Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0102: Impact of Racial Implicit Bias on Juvenile Idiopathic Arthritis Patients' Treatment Recommendations
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AA
Alisha Akinsete, MD
Hospital for Special Surgery
Wayne, NJ, United States
Abstract Poster Presenter(s)
Alisha Akinsete1, Illir Agalliu2, Dawn Wahezi1, Ellen Silvers2, Onjona Hossain2, Irene Blanco2, Tamar Rubinstein3 and Cristina Gonzalez2, 1Children's Hospital at Montefiore, Bronx, NY, 2Albert Einstein College of Medicine, Bronx, NY, 3Albert Einstein College of Medicine, White Plains, NY
Background/Purpose: There are racial and ethnic disparities in juvenile idiopathic arthritis (JIA). Implicit bias can contribute to these health disparities through provider communication and medical decision-making. For example, studies have shown that racial implicit bias can affect pain management recommendations in pediatric patients. Early aggressive treatment with biologic treatment has been shown to be more effective than conventional DMARDs. In this study we described the implicit racial and racial/medical adherence biases of the international pediatric rheumatology community and investigated their associations with treatment recommendations and perception of compliance.
Methods: Our study recruited an international cohort of faculty, fellows, physician assistants and nurse practitioners practicing in pediatric rheumatology from Nov 2021 through Feb 2022. Demographic data was collected via an online survey, after which participants participated in two online timed modules, designed to determine the "inappropriate vs appropriate vs aggressive" treatment for the JIA patients based on the data provided. Patients differed by race (White vs Black). Participants were then asked to assess how adherent the patient would likely be with treatment. Following the vignettes, participants completed the adult race Implicit Assessment Test (IAT) and the adult race and medical compliance; an IATD-score was given. A positive IAT score indicates a pro-White bias and a negative a pro-Black bias, 0 is no bias. The IAT scores range from -2 to +2. The student T-test and one-way ANOVA were used to compare IAT scores between groups. Logistic regression models were used to examine the associations of the following variables(provider age, sex, race, job title, years of experience) to the participant IAT scores with regards to the outcome variable of interest: either appropriate or aggressive treatment within each vignette (white vs black).
Results: A total of 165 providers completed the survey, modules and IATs. The majority were women (64%), White (79%) and faculty (76%). Overall, providers showed a slight pro-White bias (mean IAT D score= 0.26, SD=0.51) and slight pro-White bias with medical compliance stereotype (mean IAT D score= 0.16, SD=0.43). There were no differences in appropriate or aggressive treatment recommendations associated with IAT scores for White or Black vignettes, although the results were based on small sample size. Interestingly, there was an inverse association between the IAT score where in the Black vignette the providers we less likely to give aggressive therapy as the pro-White bias increased (OR=0.54, 95% CI 0.20-1.46, p=0.23 per unit increase in IAT) whereas in the White vignette providers were more likely to give aggressive treatment as the pro-White bias (OR= 4.07 95% CI 0.75-22.24 p=0.11). Nonetheless, findings were not statistically significant.
Conclusion: : In this feasibility study, Implicit Bias was not associated with treatment recommendation or perceived compliance of JIA patients. Further larger studies are needed to better evaluate implicit bias's impact on provider communication.
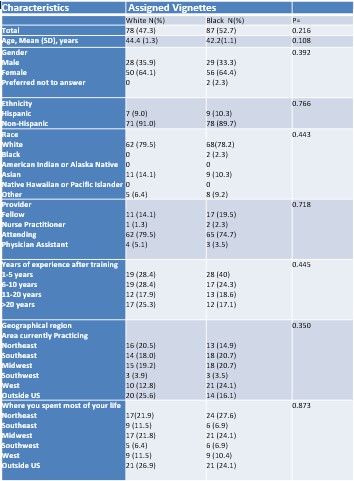 Provider Characteristics Assigned to Clinical Vignettes
Provider Characteristics Assigned to Clinical Vignettes
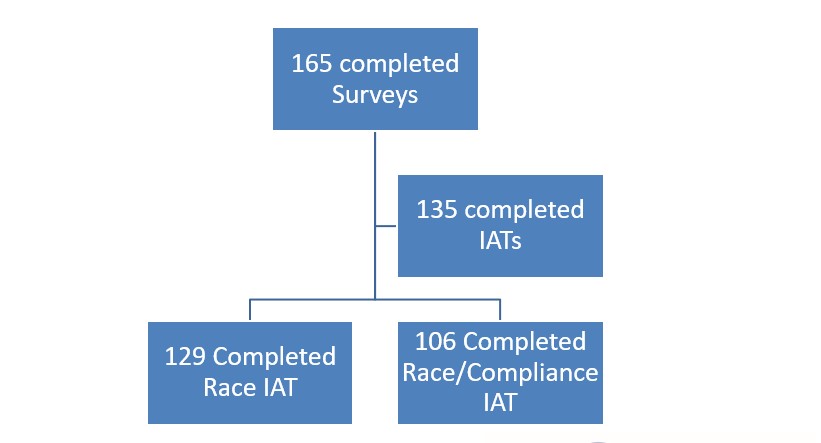 Providers Who Completed Implicit Association Tests
Providers Who Completed Implicit Association Tests
Disclosures: A. Akinsete, None; I. Agalliu, None; D. Wahezi, None; E. Silvers, None; O. Hossain, None; I. Blanco, Novartis; T. Rubinstein, None; C. Gonzalez, None.
