Back
Poster Session D
Epidemiology, health policy and outcomes
Session: (1750–1786) Epidemiology and Public Health Poster III
1768: Sex-Related Differences in Healthcare Utilization in Patients with Inflammatory Arthritis: A Population-based Study
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- ST
Sanjana Tarannum, FCPS, MBBS, MRCP
University of Toronto
Toronto, ON, Canada
Abstract Poster Presenter(s)
Sanjana Tarannum1, Jessica Widdifield1, C. Fangyun Wang2, Sindhu R. Johnson3, Paula Rochon1 and Lihi Eder4, 1University of Toronto, Toronto, ON, Canada, 2Institute for Clinical Evaluative Sciences, Toronto, ON, Canada, 3Division of Rheumatology, Department of Medicine, Schroeder Arthritis Institute, Krembil Research Institute, Toronto Western and Mount Sinai Hospitals; Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada, 4Women’s College Research Institute, Department of Medicine, University of Toronto, Toronto, ON, Canada
Background/Purpose: Delayed diagnosis of inflammatory arthritis (IA), including rheumatoid arthritis (RA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA), is associated with joint damage and disability. Thus, timely rheumatology access is necessary for favorable disease outcomes. Sex of the patient may influence various aspects of IA including healthcare utilization patterns. Our aim was to compare patterns of musculoskeletal (MSK)-related healthcare utilization before and after diagnosis of IA between male and female patients.
Methods: We assembled 3 inception cohorts of adult RA, AS and PsA patients diagnosed between April 2010 and March 2017 using health administrative data from Ontario, Canada. Healthcare utilization in terms of visits to physicians for MSK causes, MSK imaging and laboratory tests was assessed yearly for 3 years before and 3 years after the diagnosis date and compared between male and female patients. Among individuals ≥ 66 years at the time of diagnosis, dispensation of rheumatic medications was ascertained. Regression models were used to compare healthcare utilization indicators between male and female patients after adjusting for socio-demographic factors and comorbidities. Results were reported as adjusted odds ratios (OR) for female patients compared to males.
Results: A total of 41,277 patients with RA (69% females), 8,150 patients with AS (51% females) and 6,446 patients with PsA (54% female) were analyzed. Multi-morbidity, depression and osteoporosis were more common in female patients and cardiovascular disease in male patients across the 3 cohorts.
Similar trends of sex-related differences were observed in all three IA cohorts. Female patients were more likely to visit family physicians (OR 1.03 to 1.15) and rheumatologists (OR 1.32 to 2.28) especially in earlier pre-diagnosis periods (Figure 1). Male patients were more likely to visit the emergency department immediately before diagnosis (OR 0.76 to 0.78). A similar female predominance was observed in imaging modalities of X-rays (Figure 2) and laboratory tests (OR 1.10 to 2.17) before diagnosis across the three cohorts.
Dispensation of rheumatic medications showed disease specific findings. Female AS patients were more likely to be dispensed conventional disease modifying anti-rheumatic drugs (csDMARDs) whereas female RA patients had higher odds for being dispensed NSAIDs and opioid medications. (Figure 3)
Conclusion: Female patients with IA have higher MSK-related healthcare utilization compared with male patients which may indicate sex-related, biological differences in disease course or gender-related, sociocultural differences in patient behaviour, access to care and interaction with care providers.
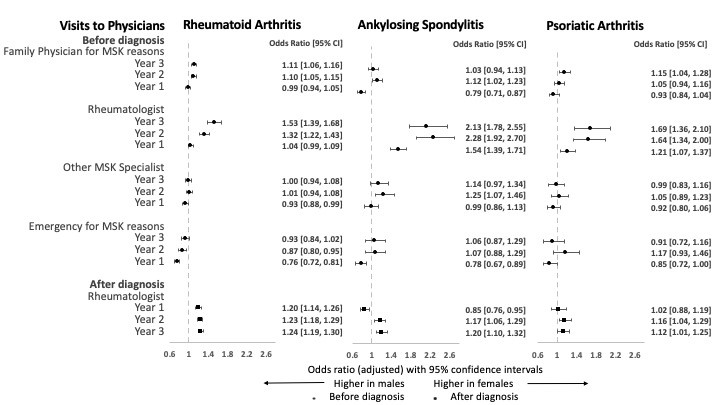 Figure 1. Adjusted odds ratios for visits to physicians for MSK reasons for female compared to male patients with IA
Figure 1. Adjusted odds ratios for visits to physicians for MSK reasons for female compared to male patients with IA
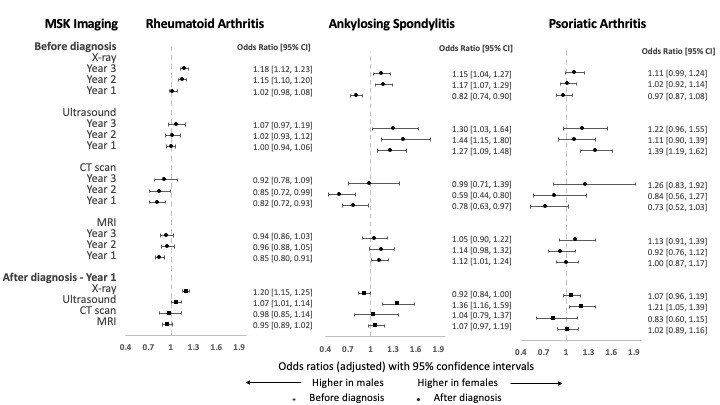 Figure 2. Adjusted odds ratios for MSK imaging for female compared to male patients with IA
Figure 2. Adjusted odds ratios for MSK imaging for female compared to male patients with IA
<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1279999-3-ANY.jpg width=440 height=247.5 border=0 style=border-style: none;>
Disclosures: S. Tarannum, None; J. Widdifield, None; C. Wang, None; S. Johnson, None; P. Rochon, None; L. Eder, AbbVie, Lilly, Novartis, UCB, Pfizer.
