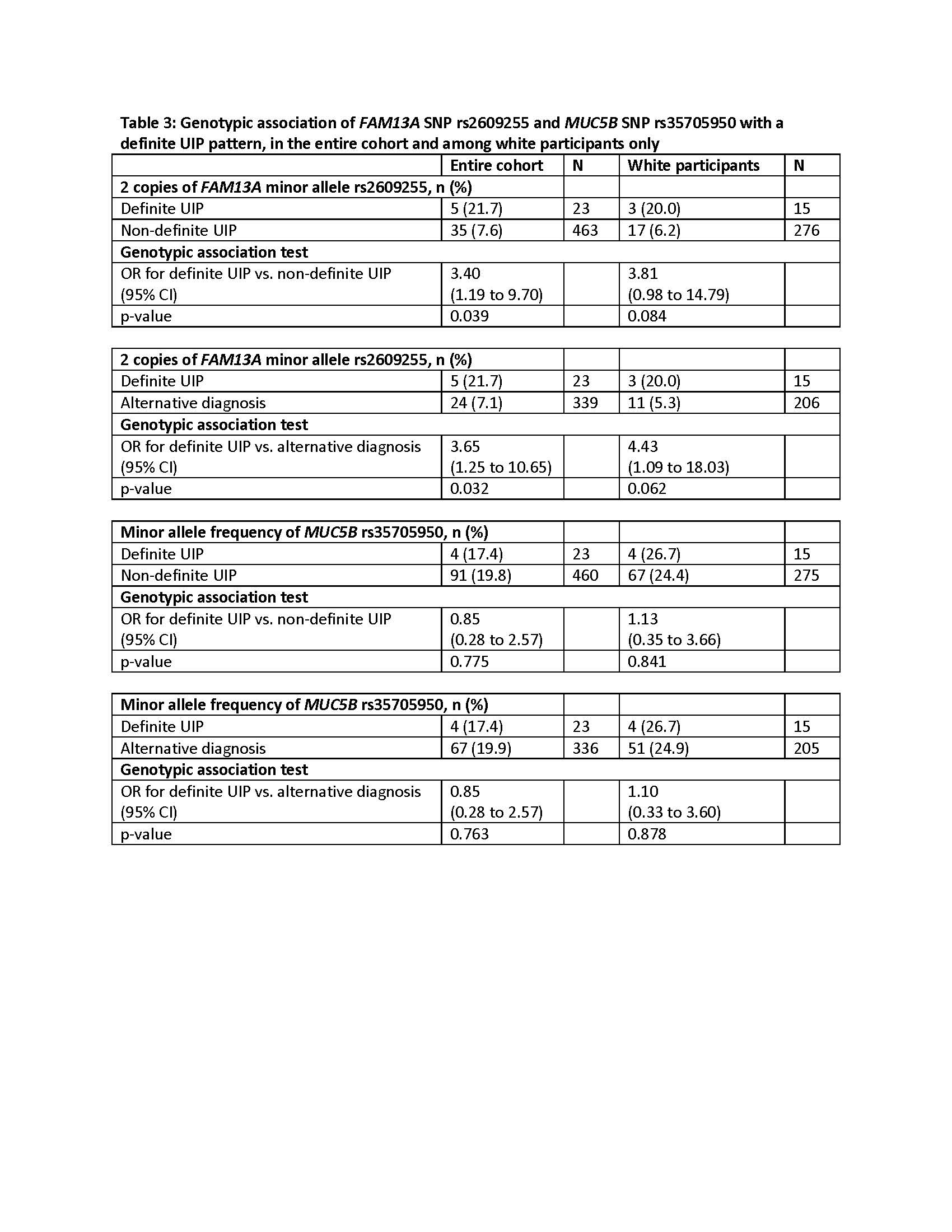 Table 3: Genotypic association of FAM13A SNP rs2609255 and MUC5B SNP rs35705950 with a definite UIP pattern, in the entire cohort and among white participants only
Table 3: Genotypic association of FAM13A SNP rs2609255 and MUC5B SNP rs35705950 with a definite UIP pattern, in the entire cohort and among white participants only
Disclosures: E. Bernstein, Boehringer-Ingelheim, Kadmon, Pfizer; F. Boin, None; B. Elicker, None; Y. Ren, None; J. Varga, Boehringer-Ingelheim; S. Assassi, Boehringer-Ingelheim, Janssen, Novartis, AstraZeneca, CSL Behring, AbbVie/Abbott.
