Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0160: Sarcopenia in Myositis Patients: A Marker of Muscle Damage Associated with Myositis Severity and Disability
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MG
Margherita Giannini, MD
Nouvel Hopital Civil, Strasbourg
Strasbourg, France
Abstract Poster Presenter(s)
Margherita Giannini1, Léa Debrut2, Anne-Laure Charles2, Mégane Pizzimenti2, Rose-Marie Javier3, Bernard Geny4 and Alain Meyer1, 1Service de Physiologie et explorations fonctionnelles, CHU, Strasbourg ; Centre de Référence des Maladies Autoimmunes Rares, CHU, Strasbourg ; UR3072, Centre de Recherche en Biomédecine, University of Strasbourg, Strasbourg, France, 2UR3072 Centre de Recherche en Biomédecine, University of Strasbourg, Strasbourg, France, 3Service de Rhumatologie, Centre de Référence des Maladies Autoimmunes Rares, University Hospital of Strasbourg, Strasbourg, France, 4Service de Physiologie et explorations fonctionnelles, CHU, Strasbourg ; UR3072 Centre de Recherche en Biomédecine, University of Strasbourg, Strasbourg, France
Background/Purpose: Myositis are autoimmune diseases characterized by muscle inflammation and weakness. Even when disease is no longer active, a great proportion of patients does not recover physical performance and residual muscle weakness persists.
Sarcopenia is a progressive and generalized skeletal muscle disorder characterized by low muscle strength and mass leading to disability, decreased quality of life and increased mortality. It has been reported in various autoimmune diseases, but it has never been studied in myositis.
The aim of this study was to investigate prevalence and significance of sarcopenia in myositis patients with low or no disease activity.
Methods: Adult myositis patients according to 2017 ACR/EULAR classification criteria, with disease duration greater than 12 months, stable medication for 6 months, creatine kinase serum level (CK) less than 500 U/l were enrolled. 30 healthy sex and age-matched controls were also included.
At the enrolment, total (LM) and appendicular lean mass (ALM) were measured using dual-energy X-ray absorptiometry (DXA) and grip strength using dynamometer. Sarcopenia was defined according to the European Working Group on Sarcopenia in Older People 2 consensus. Disease activity and damage according to International myositis assessment and Clinical Studies Group (IMACS). Muscle strength was measured by manual muscle test (MMT-8; MMT-12) and hand-held dynamometer, physical performance by 6-minute walking test (6mWT) and disability by Health Assessment Questionnaire (HAQ).
Results: 34 patients were prospectively enrolled. They suffered from DM (n= 5), necrotizing autoimmune myopathy (NAIM, n=10), anti-synthetase syndrome (ASS, n=11), scleromyositis (SM, n=8) since 4.9 years (3.0-8.6). 7 patients (20.6%) were sarcopenic (vs 0% in controls) (figure 1).
At the enrolment, sarcopenic patients were globally weaker; they had a lower physical performance and a greater disability. Both extent and severity of damage score according to the IMACS were significantly higher in sarcopenic patients (figure 2). LM and ALM negatively correlated with the IMACS damage scores, and positively with the physical performance parameters and with grip strength (figure 3).
Sarcopenic patients generally suffered from NAIM. Consistently, they had higher maximum CK levels. Moreover, 50% of sarcopenic patients had myocarditis. By contrast, extramuscular involvements were less frequent and none of sarcopenic patients had inflammatory joint involvement during the follow-up (figure 1).
In a multivariate analysis, myositis subtypes and myocarditis were independently associated with sarcopenia (respectively p=0.04 and p=0.001).
Interestingly, sarcopenic patients required more frequently aggressive therapy as intravenous immunoglobulins (83.3% vs 33.3%, p=0.03), plasmapheresis (33.3% vs 3.7%, p=0.02) and/or janus kinase inhibitors (16.7% vs 0 (0%), p=0.03).
Conclusion: Prevalence of sarcopenia in myositis with inactive or low activity disease is more than 20%. Sarcopenic patients are a subgroup with severe muscle disease, important damage and disability. Muscle mass measured by DXA is a quantitative tool to rapidly assess muscle damage in myositis.
