Back
Poster Session D
Sjögren's syndrome
Session: (2017–2051) Sjögren's Syndrome – Basic and Clinical Science Poster
2049: ILD Associated with Primary Sjögren’s Syndrome Is Frequently Progressive
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AH
Anna-Maria Hoffmann-Vold, MD, PhD
Oslo University Hospital
Oslo, Norway
Abstract Poster Presenter(s)
Anna-Maria Hoffmann-Vold1, Håvard Fretheim1, Phoung Phoung Diep1, Karoline Lerang2, Birgir Gudbransson1, Helena Andersson1, Øyvind Midtvedt1, Torhild Garen1, Michael Durheim1, Trond Mogens Aaløkken1, Øyvind Palm1 and Øyvind Molberg2, 1Oslo University Hospital, Oslo, Norway, 2Department of Rheumatology, Oslo University Hospital, Oslo, Norway, Oslo, Norway
Background/Purpose: Interstitial lung disease (ILD) in primary Sjögren's syndrome (pSS) has been reported to be present in 10-15% of patients, but ILD progression in pSS-ILD has not been assessed in detail. The objective of this study was to assess ILD progression in pSS and factors associated with disease progression in a well-characterized pSS-ILD cohort.
Methods: All pSS patients with ILD diagnosed on HRCT from the Oslo University Hospital (OUH) were included. Clinical characteristics, treatment (including rituximab, other immunosuppressives, hydroxychloroquine, nintedanib and lung transplantation), lung function tests including forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO), and ILD pattern on HRCT assessed by a radiologist were evaluated. We determined ILD progression defined as (1) absolute FVC decline >5%; or (2) absolute DLCO decline >10% over 12 +/-6 months; or (3) increasing extent of ILD on HRCT over the observation period. Potential risk factors associated with disease progression were chosen based on expert opinion. Descriptive analyses were conducted.
Results: Of 702 pSS patients followed at OUH, we identified 60 pSS patients with ILD with 33 (55%) having followup at 12 months (Table). Mean time from pSS to ILD diagnosis was 7.4 years. In 67% ILD was diagnosed after pSS, in 13% simultaneously, and in 11% before pSS diagnosis. In total, 28 (47%) had lymphocytic interstitial pneumonia (LIP) and 32 (53%) reticular pattern on HRCT. Of all, 33 (53%) were treated (Table). Over mean followup of 10.9 months (SD 4.2), 7/33 (21%) showed FVC >5% decline, 9/32 (28%) DLCO >10% decline and 12 (36%) had at least one of these defined lung function declines on standard of care treatment (Figure 1). Over an observation period of 15.4 (SD 10.6) years, 27/47 (45%) showed any ILD progression on HRCT (Figure 1). HRCT pattern was not associated with risk of >10% DLCO decline or ILD progression on HCRT. >5% FVC decline occurred more frequently in patients with reticular pattern compared to LIP (6/17 (35%) vs 1/16 (6%), p=0.041). Factors significantly associated with ILD progression on lung function (either FVC eller DLCO decline) included higher baseline FVC (99% (SD16.4) vs 87% (SD14.9), p=0.032), higher DLCO (81% (SD13.1) vs 67% (SD17.4), p=0.020), increased CRP (2/10 (20%) vs 0/16 (0%), p=0.045), presence of polyneuropathy (2/9 (22%) vs 1/17 (6%), p=0.045) and numerically male sex (2/12 (25%) vs 1/21 (6%), p=0.087) (Figure 2). Treatment was not associated with ILD progression.
Conclusion: A substantial number of patients with pSS-ILD progressed on standard of care treatment. This highlights the importance of close monitoring and active consideration of treatment initiation and escalation in pSS-ILD.