Background/Purpose: The pathogenesis of SSc-associated interstitial lung disease (ILD) is incompletely understood. The MUC5B promoter gain-of-function single nucleotide polymorphism (SNP) rs35705950 has been associated with idiopathic pulmonary fibrosis (IPF), familial pulmonary fibrosis (FPF), and RA-ILD, but not with SSc-ILD. Overexpression of MUC5B has been found in honeycombed pulmonary tissue. Honeycombing is not a feature of nonspecific interstitial pneumonitis (NSIP), the most prevalent radiographic pattern in SSc-ILD; this may explain the lack of association between the MUC5B rs35705950 SNP and SSc-ILD. In contrast, honeycombing is the hallmark of usual interstitial pneumonia (UIP), a pattern characteristic of IPF, FPF, and RA-ILD. Therefore, we hypothesize that the MUC5B promoter polymorphism or other IPF susceptibility loci may be associated with an increased risk to develop the uncommon SSc-UIP endophenotype, rather than SSc-ILD in general.
Methods: We performed a cross-sectional study of SSc-ILD patients from 4 US scleroderma centers to investigate the frequency of MUC5B rs35705950 and 12 additional IPF susceptibility loci (Table 1) in SSc-ILD patients stratified by high resolution chest CT (HRCT) imaging findings into UIP and non-UIP groups. Genotyping of the 13 investigated SNPs was performed by TaqMan assays in a central laboratory. A comprehensive analysis of HRCT scans performed by a blinded expert thoracic radiologist classified each HRCT as definite UIP, probable UIP, indeterminate, or alternative diagnosis, according to American Thoracic Society criteria. Association analyses were performed using logistic regression. HRCT pattern was the primary outcome. All genetic inheritance modes (dominant, recessive, and additive) were considered.
Results: 489 SSc-ILD patients were included; 80% were female and 75% were white. Twenty-three (4.7%) patients had a definite UIP pattern on HRCT (Table 2). Patients who had 2 copies of the IPF risk gene FAM13A minor allele rs2609255 had significantly higher odds of a definite UIP pattern compared to a non-definite UIP pattern on HRCT (OR 3.40, 95% CI 1.19 to 9.70) and compared to an alternative diagnosis (OR 3.65, 95% CI 1.25 to 10.65), a category which included mainly NSIP and organizing pneumonia. This positive association remained significant, although weaker, when analyzing white participants only. In contrast, the MUC5B promoter polymorphism was not associated with a definite UIP pattern in SSc-ILD, either in the entire cohort or among whites (Table 3).
Conclusion: We demonstrated a novel association between FAM13A and SSc-UIP. The FAM13A protein is involved in small GTPase mediated signal transduction. In addition to IPF, polymorphisms in FAM13A have been implicated in other pulmonary diseases such as silicosis and COPD. Contrary to IPF and RA-ILD, the MUC5B promoter polymorphism was not associated with a definite UIP pattern in SSc-ILD.
