Back
Poster Session D
Epidemiology, health policy and outcomes
Session: (1750–1786) Epidemiology and Public Health Poster III
1784: Gait Alterations Associated with Worsening Physical Function over 2 Years: A Machine-learning Approach in the Multicenter Osteoarthritis (MOST) Study
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Kathryn Bacon, PhD, MPH
Boston University
Boston, MA, United States
Abstract Poster Presenter(s)
Kathryn Bacon1, David Felson1, S. Reza Jafarzadeh2, Vijaya Kolachalama2, Jeffrey Hausdorff3, Eran Gazit4, Joshua Stefanik5, Patrick Corrigan6, Neil Segal7, Cora E. Lewis8, Michael Nevitt9 and Deepak Kumar1, 1Boston University, Boston, MA, 2Boston University School of Medicine, Boston, MA, 3Tel Aviv University, Tel Aviv, Israel, 4Tel Aviv Suarasky Medical Center, Tel Aviv, Israel, 5Northeastern University, Boston, MA, 6Saint Louis University, St. Louis, MO, 7University of Kansas, Kansas City, KS, 8University of Alabama at Birmingham, Birmingham, AL, 9University of California at San Francisco, Orinda, CA
Background/Purpose: Altered gait is related to pathogenesis of knee osteoarthritis (OA). For people with knee OA, in addition to pain, declines in physical function are a key reason for seeking medical care. Studies have suggested that low cadence, which increases some loading parameters, may be associated with cartilage damage. It is not known whether this or other gait alterations are related to decline in physical function in people with knee OA, and further, whether these relationships are mediated by changes in pain. We applied machine learning (ML) approaches to gait data in MOST to identify markers of gait alterations in people with worsening physical function over 2 years, and tested mediation by pain.