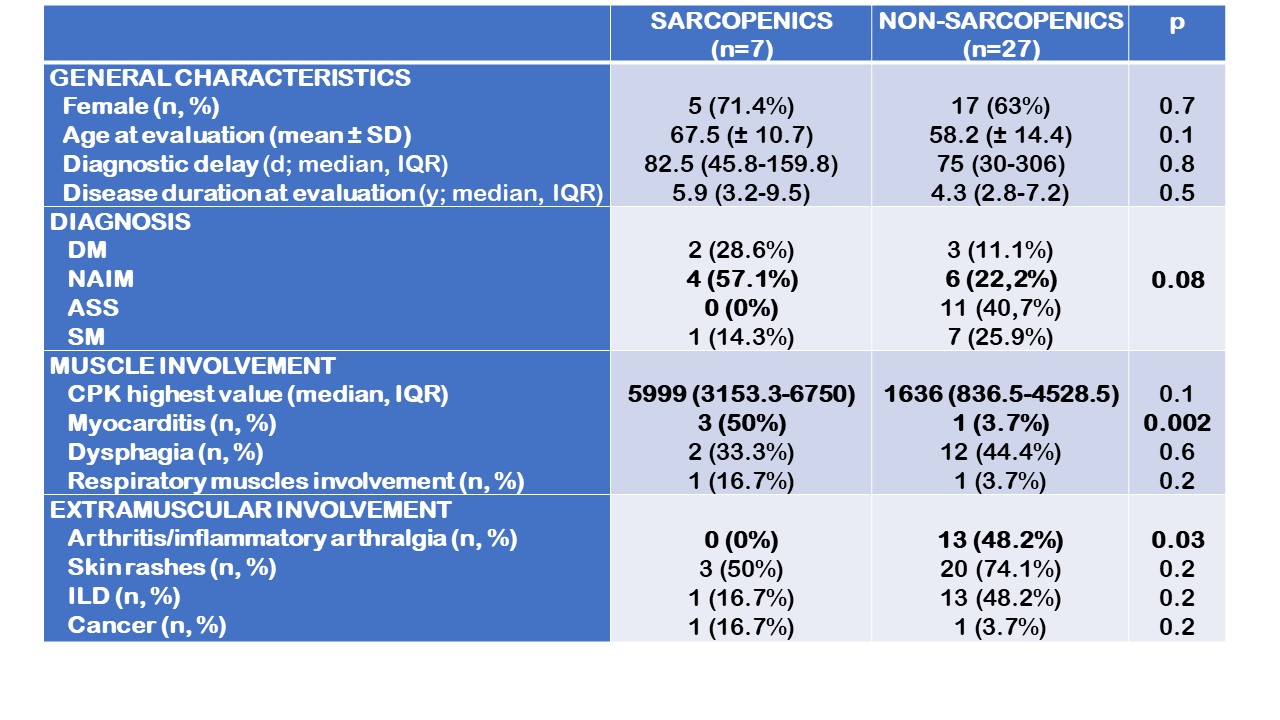 Figure 1. Demographic and clinical data on myositis cohort with low or no disease activity. Categorical data were expressed as percentages, normally distributed continuous variables as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. ASS: anti-synthetase syndrome. CPK: creatine phosphokinase. DM: dermatomyositis. ILD: interstitial lung disease. NAIM: necrotizing autoimmune myopathy. SM: scleromyositis.
Figure 1. Demographic and clinical data on myositis cohort with low or no disease activity. Categorical data were expressed as percentages, normally distributed continuous variables as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. ASS: anti-synthetase syndrome. CPK: creatine phosphokinase. DM: dermatomyositis. ILD: interstitial lung disease. NAIM: necrotizing autoimmune myopathy. SM: scleromyositis.
