Back
Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Diagnosis, Manifestations, and Outcomes II: Cardiovascular and Other Comorbidities (1646–1650)
1649: Five-Year Cardiovascular Event Risk in Early Rheumatoid Arthritis Patients Who Received Treat-to-Target Management
Monday, November 14, 2022
9:30 AM – 9:40 AM Eastern Time
Location: Terrace Ballroom IV
- TL
Tsz On Lam, MBBS, MRCP
Prince of Wales Hospital
Hong Kong, Hong Kong, China
Presenting Author(s)
Lai-shan Tam1, Tsz On Lam2 and Man Choi Wan3, 1The Chinese University of Hong Kong, Hong Kong, China, 2Prince of Wales Hospital, Hong Kong, Hong Kong, 3Ruttonjee Hospital, Hong Kong, Hong Kong, Hong Kong
Background/Purpose: Rheumatoid arthritis (RA) is known to cause increased risk of cardiovascular (CV) disease (CVD) due to the underlying inflammation. The year of 2010 revolutionised the clinical landscape of RA with the updated classification criteria allowing earlier classification of RA and with the recommendation of the treat-to-target (T2T) treatment approach. It is uncertain if the excess CVD risk could be ameliorated by effective suppression of inflammation using the T2T approach in patients with early RA (ERA). This study compared the incidence of CVD among ERA patients managed by a T2T strategy with a CV risk factor-matched non-RA population and a historical RA cohort (HRA).
Methods: This was an observational study using the territory-wide electronic health record system of Clinical Data Analysis and Reporting System (CDARS) and the Clinical Rheumatology Systemic Treat-to-target in Asia Leadership (CRYSTAL) registry. Two hundred and sixty-one ERA patients diagnosed between 2012-2016 with baseline disease duration less than 2 years were recruited. A HRA cohort with 268 RA patients diagnosed between 2002-2006 was also recruited. All of the ERA patients received T2T management aiming at remission while HRA patients received routine care. Each ERA/ HRA patient was matched to 3 non-RA controls according to age, gender, smoking status and CV risk factors including the presence of diabetes mellitus, hypertension and hyperlipidaemia. All subjects on antiplatelet/ anticoagulant agents, with pre-existing CVD, chronic kidney disease or other autoimmune diseases at baseline were excluded. All subjects were followed until death, migration or up to 5 years from baseline. Data of RA-related clinical and laboratory parameters were comprehensively collected at baseline and then at least annually. The primary endpoint was the first occurrence of a CV event (CVE). Secondary outcomes were the comparison of CVE incidence between different cohorts, differences in the inflammatory burden and treatment used between the ERA and HRA cohorts, and the RA-specific factors (inflammation and treatment) for predicting CVE among all RA patients.
Results: A total of 261 ERA patients, 783 ERA-controls, 268 HRA patients and 804 HRA-controls were eligible for this study. The incidence of CVE among ERA cohort & ERA-controls were similar (4.6 and 6.6 per 1000 persons-year respectively), with an unadjusted hazard ratio of 0.53 (95% confidence interval [CI] 0.15-1.79). In contrast, the incidence of CVE in HRA cohort was significantly higher than that of the HRA-controls with an unadjusted hazard ratio of 1.9 (95% CI 1.16-3.13). The incidence of CVE in the ERA cohort was significantly lower than that of the HRA cohort with an unadjusted hazard ratio of 0.24 (95% CI 0.1-0.6); the difference became insignificant after adjusting for inflammation (mean disease activity or remission duration), the use of methotrexate and traditional CV risk factors.
Conclusion: ERA patients managed by a T2T strategy did not develop excess CVE compared to CV risk factor-matched controls over 5 years. This diminished CVE risk among ERA patients could be explained by the lower mean disease activity, longer remission duration and the use of methotrexate.
