Back
Poster Session D
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1856–1887) Muscle Biology, Myositis and Myopathies Poster II
1871: Hospitalization Outcomes for Acute Myocardial Infraction and Acute Heart Failure in Patients with Idiopathic Inflammatory Myopathies (IIM) from 2016-2019 National Inpatient Sample (NIS)
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ZL
Zi Ying Li, MD, MPH
Roger Williams Medical Center
Providence, RI, United States
Abstract Poster Presenter(s)
Zi Ying Li1, Siyi Huang2, Kevin Xi3, Deepan Dalal4 and Anthony Reginato5, 1Roger Williams Medical Center, Providence, RI, 2UCSF Fresno, Fresno, CA, 3Brown University, Providence, 4Brown University School of Medicine, Providence, RI, 5Brown University, Providence, RI
Background/Purpose: Cardiovascular disease was encountered in 15% of hospital admission from 2016-2017 for patients with idiopathic inflammatory myopathies (IIM) based on the National Inpatient Sample (NIS) study in 2021.1 The pathophysiology for cardiovascular damage in myositis is a multifactorial-process. Myositis can cause inflammation at the myocardium with accelerated coronary atherosclerosis.2 In addition, patients with IIM are at increased risk of heart failure, conduction abnormalities and venous thromboembolism .3,4,5 However, the presence of underlying inflammatory myositis and its direct impact on outcomes after acute myocardial infraction (AMI) and acute heart failure(AHF) has not been elucidated.
Methods: Using NIS database from 2016-19, which stratifies 20% of the total national hospital admissions, we identified patients with a primary admission diagnosis of AMI or AHF using ICD-10 codes. For each admission, we calculated the length of stay and ascertained the mortality. The independent variable for present or absence of myositis as a secondary diagnosis. Covariates of interest included baseline demographics and other comorbidities. The association of myositis with inpatient mortality and length of stay (LOS) was calculated using multivariable logistic regression.
Results: We identified 508,313 AMI hospitalization from 2016-2019, of which 512 patients had IMM. Patient in the myositis group were older in mean age (67 vs 69; p< 0.001), and had a higher proportion of females(37% vs 46%; p< 0.001). There was no difference in inpatient mortality between two groups of patients (4.6% vs 5.5%; p=0.3). In multivariable logistic regression model, after adjusting for age, race, gender, region, income and confounding comorbidities, there was continued to remain no significant difference in the odd of inpatient mortality between the two group (p=0.7). The LOS associated with myocardial infarction admission was longer in patient with IMM as compared to those without IMM . (Table. 1A/B)
We identified 220,647 AHF hospitalization from 2016-2019 with 303 patients had IMM. Myositis patients in this cohort were significantly younger (73 vs. 70; p< 0.001), and majority of them were female compared to the non-myositis group. (48% vs. 55%; p=0.007). There was no significant difference in hospitalization mortality for AHF between these two groups of patient (2.8% vs.3.6%; p=0.4). There was no significant difference in the odd of hospitalization mortality of AHF between these two groups. (p=0.5). The adjusted odds of LOS for acute heart failure in patients with IMM was significant longer compared to those without IMM (p< 0.001).(Table.2A/B)
Conclusion: Inpatient mortality in acute myocardial infraction and acute heart failure were similar in patient with and without IMM in this 4-year cohort study, whereas the LOS in both cohorts were longer in patients with myositis. The increase LOS may due to the extra time in work up or monitoring for myositis disease activity.
.jpg) Hospitalization Mortality of Acute Myocardial Infraction in Patient Without and With Myositis in 2016-2019
Hospitalization Mortality of Acute Myocardial Infraction in Patient Without and With Myositis in 2016-2019
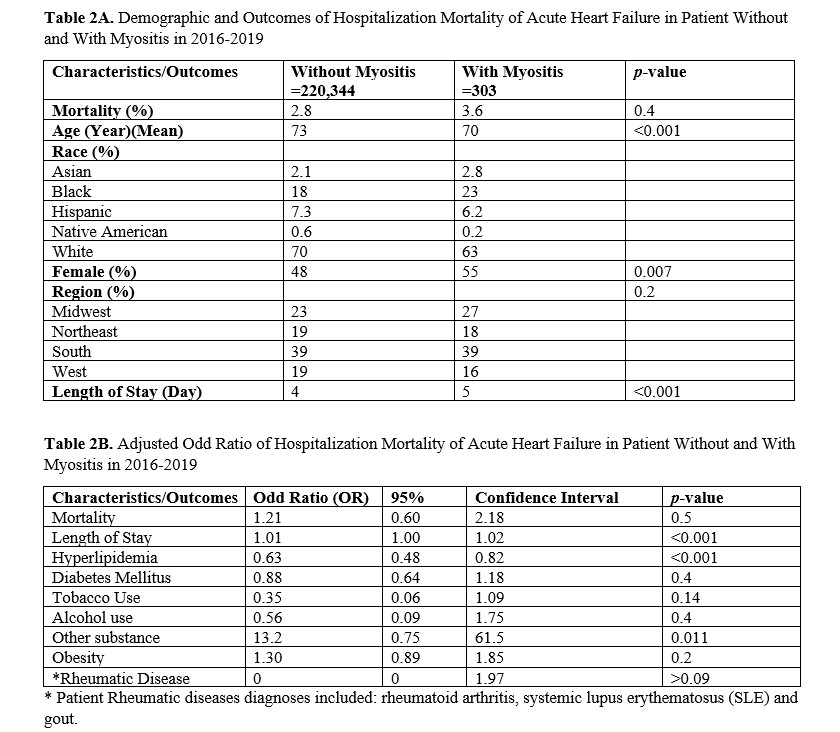 Hospitalization Mortality of Acute Heart Failure in Patient Without and With Myositis in 2016-2019
Hospitalization Mortality of Acute Heart Failure in Patient Without and With Myositis in 2016-2019
Disclosures: Z. Li, None; S. Huang, None; K. Xi, None; D. Dalal, None; A. Reginato, None.