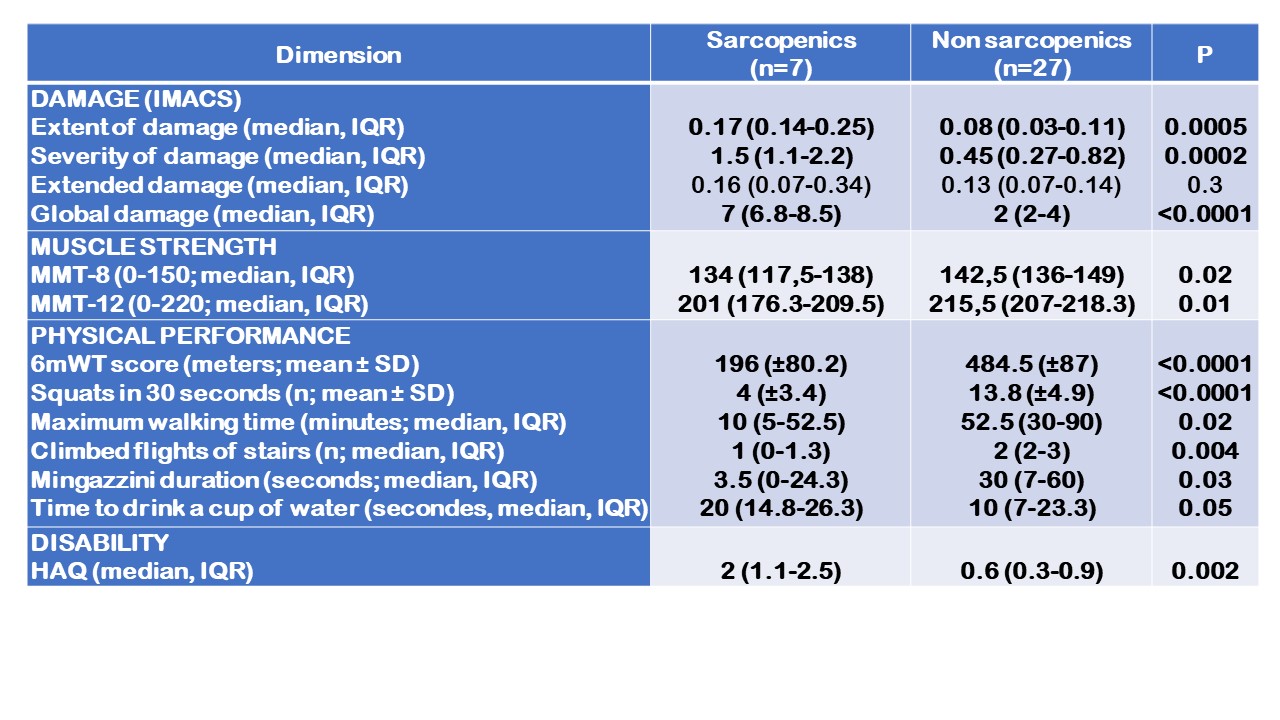 Figure 2. Parameters assessed at inclusion. Normally distributed continuous variables were expressed as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. HAQ: health assessment questionnaire. IMACS: International Myositis Assessment and Clinical Studies Group. IQR: interquartile range. MMT: manual muscle test. 6mWT: 6-minute walking test.
Figure 2. Parameters assessed at inclusion. Normally distributed continuous variables were expressed as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. HAQ: health assessment questionnaire. IMACS: International Myositis Assessment and Clinical Studies Group. IQR: interquartile range. MMT: manual muscle test. 6mWT: 6-minute walking test.