Background/Purpose: Delayed diagnosis of inflammatory arthritis (IA), including rheumatoid arthritis (RA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA), is associated with joint damage and disability. Thus, timely rheumatology access is necessary for favorable disease outcomes. Sex of the patient may influence various aspects of IA including healthcare utilization patterns. Our aim was to compare patterns of musculoskeletal (MSK)-related healthcare utilization before and after diagnosis of IA between male and female patients.
Methods: We assembled 3 inception cohorts of adult RA, AS and PsA patients diagnosed between April 2010 and March 2017 using health administrative data from Ontario, Canada. Healthcare utilization in terms of visits to physicians for MSK causes, MSK imaging and laboratory tests was assessed yearly for 3 years before and 3 years after the diagnosis date and compared between male and female patients. Among individuals ≥ 66 years at the time of diagnosis, dispensation of rheumatic medications was ascertained. Regression models were used to compare healthcare utilization indicators between male and female patients after adjusting for socio-demographic factors and comorbidities. Results were reported as adjusted odds ratios (OR) for female patients compared to males.
Results: A total of 41,277 patients with RA (69% females), 8,150 patients with AS (51% females) and 6,446 patients with PsA (54% female) were analyzed. Multi-morbidity, depression and osteoporosis were more common in female patients and cardiovascular disease in male patients across the 3 cohorts.
Similar trends of sex-related differences were observed in all three IA cohorts. Female patients were more likely to visit family physicians (OR 1.03 to 1.15) and rheumatologists (OR 1.32 to 2.28) especially in earlier pre-diagnosis periods (Figure 1). Male patients were more likely to visit the emergency department immediately before diagnosis (OR 0.76 to 0.78). A similar female predominance was observed in imaging modalities of X-rays (Figure 2) and laboratory tests (OR 1.10 to 2.17) before diagnosis across the three cohorts.
Dispensation of rheumatic medications showed disease specific findings. Female AS patients were more likely to be dispensed conventional disease modifying anti-rheumatic drugs (csDMARDs) whereas female RA patients had higher odds for being dispensed NSAIDs and opioid medications. (Figure 3)
Conclusion: Female patients with IA have higher MSK-related healthcare utilization compared with male patients which may indicate sex-related, biological differences in disease course or gender-related, sociocultural differences in patient behaviour, access to care and interaction with care providers.
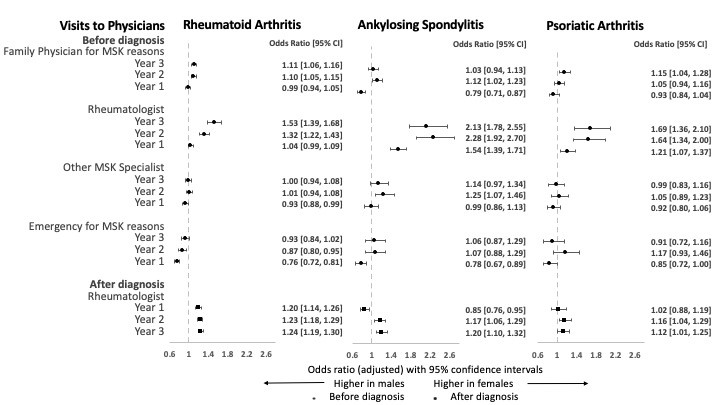 Figure 1. Adjusted odds ratios for visits to physicians for MSK reasons for female compared to male patients with IA
Figure 1. Adjusted odds ratios for visits to physicians for MSK reasons for female compared to male patients with IA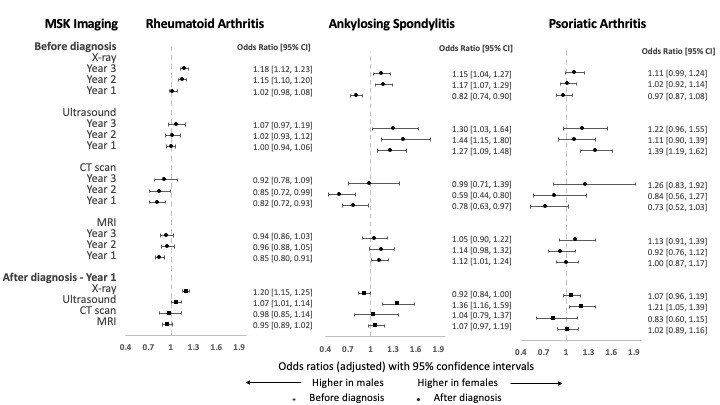 Figure 2. Adjusted odds ratios for MSK imaging for female compared to male patients with IA
Figure 2. Adjusted odds ratios for MSK imaging for female compared to male patients with IA<img src=https://www.abstractscorecard.com/uploads/Tasks/upload/17574/QHOPTGBB-1279999-3-ANY.jpg width=440 height=247.5 border=0 style=border-style: none;>
Figure 3. Adjusted odds ratios for dispensation of medications for female compared to male older patients with IA (age>65)
Disclosures: S. Tarannum, None; J. Widdifield, None; C. Wang, None; S. Johnson, None; P. Rochon, None; L. Eder, AbbVie, Lilly, Novartis, UCB, Pfizer.