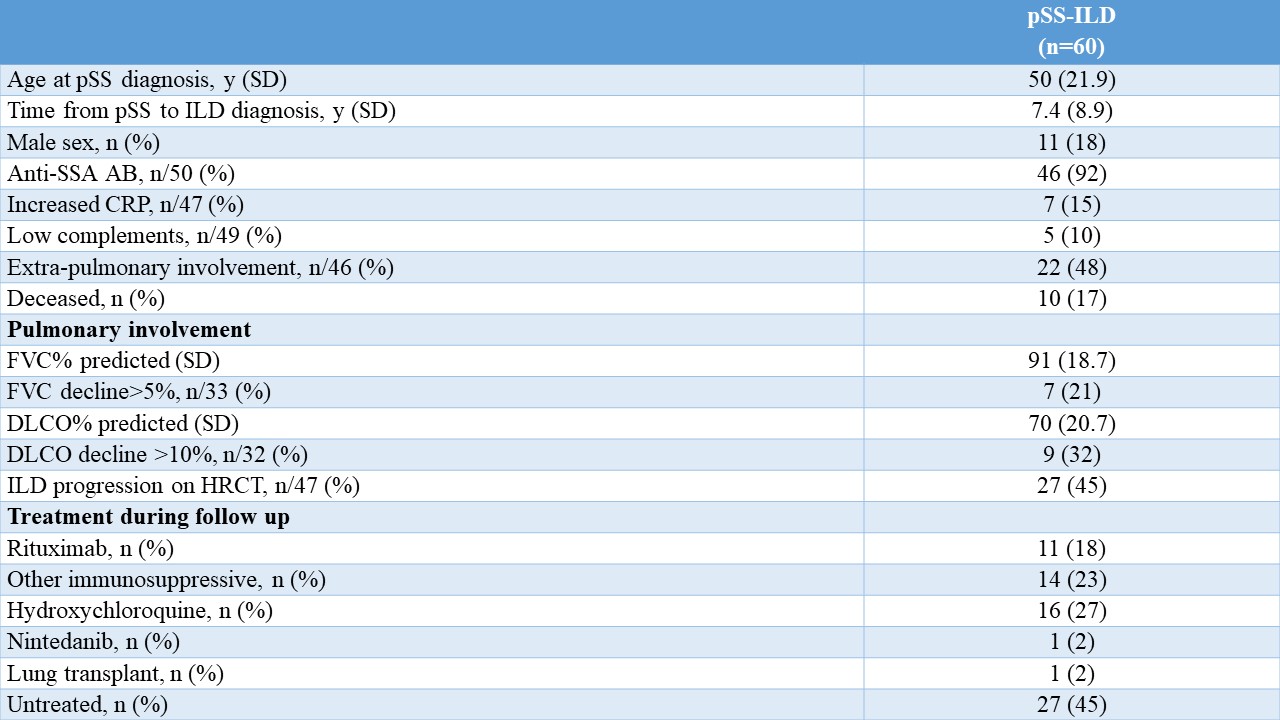 Table1: Clinical characteristics, demographics and outcome of pSS with ILD
Table1: Clinical characteristics, demographics and outcome of pSS with ILD
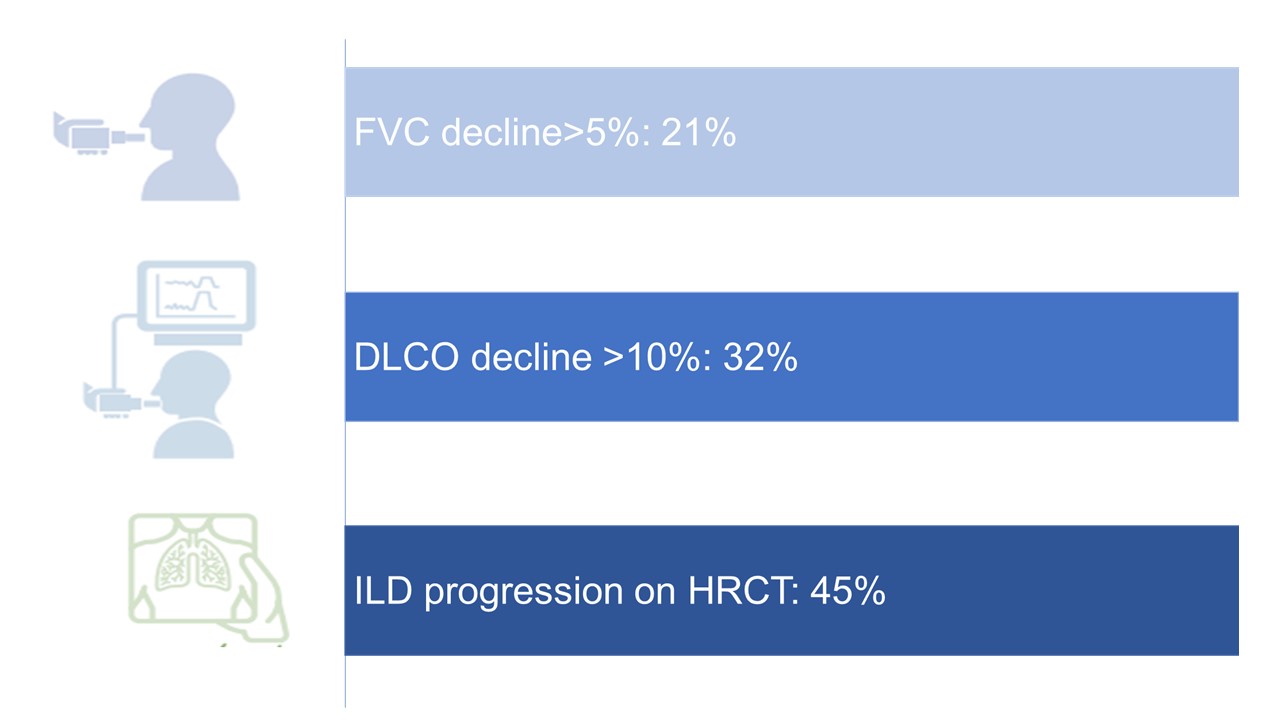 Figure 1: ILD progression in pSS
Figure 1: ILD progression in pSS
.jpg) Figure 2: Baseline characteristics significantly associated with ILD progression in pSS-ILD
Figure 2: Baseline characteristics significantly associated with ILD progression in pSS-ILD
Disclosures: A. Hoffmann-Vold, Boehringer-Ingelheim, Janssen, Eli Lilly, Merck/MSD, Roche; H. Fretheim, Bayer, GSK and Actelion; P. Diep, Boehringer Ingelheim; K. Lerang, None; B. Gudbransson, None; H. Andersson, Boehringer Ingelheim; Ø. Midtvedt, Jannsen, Boehringer-Ingelheim; T. Garen, None; M. Durheim, Boehringer Ingelheim, Roche; T. Aaløkken, Boehringer Ingelheim; Ø. Palm, None; Ø. Molberg, None.
Background/Purpose: Interstitial lung disease (ILD) in primary Sjögren's syndrome (pSS) has been reported to be present in 10-15% of patients, but ILD progression in pSS-ILD has not been assessed in detail. The objective of this study was to assess ILD progression in pSS and factors associated with disease progression in a well-characterized pSS-ILD cohort.
Methods: All pSS patients with ILD diagnosed on HRCT from the Oslo University Hospital (OUH) were included. Clinical characteristics, treatment (including rituximab, other immunosuppressives, hydroxychloroquine, nintedanib and lung transplantation), lung function tests including forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO), and ILD pattern on HRCT assessed by a radiologist were evaluated. We determined ILD progression defined as (1) absolute FVC decline >5%; or (2) absolute DLCO decline >10% over 12 +/-6 months; or (3) increasing extent of ILD on HRCT over the observation period. Potential risk factors associated with disease progression were chosen based on expert opinion. Descriptive analyses were conducted.
