Back
Poster Session D
Crystal arthropathies
Session: (1787–1829) Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
1826: Association of High Uric Acid Levels with Low Bone Mineral Density in Pre- but Not Post-menopausal Women with Rheumatoid Arthritis
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SH
Sandra Hermann, MD
Charité
Berlin, Germany
Abstract Poster Presenter(s)
Sandra Hermann1, Andriko Palmowski1, Bukrhard Muche2, Kay-Geert Hermann3, Edgar Wiebe1 and Frank Buttgereit4, 1Department of Rheumatology and Clinical Immunology, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany, 2Charité University Hospital, CCM, Berlin, Germany, 3Charité - Universitätsmedizin Berlin, Berlin, Germany, 4Charité Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin / DRFZ Berlin, Berlin, Germany
Background/Purpose: Uric acid is controversially discussed regarding its effect on bone health. Higher uric acid levels have been associated with higher T-scores and fewer bone fractures in postmenopausal women. Rheumatoid arthritis (RA), as a chronic inflammatory disease, is a risk factor for fractures in both men and women. The role of uric acid in patients with RA is not yet clarified. Further, there may be different effects of uric acid on organ tissues such as the lungs, depending on the hormone status of women. We aimed at investigating the effect of uric acid level on bone mineral density and the development of osteoporosis in patients with RA and whether there is a difference between premenopausal and postmenopausal women with RA.
Methods: We utilized data from the Rh-GIOP (Glucocorticoid-Induced Osteoporosis in Patients with chronic inflammatory Rheumatic diseases) cohort, a prospective, monocentric observational study conducted at our department. All female patients with a diagnosis of RA were included in the analysis. For assessing the association between uric acid levels and lowest (minimum) T-scores measured at the lumbar spine, hip or femur, we used linear regression with adjustment for various confounders. An interaction term was included to evaluate differential associations in pre- and postmenopausal women.
Results: A total of 206 patients with RA, available dual X-ray absorptiometry (DXA) measurements, and serum uric acid levels were included in the analysis. Of those, 167 were women, and 165 had their menopausal status documented: 16 were premenopausal (age 40.32±7.85) and 149 postmenopausal (age 64.49±9.69), respectively. Postmenopausal patients had lower T-scores than non-menopausal patients. In the analysis of the whole sample, uric acid was not associated with T-scores (slope -0.08; p=0.43), but after inclusion of the interaction term, we found that uric acid was strongly negatively associated with T-scores in premenopausal women (slope -1.02; p=0.008, figure 1).
Conclusion: Uric acid appears to be negatively associated with bone mineral density in premenopausal but not in postmenopausal women with RA. This might be due to the different effect on the bone depending on the hormone status of women. Of note, the sample size of premenopausal women with RA was small. Therefore, these findings have to be proven in a larger cohort.