Methods: MOST participants were age 45-90 with, or at risk for, knee OA. Gait was assessed using inertial measurement units (OPAL, APDM, Portland, OR) worn on the trunk and both ankles during a 20-meter walk test at a self-selected speed. Participants were categorized by the outcome, worsening physical function, defined as MCID increase in WOMAC physical function score (4+ points on 0-68 scale ) over 2-years.
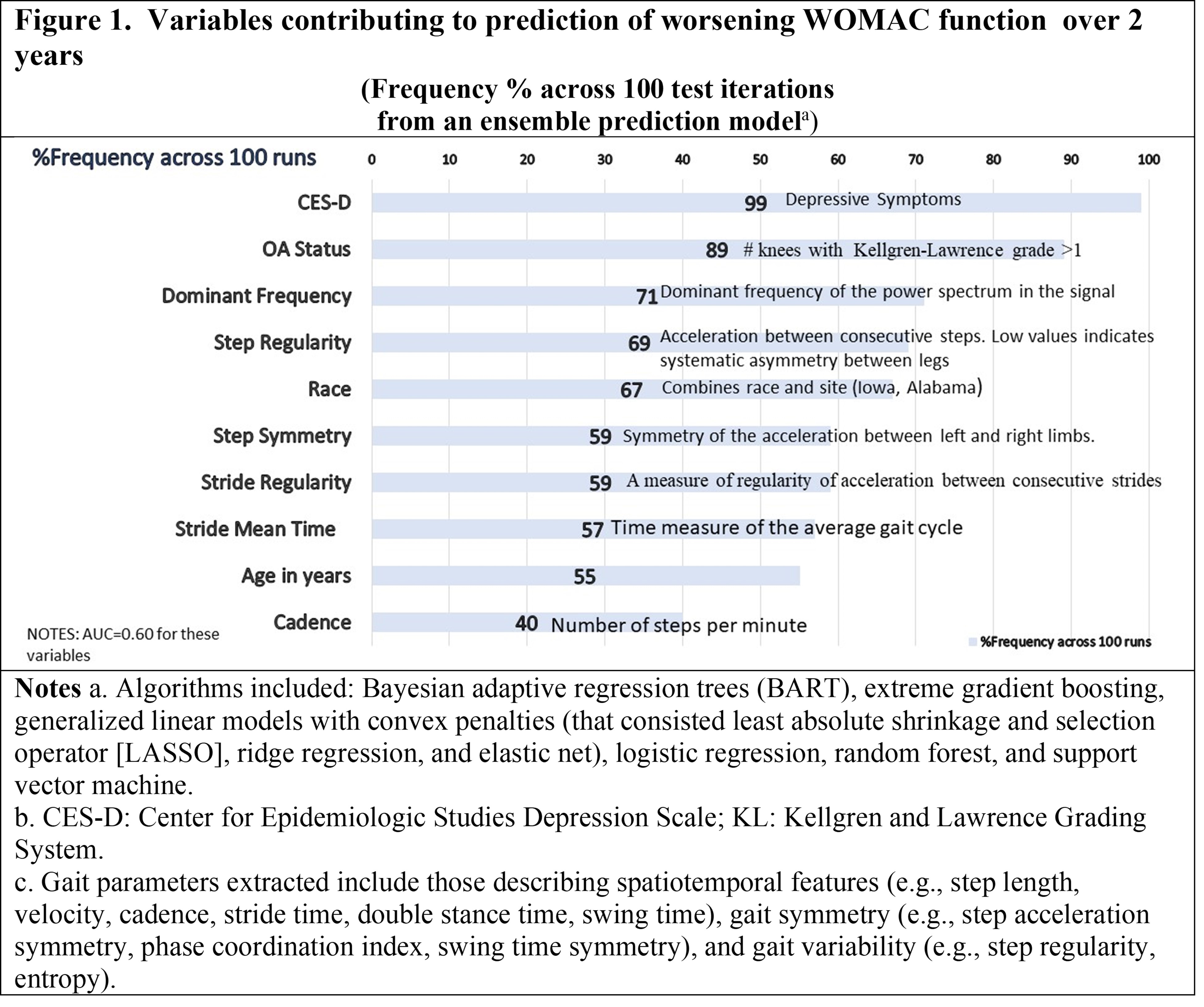
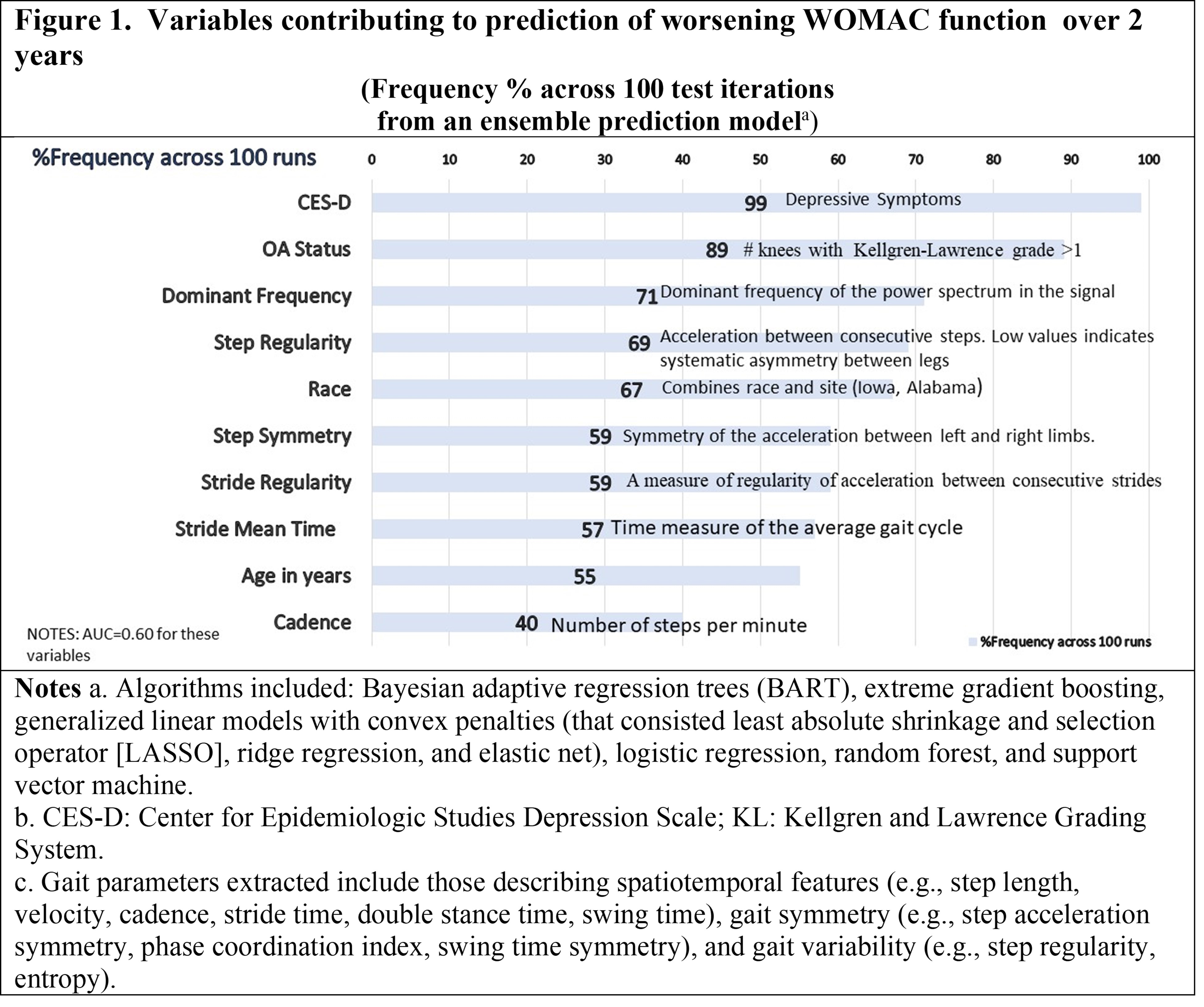
We used an ensemble machine learning technique (“super learning”) with multiple algorithms (Figure 1 footnote) to optimally discriminate between those with and without the outcome. Variables included as possible predictors in the ML process included person-level gait variables , person-level OA status (# of knees with K-L grade >1), age, BMI, depressive symptoms (CES-D), and race. Data were randomly split into 70% training and 30% test sets; data split, model training and testing were repeated 100 times. We used a variable importance statistic to identify the 10 most influential variables that most frequently contributed to the prediction of worsening physical function. Log-binomial regression evaluated associations of these variables with MCID change in WOMAC function over 2 years. Continuous variables were standardized. As changes in function could be related to pain, we also tested for mediation by MCID change in WOMAC pain over 2 years.
