Back
Poster Session D
Osteoarthritis (OA) and related disorders
Session: (1888–1923) Osteoarthritis – Clinical Poster
1906: Bile Acid Profile Is Associated to Synovitis in Knee Osteoarthritis
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Jessica Murillo Saich, PhD, BSc
University of California San Diego
La Jolla, CA, United States
Abstract Poster Presenter(s)
Roxana Coras1, Jessica Murillo Saich2, Michal Hose Sanchez3, Anne Quan3, Emily Gentry1, Pieter Dorrestein1, Nancy Lane4 and Monica Guma5, 1University of California San Diego, San Diego, CA, 2University of California San Diego, La Jolla, CA, 3VA San Diego Healthcare System, San Diego, CA, 4University of California Davis, Hillsborough, CA, 5Division of Rheumatology, Allergy, and Immunology, Department of Medicine, University of California San Diego, La Jolla, CA
Background/Purpose: Increasing evidence indicates that low grade systemic and local inflammation contributes to osteoarthritis (OA) progression. Bioactive lipid mediators are signaling molecules involved in inflammatory processes. Among them, bile acids (BAs) are signaling molecules that regulate various cellular processes. Gut bacteria metabolize primary BAs such as chenodeoxycholic and cholic acid, which are synthesized in the liver from cholesterol, to secondary BAs such as deoxycholic and lithocholic acid. BAs modulate intestinal permeability and have been detected in the systemic circulation and related to insulin resistance and homeostasis of the mucosal immune function in the gut. However, the role of BAs in OA has not been explored.
Methods: Twenty-eight patients with a diagnosis of radiographic knee OA (KOA) with Kellgren and Lawrence (KL) ³ 2 were recruited in our study A thorough clinical examination was conducted. Patients completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire. Ultrasound examination (US) for effusion, synovial hypertrophy, popliteal cysts, and power Doppler (PD) signal within the synovium was performed. PD assessment was focused on areas of synovial hypertrophy and recorded as absent or present. Synovitis was defined as the presence of synovial hypertrophy and or/effusion and scored from 0 to 3, according to the OMERACT guidelines. Patients were stratified by degree of synovitis in low-grade (scores 0 and 1) and high-grade (scores 2 and 3). Plasma LPB (Lipopolysaccharide LPS-binding protein) was measured by ELISA (ng/ml). Plasma BA profiling was determined by mass spectrometry. Data processing and statistical analysis were performed in R and Metaboanalyst.
Results: Plasma from twenty-eight older adults (average age 65.4 (SD 8.01), 64% males, body mass index (BMI); 30.9 (SD 5.1)) were analyzed. Ultrasound examination classified 16 patients as having low-grade whereas 12 had high-grade synovitis. Figure 1 shows a partial least-squares discriminant analysis (PLS-DA) with all identified BAs that achieved partial discrimination among the groups, with several BAs that were dysregulated in the group with high-grade synovitis. Plasma LBP concentration was significantly increased in samples with high-grade synovitis (4456 ±1184 vs 3180±1309, p=0.01 in high vs low-grade synovitis respectively). Moreover, circulating BAs were associated with OA outcome scores. The association with cholic acid and the WOMAC score (r=0.44, p=0.01) was the strongest. Interestingly, BAs were also associated with synovitis (glycoursodeoxycholic acid, r=0.39, p=0.04), BMI (taurocholic acid, r=0.38, p=0.05) and with LBP, a biomarker of KOA progression (cholic acid, r=0.41, p=0.03). These associations differed between obese (BMI >30) and non-obese subjects (Figure 2).
Conclusion: We have identified several BAs that are associated with high-grade synovitis, BMI, and LPS binding protein, suggesting that gut-microbiome derived BAs may be not only key mediators of OA development and progression, but also predict KOA progression by identifying subjects with synovial inflammation and altered microbiome and intestinal permeability.