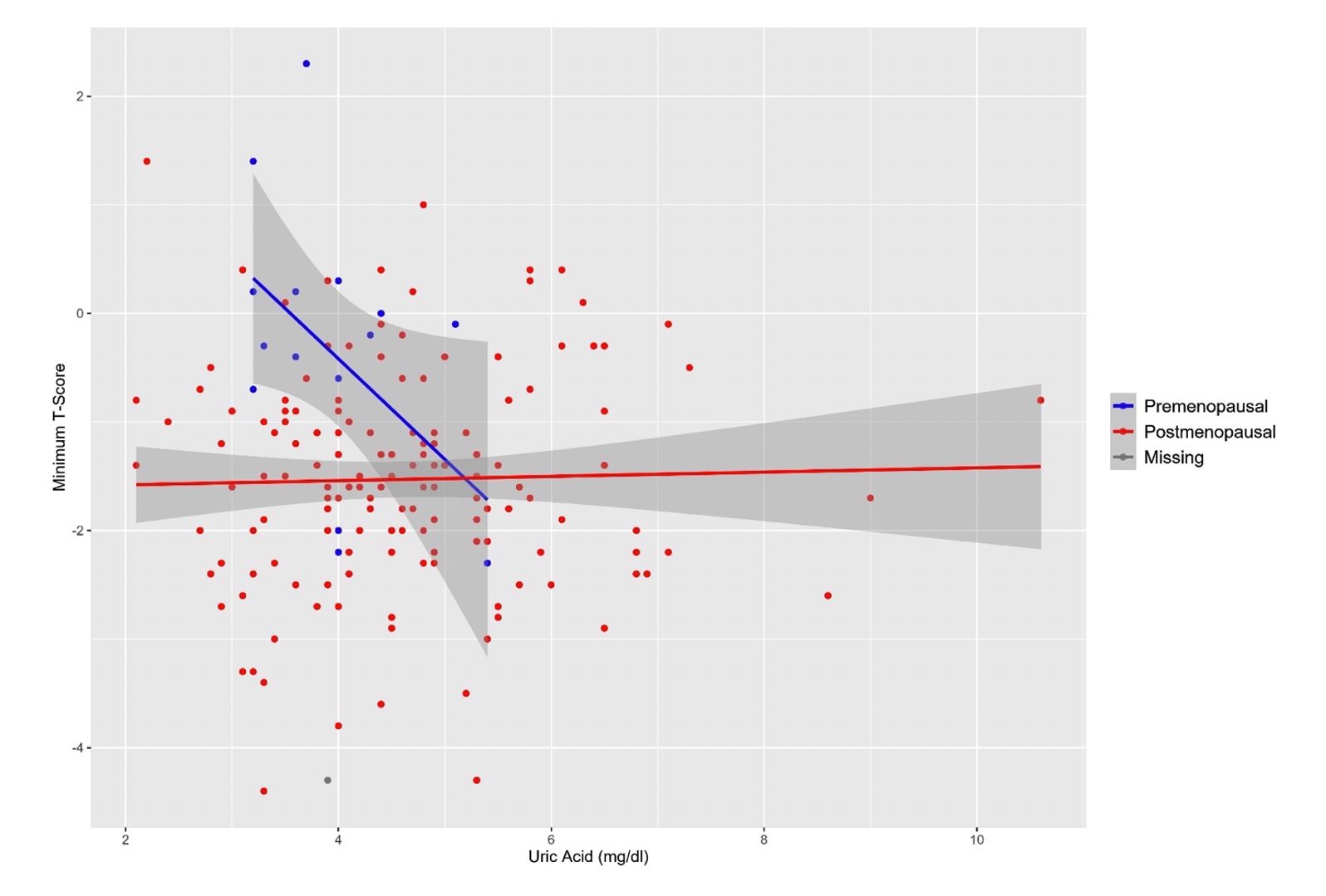 Figure 1. Scatterplot of minimum T-scores and uric acid in female rheumatoid arthritis patients stratified by menopausal status. Grey shadows surrounding the regression lines are the respective 95% confidence intervals.
Figure 1. Scatterplot of minimum T-scores and uric acid in female rheumatoid arthritis patients stratified by menopausal status. Grey shadows surrounding the regression lines are the respective 95% confidence intervals.
Disclosures: S. Hermann, AbbVie; A. Palmowski, None; B. Muche, Amgen, Gilead, Galapagos, UCB and Stadapharm, Kyowa Kirin; K. Hermann, AbbVie, Merck/MSD, Pfizer, Novartis, BerlinFlame GmbH; E. Wiebe, Medac, Novartis; F. Buttgereit, Horizon Therapeutics, Roche, Abbvie, AstraZeneca, Gruenenthal, Mundipharma, Pfizer.
Background/Purpose: Uric acid is controversially discussed regarding its effect on bone health. Higher uric acid levels have been associated with higher T-scores and fewer bone fractures in postmenopausal women. Rheumatoid arthritis (RA), as a chronic inflammatory disease, is a risk factor for fractures in both men and women. The role of uric acid in patients with RA is not yet clarified. Further, there may be different effects of uric acid on organ tissues such as the lungs, depending on the hormone status of women. We aimed at investigating the effect of uric acid level on bone mineral density and the development of osteoporosis in patients with RA and whether there is a difference between premenopausal and postmenopausal women with RA.
Methods: We utilized data from the Rh-GIOP (Glucocorticoid-Induced Osteoporosis in Patients with chronic inflammatory Rheumatic diseases) cohort, a prospective, monocentric observational study conducted at our department. All female patients with a diagnosis of RA were included in the analysis. For assessing the association between uric acid levels and lowest (minimum) T-scores measured at the lumbar spine, hip or femur, we used linear regression with adjustment for various confounders. An interaction term was included to evaluate differential associations in pre- and postmenopausal women.
Results: A total of 206 patients with RA, available dual X-ray absorptiometry (DXA) measurements, and serum uric acid levels were included in the analysis. Of those, 167 were women, and 165 had their menopausal status documented: 16 were premenopausal (age 40.32±7.85) and 149 postmenopausal (age 64.49±9.69), respectively. Postmenopausal patients had lower T-scores than non-menopausal patients. In the analysis of the whole sample, uric acid was not associated with T-scores (slope -0.08; p=0.43), but after inclusion of the interaction term, we found that uric acid was strongly negatively associated with T-scores in premenopausal women (slope -1.02; p=0.008, figure 1).
Conclusion: Uric acid appears to be negatively associated with bone mineral density in premenopausal but not in postmenopausal women with RA. This might be due to the different effect on the bone depending on the hormone status of women. Of note, the sample size of premenopausal women with RA was small. Therefore, these findings have to be proven in a larger cohort.