Background/Purpose: There are racial and ethnic disparities in juvenile idiopathic arthritis (JIA). Implicit bias can contribute to these health disparities through provider communication and medical decision-making. For example, studies have shown that racial implicit bias can affect pain management recommendations in pediatric patients. Early aggressive treatment with biologic treatment has been shown to be more effective than conventional DMARDs. In this study we described the implicit racial and racial/medical adherence biases of the international pediatric rheumatology community and investigated their associations with treatment recommendations and perception of compliance.
Methods: Our study recruited an international cohort of faculty, fellows, physician assistants and nurse practitioners practicing in pediatric rheumatology from Nov 2021 through Feb 2022. Demographic data was collected via an online survey, after which participants participated in two online timed modules, designed to determine the "inappropriate vs appropriate vs aggressive" treatment for the JIA patients based on the data provided. Patients differed by race (White vs Black). Participants were then asked to assess how adherent the patient would likely be with treatment. Following the vignettes, participants completed the adult race Implicit Assessment Test (IAT) and the adult race and medical compliance; an IATD-score was given. A positive IAT score indicates a pro-White bias and a negative a pro-Black bias, 0 is no bias. The IAT scores range from -2 to +2. The student T-test and one-way ANOVA were used to compare IAT scores between groups. Logistic regression models were used to examine the associations of the following variables(provider age, sex, race, job title, years of experience) to the participant IAT scores with regards to the outcome variable of interest: either appropriate or aggressive treatment within each vignette (white vs black).
Results: A total of 165 providers completed the survey, modules and IATs. The majority were women (64%), White (79%) and faculty (76%). Overall, providers showed a slight pro-White bias (mean IAT D score= 0.26, SD=0.51) and slight pro-White bias with medical compliance stereotype (mean IAT D score= 0.16, SD=0.43). There were no differences in appropriate or aggressive treatment recommendations associated with IAT scores for White or Black vignettes, although the results were based on small sample size. Interestingly, there was an inverse association between the IAT score where in the Black vignette the providers we less likely to give aggressive therapy as the pro-White bias increased (OR=0.54, 95% CI 0.20-1.46, p=0.23 per unit increase in IAT) whereas in the White vignette providers were more likely to give aggressive treatment as the pro-White bias (OR= 4.07 95% CI 0.75-22.24 p=0.11). Nonetheless, findings were not statistically significant.
Conclusion: : In this feasibility study, Implicit Bias was not associated with treatment recommendation or perceived compliance of JIA patients. Further larger studies are needed to better evaluate implicit bias's impact on provider communication.
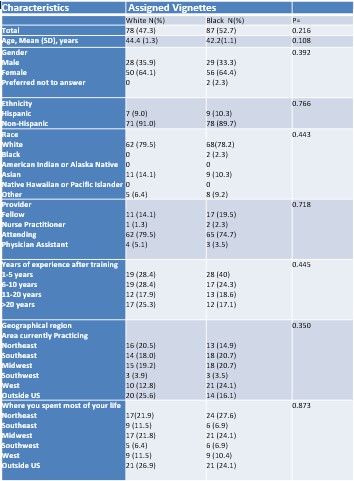 Provider Characteristics Assigned to Clinical Vignettes
Provider Characteristics Assigned to Clinical Vignettes 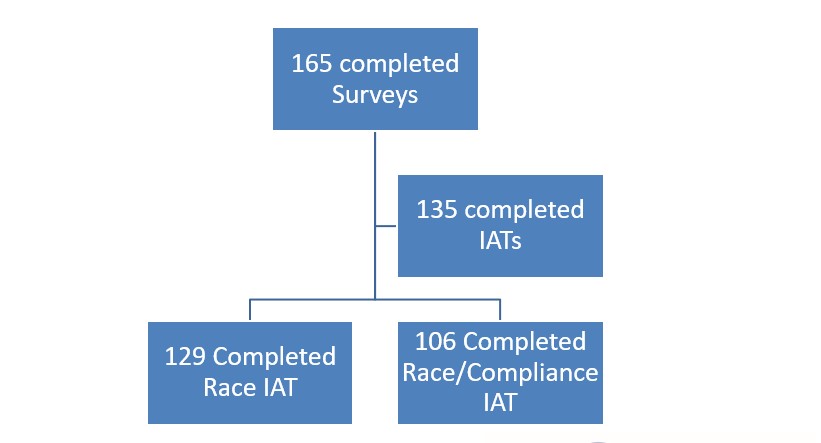 Providers Who Completed Implicit Association Tests
Providers Who Completed Implicit Association TestsDisclosures: A. Akinsete, None; I. Agalliu, None; D. Wahezi, None; E. Silvers, None; O. Hossain, None; I. Blanco, Novartis; T. Rubinstein, None; C. Gonzalez, None.