Results: Of 702 pSS patients followed at OUH, we identified 60 pSS patients with ILD with 33 (55%) having followup at 12 months (Table). Mean time from pSS to ILD diagnosis was 7.4 years. In 67% ILD was diagnosed after pSS, in 13% simultaneously, and in 11% before pSS diagnosis. In total, 28 (47%) had lymphocytic interstitial pneumonia (LIP) and 32 (53%) reticular pattern on HRCT. Of all, 33 (53%) were treated (Table). Over mean followup of 10.9 months (SD 4.2), 7/33 (21%) showed FVC >5% decline, 9/32 (28%) DLCO >10% decline and 12 (36%) had at least one of these defined lung function declines on standard of care treatment (Figure 1). Over an observation period of 15.4 (SD 10.6) years, 27/47 (45%) showed any ILD progression on HRCT (Figure 1). HRCT pattern was not associated with risk of >10% DLCO decline or ILD progression on HCRT. >5% FVC decline occurred more frequently in patients with reticular pattern compared to LIP (6/17 (35%) vs 1/16 (6%), p=0.041). Factors significantly associated with ILD progression on lung function (either FVC eller DLCO decline) included higher baseline FVC (99% (SD16.4) vs 87% (SD14.9), p=0.032), higher DLCO (81% (SD13.1) vs 67% (SD17.4), p=0.020), increased CRP (2/10 (20%) vs 0/16 (0%), p=0.045), presence of polyneuropathy (2/9 (22%) vs 1/17 (6%), p=0.045) and numerically male sex (2/12 (25%) vs 1/21 (6%), p=0.087) (Figure 2). Treatment was not associated with ILD progression.