Background/Purpose: Cardiovascular disease was encountered in 15% of hospital admission from 2016-2017 for patients with idiopathic inflammatory myopathies (IIM) based on the National Inpatient Sample (NIS) study in 2021.1 The pathophysiology for cardiovascular damage in myositis is a multifactorial-process. Myositis can cause inflammation at the myocardium with accelerated coronary atherosclerosis.2 In addition, patients with IIM are at increased risk of heart failure, conduction abnormalities and venous thromboembolism .3,4,5 However, the presence of underlying inflammatory myositis and its direct impact on outcomes after acute myocardial infraction (AMI) and acute heart failure(AHF) has not been elucidated.
Methods: Using NIS database from 2016-19, which stratifies 20% of the total national hospital admissions, we identified patients with a primary admission diagnosis of AMI or AHF using ICD-10 codes. For each admission, we calculated the length of stay and ascertained the mortality. The independent variable for present or absence of myositis as a secondary diagnosis. Covariates of interest included baseline demographics and other comorbidities. The association of myositis with inpatient mortality and length of stay (LOS) was calculated using multivariable logistic regression.
Results: We identified 508,313 AMI hospitalization from 2016-2019, of which 512 patients had IMM. Patient in the myositis group were older in mean age (67 vs 69; p< 0.001), and had a higher proportion of females(37% vs 46%; p< 0.001). There was no difference in inpatient mortality between two groups of patients (4.6% vs 5.5%; p=0.3). In multivariable logistic regression model, after adjusting for age, race, gender, region, income and confounding comorbidities, there was continued to remain no significant difference in the odd of inpatient mortality between the two group (p=0.7). The LOS associated with myocardial infarction admission was longer in patient with IMM as compared to those without IMM . (Table. 1A/B)
We identified 220,647 AHF hospitalization from 2016-2019 with 303 patients had IMM. Myositis patients in this cohort were significantly younger (73 vs. 70; p< 0.001), and majority of them were female compared to the non-myositis group. (48% vs. 55%; p=0.007). There was no significant difference in hospitalization mortality for AHF between these two groups of patient (2.8% vs.3.6%; p=0.4). There was no significant difference in the odd of hospitalization mortality of AHF between these two groups. (p=0.5). The adjusted odds of LOS for acute heart failure in patients with IMM was significant longer compared to those without IMM (p< 0.001).(Table.2A/B)
Conclusion: Inpatient mortality in acute myocardial infraction and acute heart failure were similar in patient with and without IMM in this 4-year cohort study, whereas the LOS in both cohorts were longer in patients with myositis. The increase LOS may due to the extra time in work up or monitoring for myositis disease activity.
.jpg) Hospitalization Mortality of Acute Myocardial Infraction in Patient Without and With Myositis in 2016-2019
Hospitalization Mortality of Acute Myocardial Infraction in Patient Without and With Myositis in 2016-2019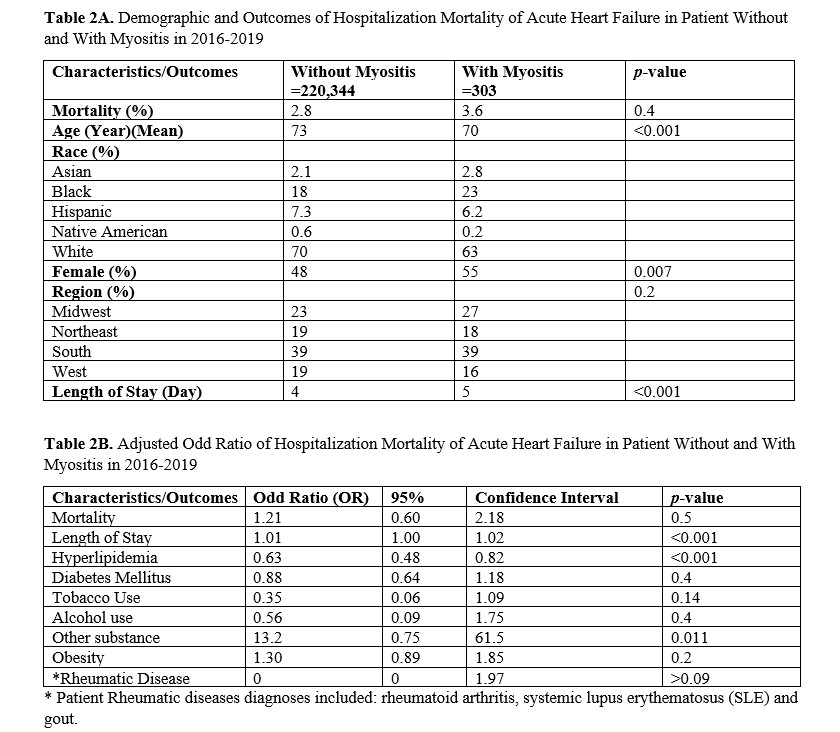 Hospitalization Mortality of Acute Heart Failure in Patient Without and With Myositis in 2016-2019
Hospitalization Mortality of Acute Heart Failure in Patient Without and With Myositis in 2016-2019Disclosures: Z. Li, None; S. Huang, None; K. Xi, None; D. Dalal, None; A. Reginato, None.