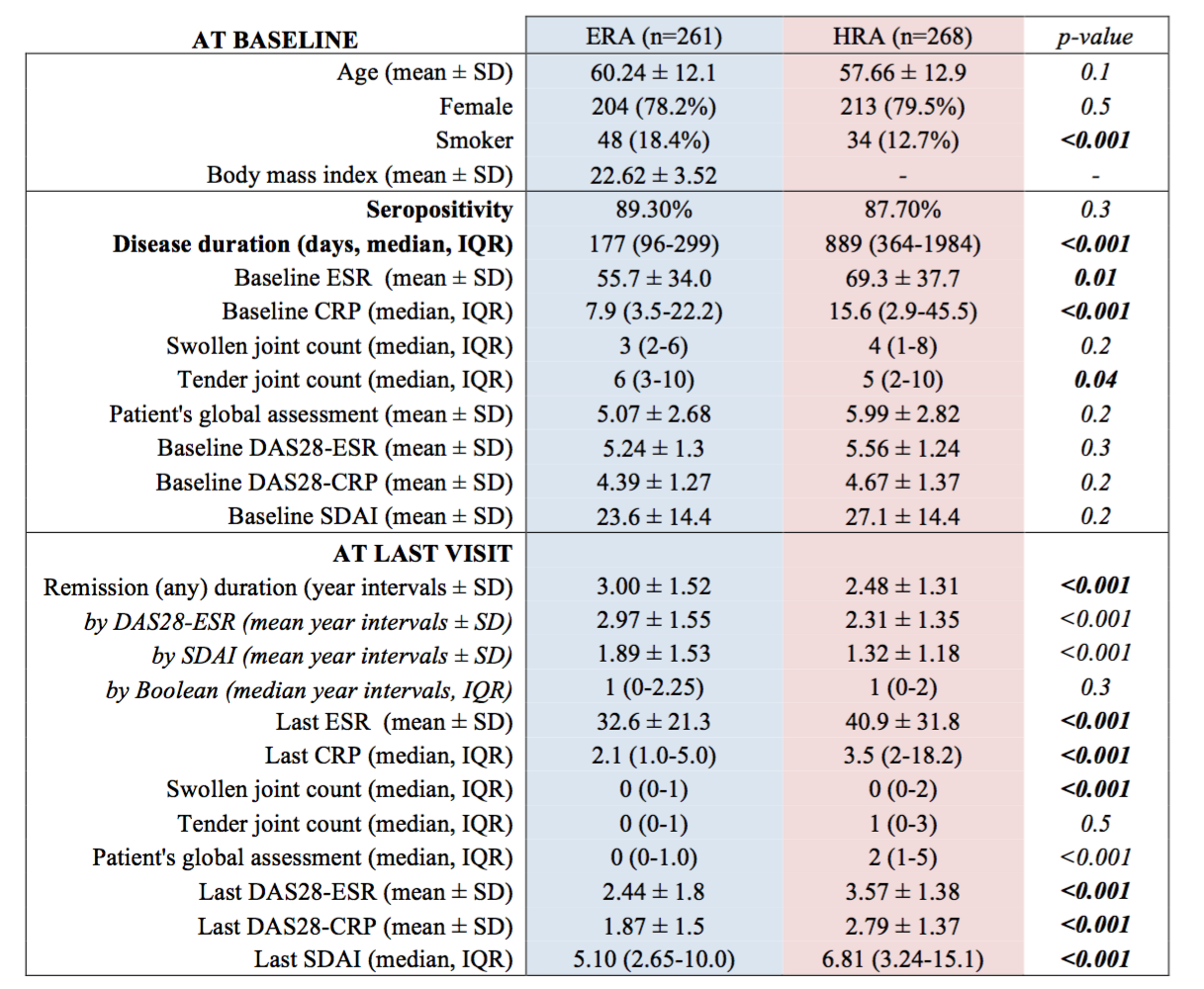 Table 1. Disease characteristics at baseline and at the end of follow-up. Although ERA patients had shorter baseline disease duration than HRA patients did, they both had comparably high disease activity at baseline. ERA patients, who received T2T management, enjoyed significantly lower disease activity at the last clinic visit.
Table 1. Disease characteristics at baseline and at the end of follow-up. Although ERA patients had shorter baseline disease duration than HRA patients did, they both had comparably high disease activity at baseline. ERA patients, who received T2T management, enjoyed significantly lower disease activity at the last clinic visit.
.jpg) Image 1. CVE-free survival Kaplan-Meier curves of ERA, HRA patients and their controls. HRA patients had significantly higher risk of CVE compared to their controls, while ERA and their controls had comparable risk of CVE.
Image 1. CVE-free survival Kaplan-Meier curves of ERA, HRA patients and their controls. HRA patients had significantly higher risk of CVE compared to their controls, while ERA and their controls had comparable risk of CVE.