Conclusion: A substantial number of patients with pSS-ILD progressed on standard of care treatment. This highlights the importance of close monitoring and active consideration of treatment initiation and escalation in pSS-ILD.
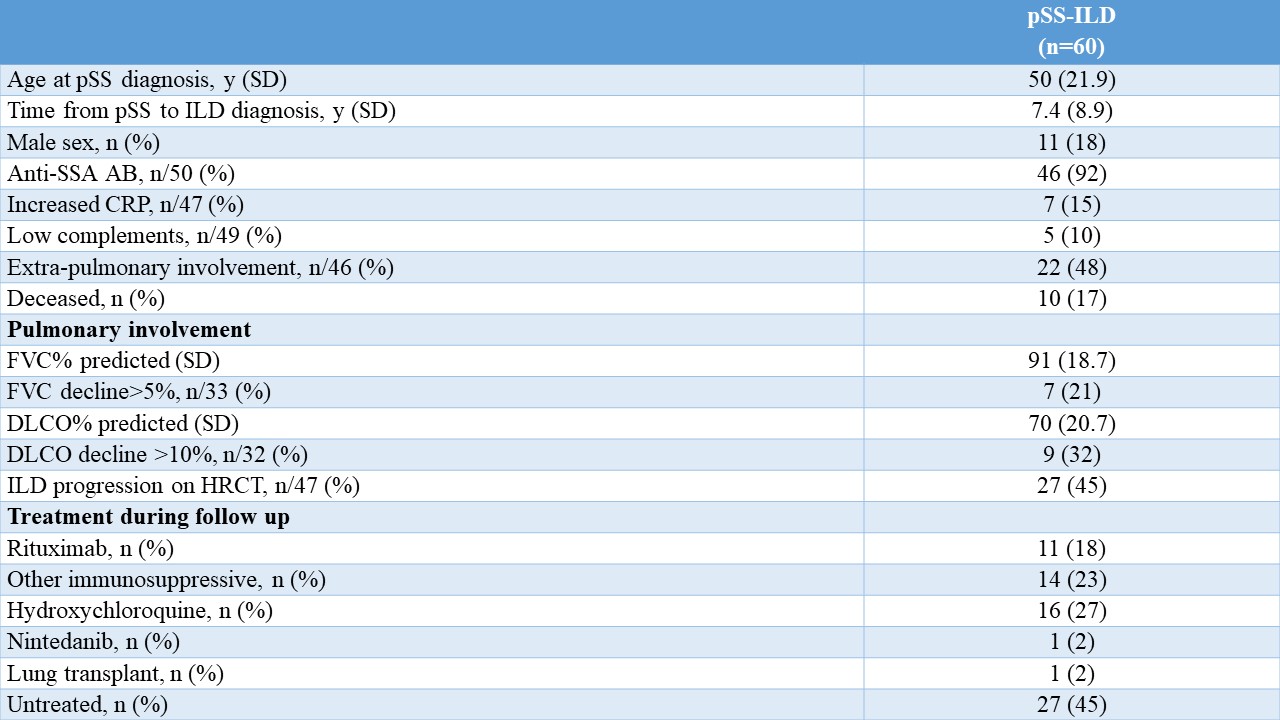 Table1: Clinical characteristics, demographics and outcome of pSS with ILD
Table1: Clinical characteristics, demographics and outcome of pSS with ILD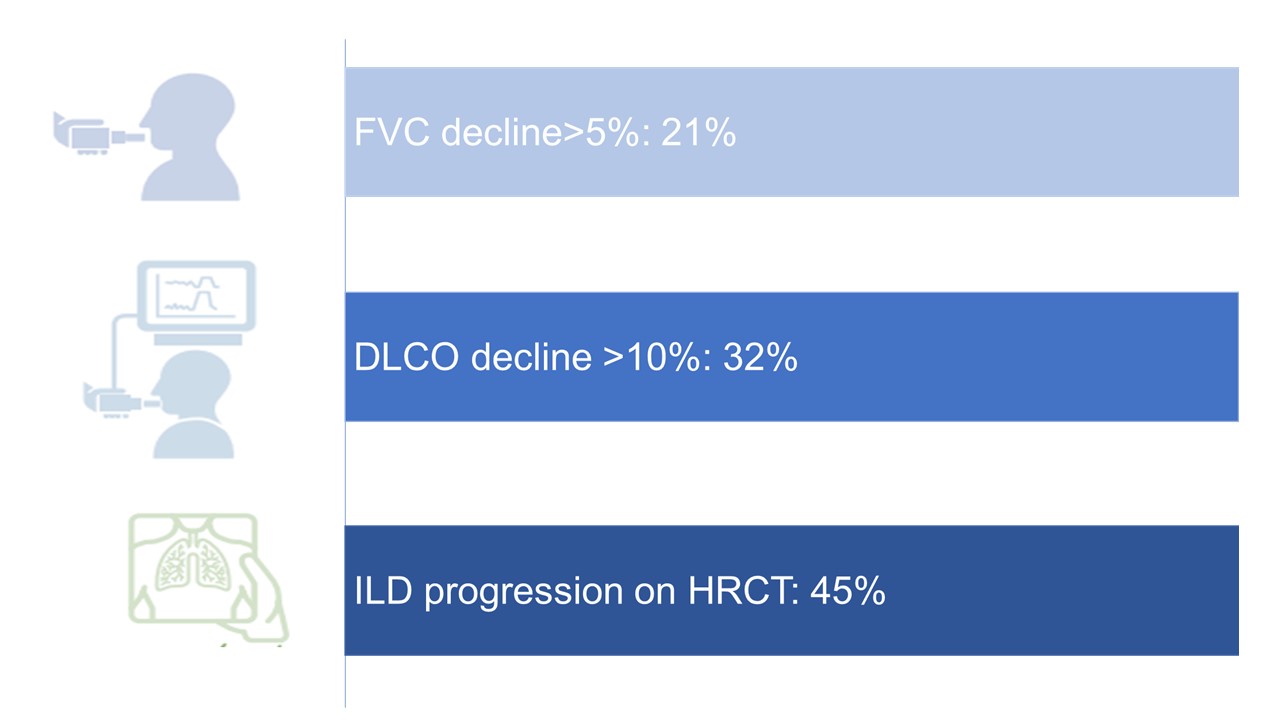 Figure 1: ILD progression in pSS
Figure 1: ILD progression in pSS.jpg) Figure 2: Baseline characteristics significantly associated with ILD progression in pSS-ILD
Figure 2: Baseline characteristics significantly associated with ILD progression in pSS-ILDDisclosures: A. Hoffmann-Vold, Boehringer-Ingelheim, Janssen, Eli Lilly, Merck/MSD, Roche; H. Fretheim, Bayer, GSK and Actelion; P. Diep, Boehringer Ingelheim; K. Lerang, None; B. Gudbransson, None; H. Andersson, Boehringer Ingelheim; Ø. Midtvedt, Jannsen, Boehringer-Ingelheim; T. Garen, None; M. Durheim, Boehringer Ingelheim, Roche; T. Aaløkken, Boehringer Ingelheim; Ø. Palm, None; Ø. Molberg, None.