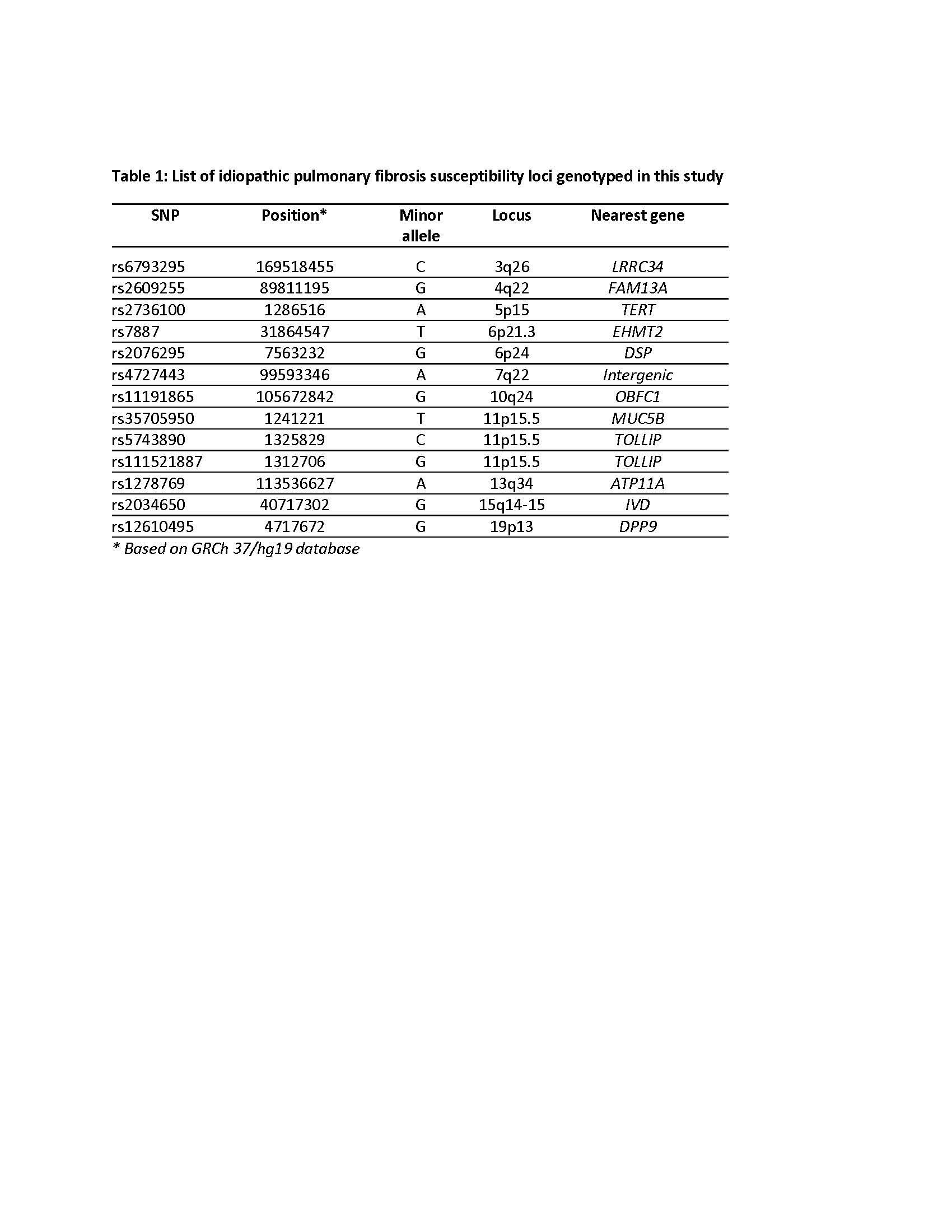 Table 1: List of idiopathic pulmonary fibrosis susceptibility loci genotyped in this study
Table 1: List of idiopathic pulmonary fibrosis susceptibility loci genotyped in this study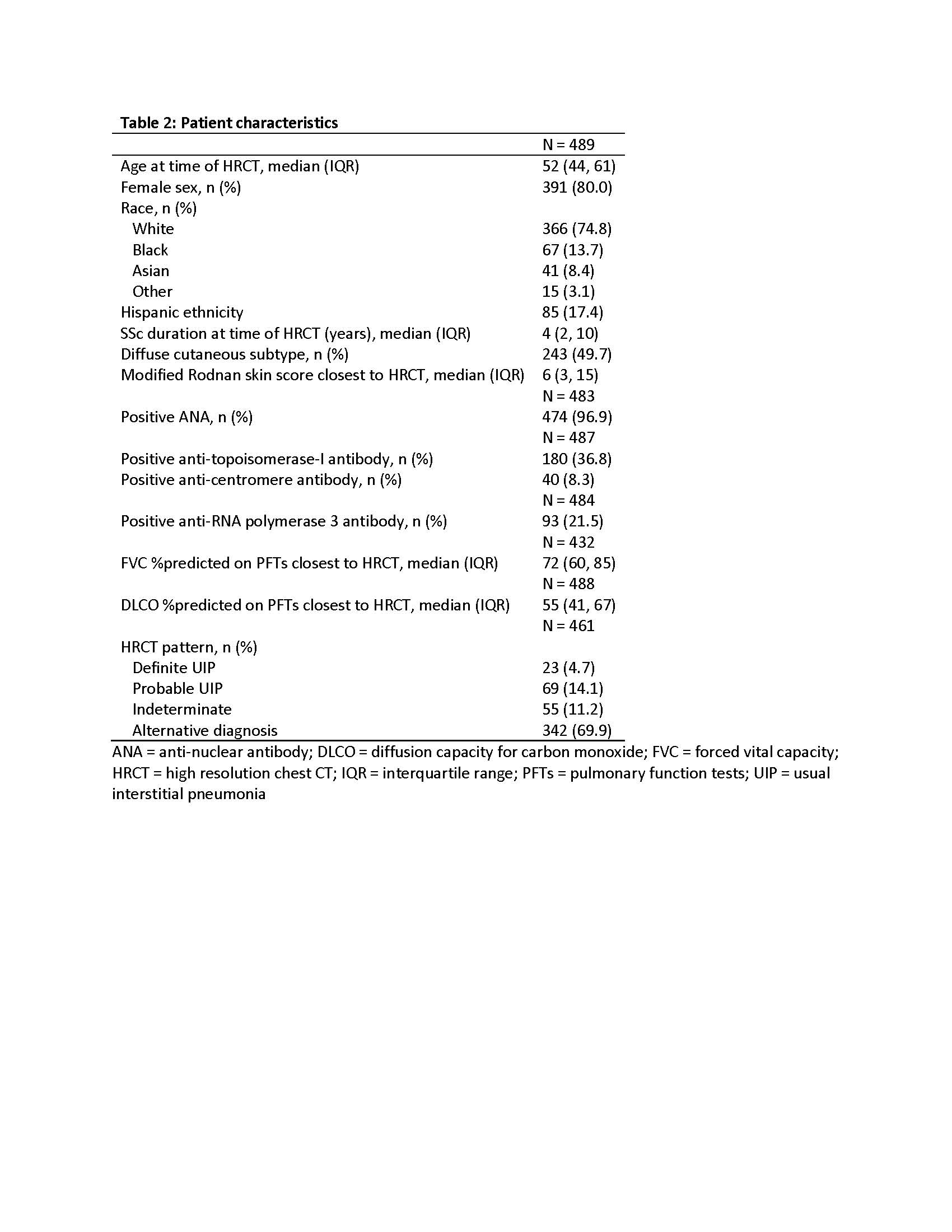 Table 2: Patient characteristics