.jpg) Table 2. Cox-regression using different models showed that the lower risk of CVE in ERA patients was probably driven by MTX use, lower disease activity and longer disease remission.
Table 2. Cox-regression using different models showed that the lower risk of CVE in ERA patients was probably driven by MTX use, lower disease activity and longer disease remission.
Disclosures: L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca; T. Lam, None; M. Wan, None.
Background/Purpose: Rheumatoid arthritis (RA) is known to cause increased risk of cardiovascular (CV) disease (CVD) due to the underlying inflammation. The year of 2010 revolutionised the clinical landscape of RA with the updated classification criteria allowing earlier classification of RA and with the recommendation of the treat-to-target (T2T) treatment approach. It is uncertain if the excess CVD risk could be ameliorated by effective suppression of inflammation using the T2T approach in patients with early RA (ERA). This study compared the incidence of CVD among ERA patients managed by a T2T strategy with a CV risk factor-matched non-RA population and a historical RA cohort (HRA).
Methods: This was an observational study using the territory-wide electronic health record system of Clinical Data Analysis and Reporting System (CDARS) and the Clinical Rheumatology Systemic Treat-to-target in Asia Leadership (CRYSTAL) registry. Two hundred and sixty-one ERA patients diagnosed between 2012-2016 with baseline disease duration less than 2 years were recruited. A HRA cohort with 268 RA patients diagnosed between 2002-2006 was also recruited. All of the ERA patients received T2T management aiming at remission while HRA patients received routine care. Each ERA/ HRA patient was matched to 3 non-RA controls according to age, gender, smoking status and CV risk factors including the presence of diabetes mellitus, hypertension and hyperlipidaemia. All subjects on antiplatelet/ anticoagulant agents, with pre-existing CVD, chronic kidney disease or other autoimmune diseases at baseline were excluded. All subjects were followed until death, migration or up to 5 years from baseline. Data of RA-related clinical and laboratory parameters were comprehensively collected at baseline and then at least annually. The primary endpoint was the first occurrence of a CV event (CVE). Secondary outcomes were the comparison of CVE incidence between different cohorts, differences in the inflammatory burden and treatment used between the ERA and HRA cohorts, and the RA-specific factors (inflammation and treatment) for predicting CVE among all RA patients.
Results: A total of 261 ERA patients, 783 ERA-controls, 268 HRA patients and 804 HRA-controls were eligible for this study. The incidence of CVE among ERA cohort & ERA-controls were similar (4.6 and 6.6 per 1000 persons-year respectively), with an unadjusted hazard ratio of 0.53 (95% confidence interval [CI] 0.15-1.79). In contrast, the incidence of CVE in HRA cohort was significantly higher than that of the HRA-controls with an unadjusted hazard ratio of 1.9 (95% CI 1.16-3.13). The incidence of CVE in the ERA cohort was significantly lower than that of the HRA cohort with an unadjusted hazard ratio of 0.24 (95% CI 0.1-0.6); the difference became insignificant after adjusting for inflammation (mean disease activity or remission duration), the use of methotrexate and traditional CV risk factors.
Conclusion: ERA patients managed by a T2T strategy did not develop excess CVE compared to CV risk factor-matched controls over 5 years. This diminished CVE risk among ERA patients could be explained by the lower mean disease activity, longer remission duration and the use of methotrexate.