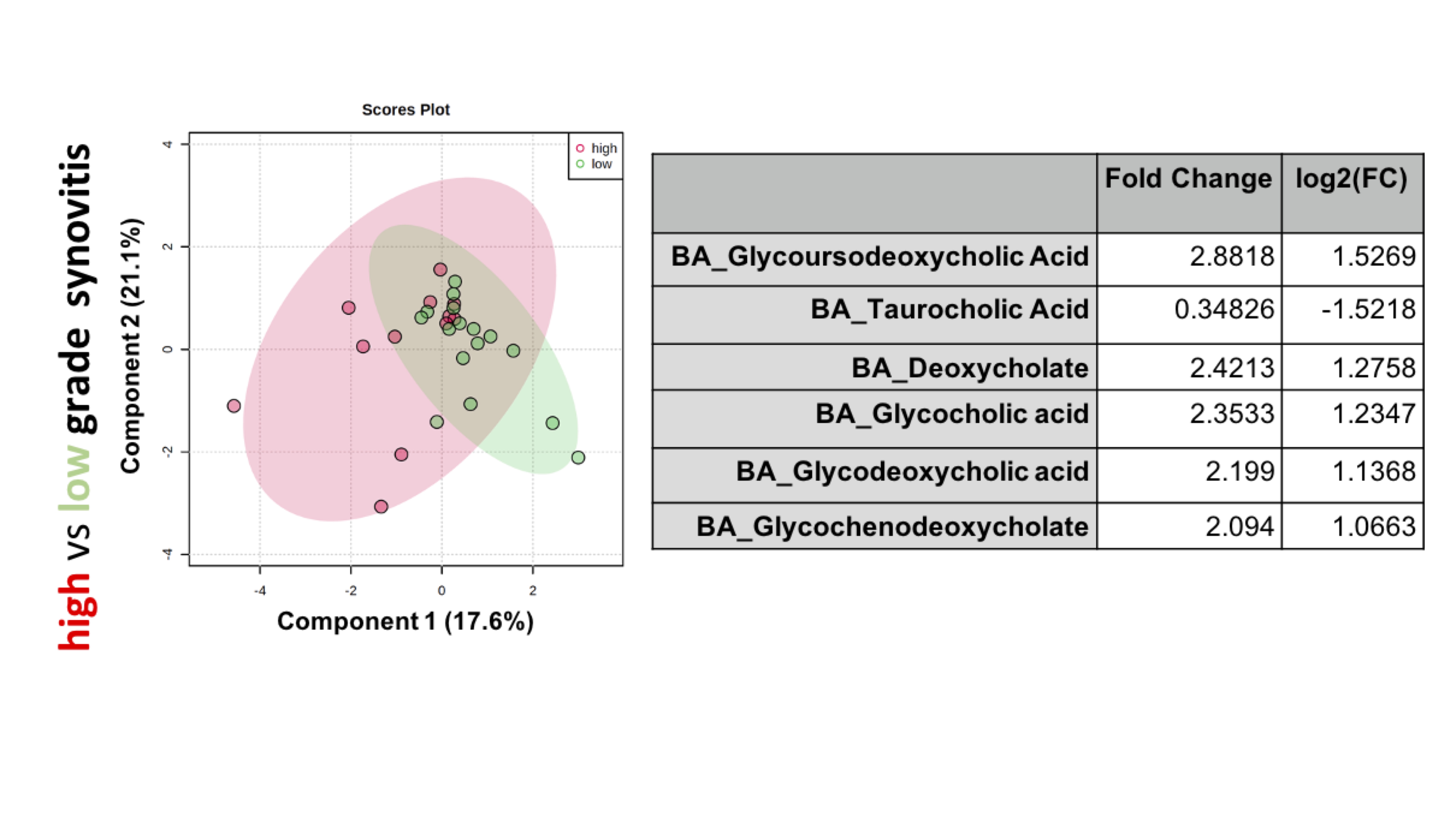 Figure 1. BA profiling in KOA patients. Partial least-squares discriminant analysis (PLS/DA) of KOA patients with high-grade synovitis (red) versus low-grade synovitis KOA (green). Right shows top BAs with significant fold change between samples with high versus low-grade synovitis adjusted by age, sex and BMI.
Figure 1. BA profiling in KOA patients. Partial least-squares discriminant analysis (PLS/DA) of KOA patients with high-grade synovitis (red) versus low-grade synovitis KOA (green). Right shows top BAs with significant fold change between samples with high versus low-grade synovitis adjusted by age, sex and BMI.
.jpg) Figure 2. Pearson correlation coefficients between some of the identified BAs and clinical scores, synovitis (scored by ultrasound), and LBP (ng/ml) (measured by ELISA) in obese and non-obese KOA patients.