Table 2: Patient characteristics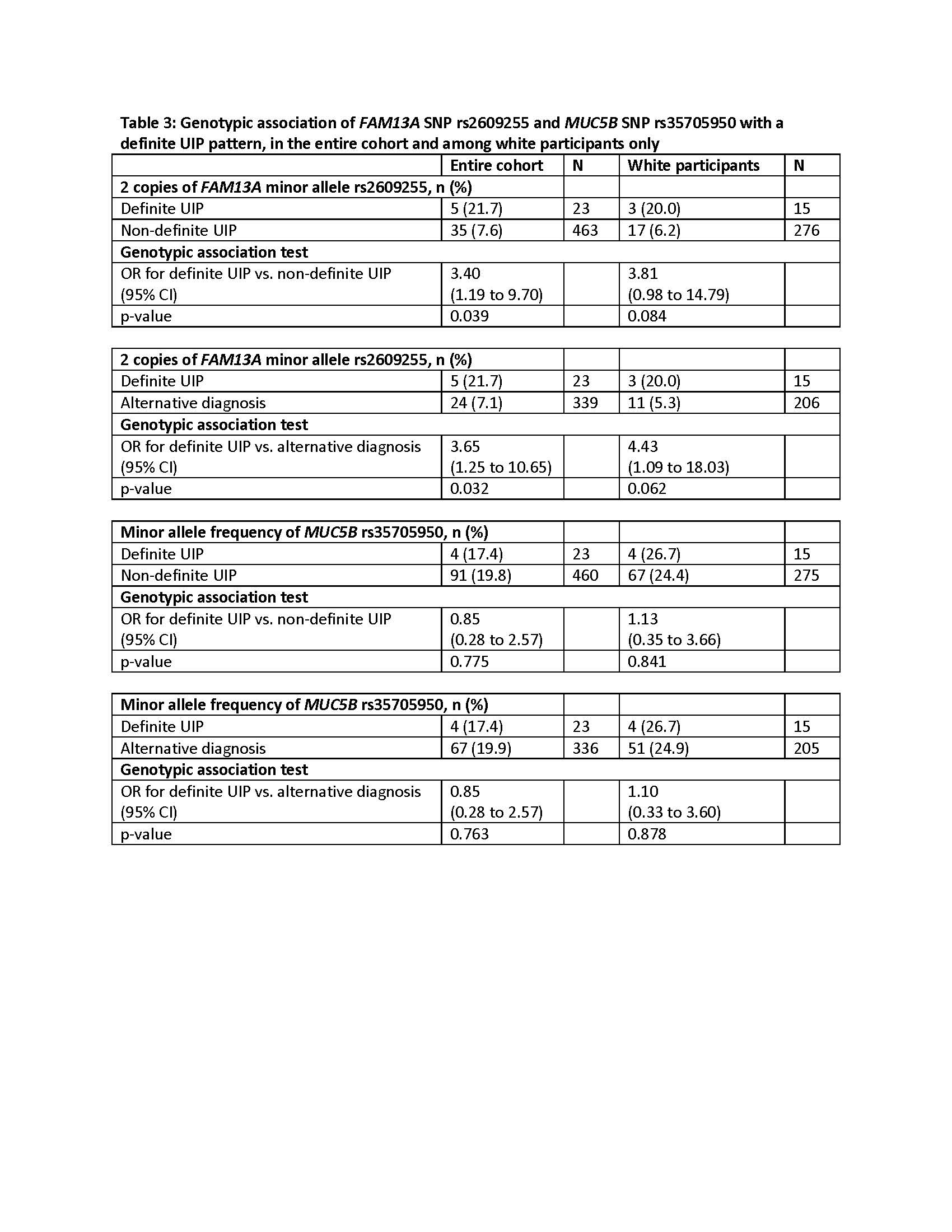 Table 3: Genotypic association of FAM13A SNP rs2609255 and MUC5B SNP rs35705950 with a definite UIP pattern, in the entire cohort and among white participants only
Table 3: Genotypic association of FAM13A SNP rs2609255 and MUC5B SNP rs35705950 with a definite UIP pattern, in the entire cohort and among white participants onlyDisclosures: E. Bernstein, Boehringer-Ingelheim, Kadmon, Pfizer; F. Boin, None; B. Elicker, None; Y. Ren, None; J. Varga, Boehringer-Ingelheim; S. Assassi, Boehringer-Ingelheim, Janssen, Novartis, AstraZeneca, CSL Behring, AbbVie/Abbott.