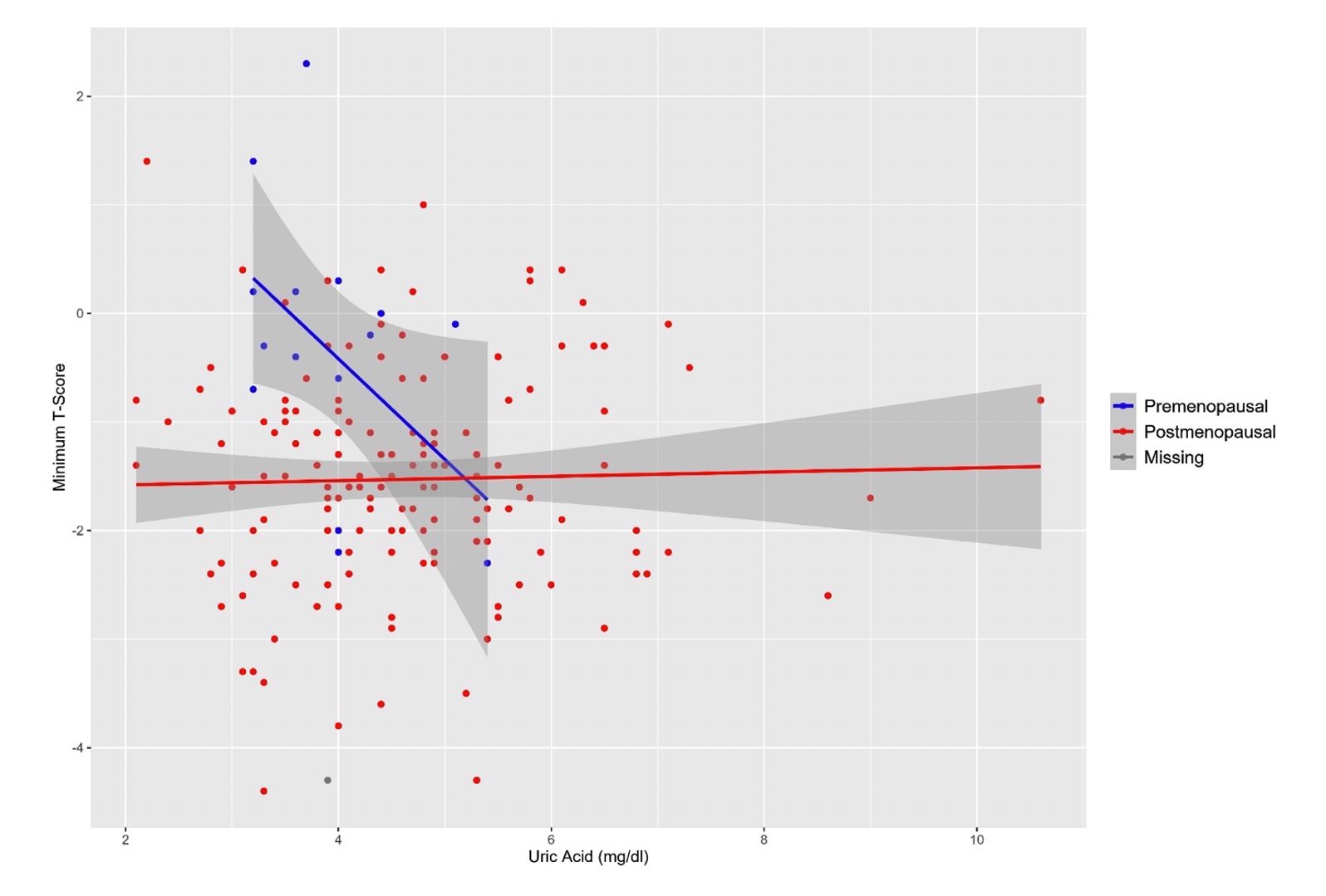 Figure 1. Scatterplot of minimum T-scores and uric acid in female rheumatoid arthritis patients stratified by menopausal status. Grey shadows surrounding the regression lines are the respective 95% confidence intervals.
Figure 1. Scatterplot of minimum T-scores and uric acid in female rheumatoid arthritis patients stratified by menopausal status. Grey shadows surrounding the regression lines are the respective 95% confidence intervals.Disclosures: S. Hermann, AbbVie; A. Palmowski, None; B. Muche, Amgen, Gilead, Galapagos, UCB and Stadapharm, Kyowa Kirin; K. Hermann, AbbVie, Merck/MSD, Pfizer, Novartis, BerlinFlame GmbH; E. Wiebe, Medac, Novartis; F. Buttgereit, Horizon Therapeutics, Roche, Abbvie, AstraZeneca, Gruenenthal, Mundipharma, Pfizer.