Figure 2. Pearson correlation coefficients between some of the identified BAs and clinical scores, synovitis (scored by ultrasound), and LBP (ng/ml) (measured by ELISA) in obese and non-obese KOA patients.
Disclosures: R. Coras, None; J. Murillo Saich, None; M. Sanchez, None; A. Quan, None; E. Gentry, None; P. Dorrestein, None; N. Lane, Amgen, GlaxoSmithKlein(GSK); M. Guma, Novartis, Pfizer, Gilead, Genentech, Sonoma Biotherapeutics.
Background/Purpose: Increasing evidence indicates that low grade systemic and local inflammation contributes to osteoarthritis (OA) progression. Bioactive lipid mediators are signaling molecules involved in inflammatory processes. Among them, bile acids (BAs) are signaling molecules that regulate various cellular processes. Gut bacteria metabolize primary BAs such as chenodeoxycholic and cholic acid, which are synthesized in the liver from cholesterol, to secondary BAs such as deoxycholic and lithocholic acid. BAs modulate intestinal permeability and have been detected in the systemic circulation and related to insulin resistance and homeostasis of the mucosal immune function in the gut. However, the role of BAs in OA has not been explored.
Methods: Twenty-eight patients with a diagnosis of radiographic knee OA (KOA) with Kellgren and Lawrence (KL) ³ 2 were recruited in our study A thorough clinical examination was conducted. Patients completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire. Ultrasound examination (US) for effusion, synovial hypertrophy, popliteal cysts, and power Doppler (PD) signal within the synovium was performed. PD assessment was focused on areas of synovial hypertrophy and recorded as absent or present. Synovitis was defined as the presence of synovial hypertrophy and or/effusion and scored from 0 to 3, according to the OMERACT guidelines. Patients were stratified by degree of synovitis in low-grade (scores 0 and 1) and high-grade (scores 2 and 3). Plasma LPB (Lipopolysaccharide LPS-binding protein) was measured by ELISA (ng/ml). Plasma BA profiling was determined by mass spectrometry. Data processing and statistical analysis were performed in R and Metaboanalyst.
Results: Plasma from twenty-eight older adults (average age 65.4 (SD 8.01), 64% males, body mass index (BMI); 30.9 (SD 5.1)) were analyzed. Ultrasound examination classified 16 patients as having low-grade whereas 12 had high-grade synovitis. Figure 1 shows a partial least-squares discriminant analysis (PLS-DA) with all identified BAs that achieved partial discrimination among the groups, with several BAs that were dysregulated in the group with high-grade synovitis. Plasma LBP concentration was significantly increased in samples with high-grade synovitis (4456 ±1184 vs 3180±1309, p=0.01 in high vs low-grade synovitis respectively). Moreover, circulating BAs were associated with OA outcome scores. The association with cholic acid and the WOMAC score (r=0.44, p=0.01) was the strongest. Interestingly, BAs were also associated with synovitis (glycoursodeoxycholic acid, r=0.39, p=0.04), BMI (taurocholic acid, r=0.38, p=0.05) and with LBP, a biomarker of KOA progression (cholic acid, r=0.41, p=0.03). These associations differed between obese (BMI >30) and non-obese subjects (Figure 2).
Conclusion: We have identified several BAs that are associated with high-grade synovitis, BMI, and LPS binding protein, suggesting that gut-microbiome derived BAs may be not only key mediators of OA development and progression, but also predict KOA progression by identifying subjects with synovial inflammation and altered microbiome and intestinal permeability.