Results: Of 2324 participants (mean age 63.6 [SD: 10.5] years, 57% female). 24% had worsening WOMAC function over 2 years by MCID change. Figure 1 lists top contributing variables from the ensemble ML process (AUC=0.60).
Lower cadence (Figure 2) was associated with worsening function over 2 years. Also associated with worsening function were depressive symptoms, older age, radiographic OA, and clinic site. MCID change in WOMAC pain mediated the association of cadence and worsening function over 2 years, accounting for approximately 34% of the total effect of cadence on worsening function.
Conclusion: Our results suggest lower cadence is associated with worsening physical function over 2 years in individuals with, or at risk for, knee OA, a minority of which is mediated by changes in pain. Further support comes from observations that in people with hip OA who receive a biomechanical intervention, improvements in cadence are related to improved WOMAC Function scores. Interventions that target cadence in people with knee OA may lead to improvements in physical function.
.jpg)
Disclosures: K. Bacon, None; D. Felson, None; S. Jafarzadeh, None; V. Kolachalama, None; J. Hausdorff, None; E. Gazit, None; J. Stefanik, None; P. Corrigan, None; N. Segal, Pacira Biosciences, Integra LifeSciences, Trice Medical; C. Lewis, None; M. Nevitt, None; D. Kumar, Pfizer, Eli Lilly.
Background/Purpose: Altered gait is related to pathogenesis of knee osteoarthritis (OA). For people with knee OA, in addition to pain, declines in physical function are a key reason for seeking medical care. Studies have suggested that low cadence, which increases some loading parameters, may be associated with cartilage damage. It is not known whether this or other gait alterations are related to decline in physical function in people with knee OA, and further, whether these relationships are mediated by changes in pain. We applied machine learning (ML) approaches to gait data in MOST to identify markers of gait alterations in people with worsening physical function over 2 years, and tested mediation by pain.
Methods: MOST participants were age 45-90 with, or at risk for, knee OA. Gait was assessed using inertial measurement units (OPAL, APDM, Portland, OR) worn on the trunk and both ankles during a 20-meter walk test at a self-selected speed. Participants were categorized by the outcome, worsening physical function, defined as MCID increase in WOMAC physical function score (4+ points on 0-68 scale ) over 2-years.
We used an ensemble machine learning technique (“super learning”) with multiple algorithms (Figure 1 footnote) to optimally discriminate between those with and without the outcome. Variables included as possible predictors in the ML process included person-level gait variables , person-level OA status (# of knees with K-L grade >1), age, BMI, depressive symptoms (CES-D), and race. Data were randomly split into 70% training and 30% test sets; data split, model training and testing were repeated 100 times. We used a variable importance statistic to identify the 10 most influential variables that most frequently contributed to the prediction of worsening physical function. Log-binomial regression evaluated associations of these variables with MCID change in WOMAC function over 2 years. Continuous variables were standardized. As changes in function could be related to pain, we also tested for mediation by MCID change in WOMAC pain over 2 years.
Results: Of 2324 participants (mean age 63.6 [SD: 10.5] years, 57% female). 24% had worsening WOMAC function over 2 years by MCID change. Figure 1 lists top contributing variables from the ensemble ML process (AUC=0.60).
Lower cadence (Figure 2) was associated with worsening function over 2 years. Also associated with worsening function were depressive symptoms, older age, radiographic OA, and clinic site. MCID change in WOMAC pain mediated the association of cadence and worsening function over 2 years, accounting for approximately 34% of the total effect of cadence on worsening function.
Conclusion: Our results suggest lower cadence is associated with worsening physical function over 2 years in individuals with, or at risk for, knee OA, a minority of which is mediated by changes in pain. Further support comes from observations that in people with hip OA who receive a biomechanical intervention, improvements in cadence are related to improved WOMAC Function scores. Interventions that target cadence in people with knee OA may lead to improvements in physical function.
.jpg)
Disclosures: K. Bacon, None; D. Felson, None; S. Jafarzadeh, None; V. Kolachalama, None; J. Hausdorff, None; E. Gazit, None; J. Stefanik, None; P. Corrigan, None; N. Segal, Pacira Biosciences, Integra LifeSciences, Trice Medical; C. Lewis, None; M. Nevitt, None; D. Kumar, Pfizer, Eli Lilly.