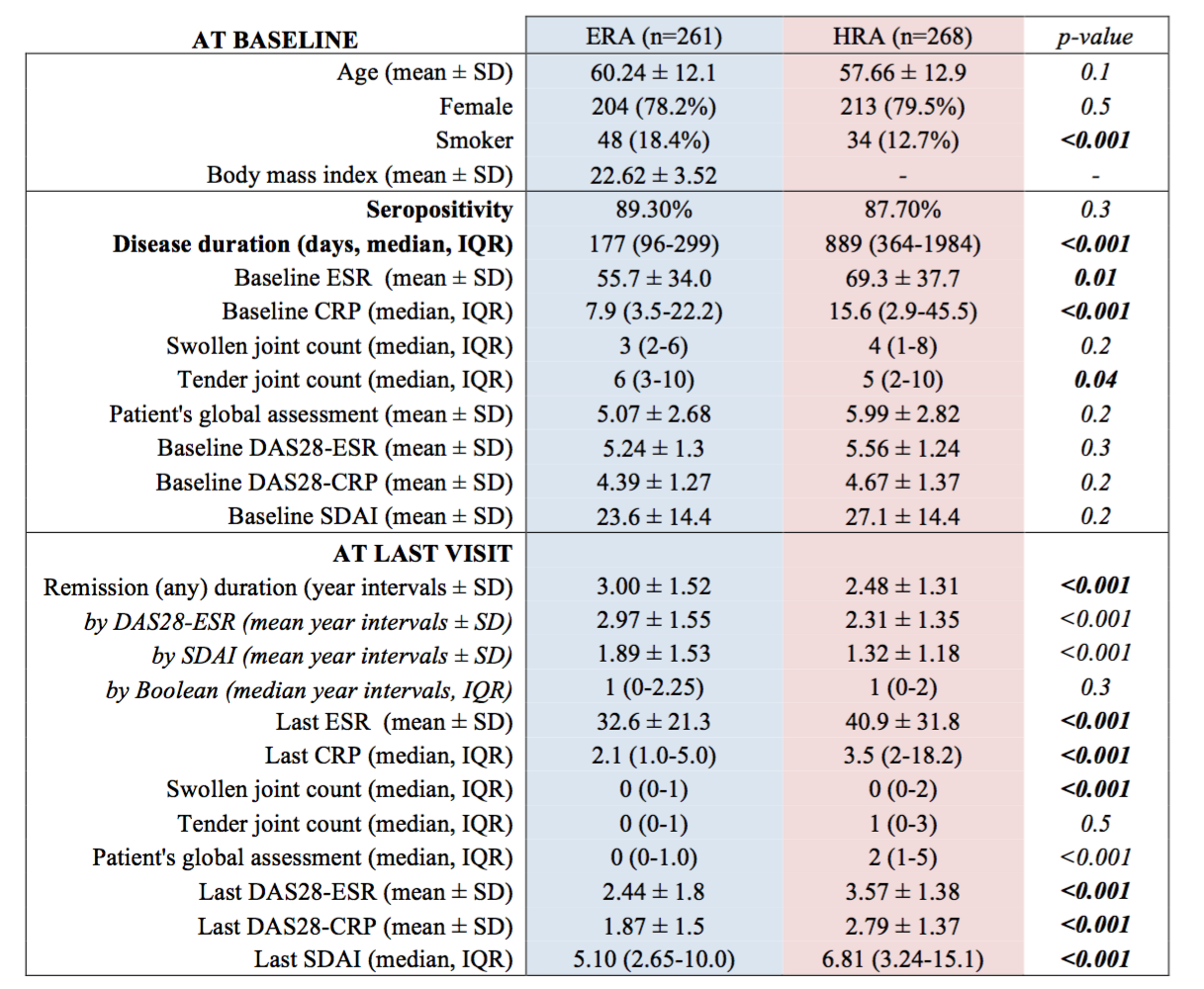 Table 1. Disease characteristics at baseline and at the end of follow-up. Although ERA patients had shorter baseline disease duration than HRA patients did, they both had comparably high disease activity at baseline. ERA patients, who received T2T management, enjoyed significantly lower disease activity at the last clinic visit.
Table 1. Disease characteristics at baseline and at the end of follow-up. Although ERA patients had shorter baseline disease duration than HRA patients did, they both had comparably high disease activity at baseline. ERA patients, who received T2T management, enjoyed significantly lower disease activity at the last clinic visit..jpg) Image 1. CVE-free survival Kaplan-Meier curves of ERA, HRA patients and their controls. HRA patients had significantly higher risk of CVE compared to their controls, while ERA and their controls had comparable risk of CVE.
Image 1. CVE-free survival Kaplan-Meier curves of ERA, HRA patients and their controls. HRA patients had significantly higher risk of CVE compared to their controls, while ERA and their controls had comparable risk of CVE..jpg) Table 2. Cox-regression using different models showed that the lower risk of CVE in ERA patients was probably driven by MTX use, lower disease activity and longer disease remission.
Table 2. Cox-regression using different models showed that the lower risk of CVE in ERA patients was probably driven by MTX use, lower disease activity and longer disease remission.Disclosures: L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca; T. Lam, None; M. Wan, None.