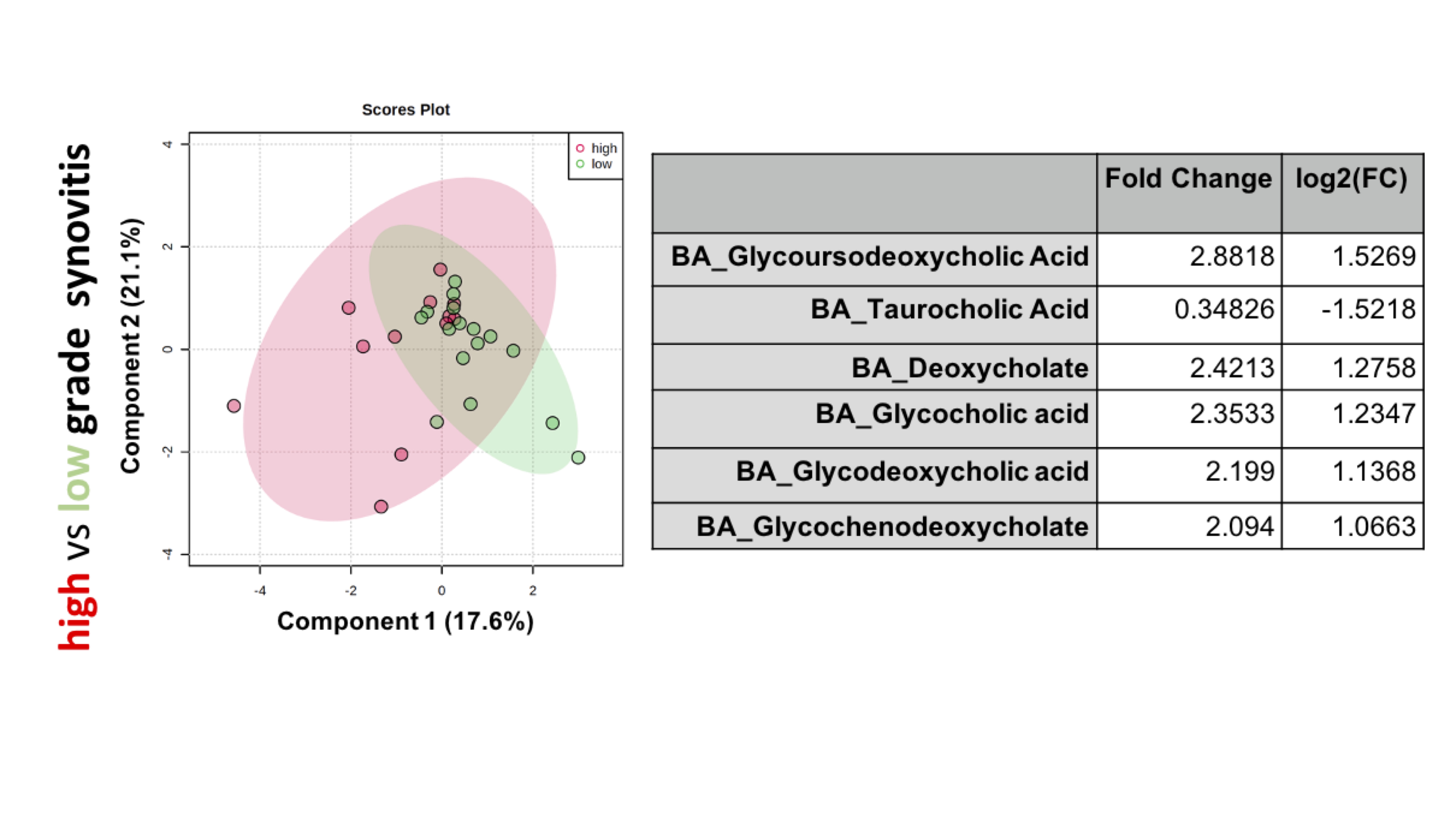 Figure 1. BA profiling in KOA patients. Partial least-squares discriminant analysis (PLS/DA) of KOA patients with high-grade synovitis (red) versus low-grade synovitis KOA (green). Right shows top BAs with significant fold change between samples with high versus low-grade synovitis adjusted by age, sex and BMI.
Figure 1. BA profiling in KOA patients. Partial least-squares discriminant analysis (PLS/DA) of KOA patients with high-grade synovitis (red) versus low-grade synovitis KOA (green). Right shows top BAs with significant fold change between samples with high versus low-grade synovitis adjusted by age, sex and BMI..jpg) Figure 2. Pearson correlation coefficients between some of the identified BAs and clinical scores, synovitis (scored by ultrasound), and LBP (ng/ml) (measured by ELISA) in obese and non-obese KOA patients.
Figure 2. Pearson correlation coefficients between some of the identified BAs and clinical scores, synovitis (scored by ultrasound), and LBP (ng/ml) (measured by ELISA) in obese and non-obese KOA patients.Disclosures: R. Coras, None; J. Murillo Saich, None; M. Sanchez, None; A. Quan, None; E. Gentry, None; P. Dorrestein, None; N. Lane, Amgen, GlaxoSmithKlein(GSK); M. Guma, Novartis, Pfizer, Gilead, Genentech, Sonoma Biotherapeutics.