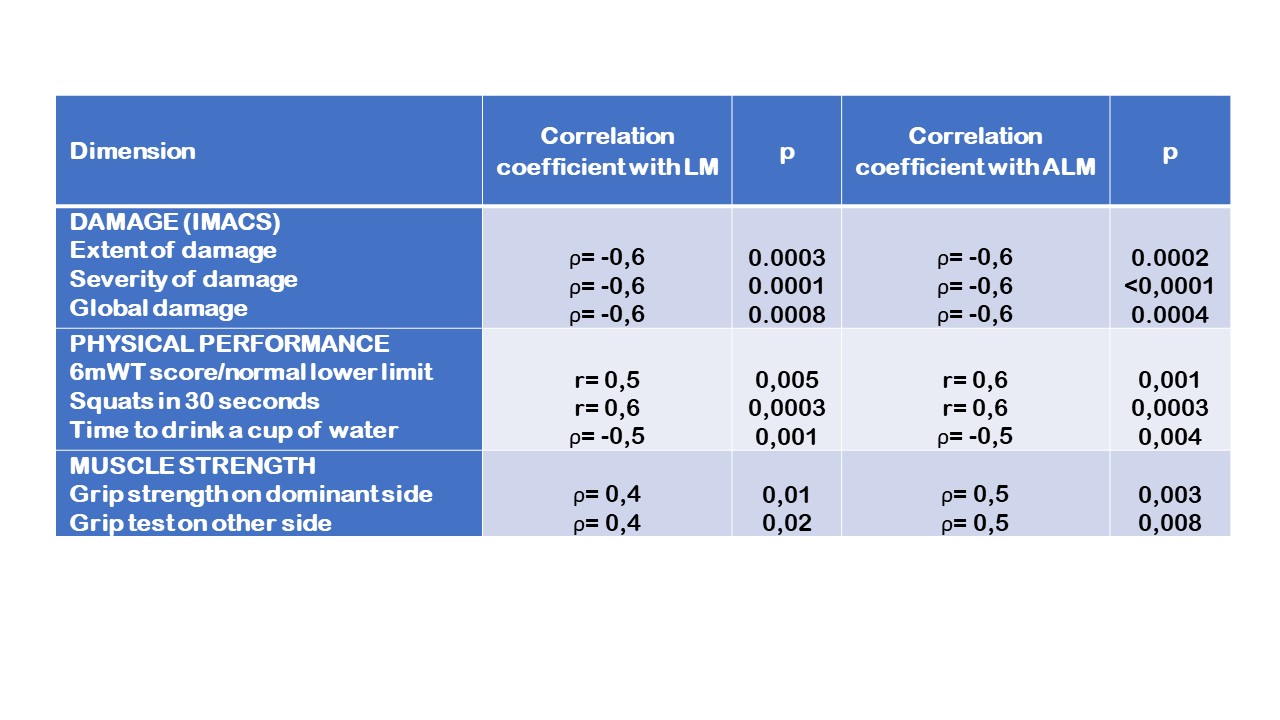 Figure 3. Correlations between total (LM) and appendicular lean mass (ALM) and physical parameters.
Figure 3. Correlations between total (LM) and appendicular lean mass (ALM) and physical parameters.
IMACS: International Myositis Assessment and Clinical Studies Group. 6mWT: 6-minute walking test.
Disclosures: M. Giannini, None; L. Debrut, None; A. Charles, None; M. Pizzimenti, None; R. Javier, None; B. Geny, None; A. Meyer, None.
Background/Purpose: Myositis are autoimmune diseases characterized by muscle inflammation and weakness. Even when disease is no longer active, a great proportion of patients does not recover physical performance and residual muscle weakness persists.
Sarcopenia is a progressive and generalized skeletal muscle disorder characterized by low muscle strength and mass leading to disability, decreased quality of life and increased mortality. It has been reported in various autoimmune diseases, but it has never been studied in myositis.
The aim of this study was to investigate prevalence and significance of sarcopenia in myositis patients with low or no disease activity.
Methods: Adult myositis patients according to 2017 ACR/EULAR classification criteria, with disease duration greater than 12 months, stable medication for 6 months, creatine kinase serum level (CK) less than 500 U/l were enrolled. 30 healthy sex and age-matched controls were also included.
At the enrolment, total (LM) and appendicular lean mass (ALM) were measured using dual-energy X-ray absorptiometry (DXA) and grip strength using dynamometer. Sarcopenia was defined according to the European Working Group on Sarcopenia in Older People 2 consensus. Disease activity and damage according to International myositis assessment and Clinical Studies Group (IMACS). Muscle strength was measured by manual muscle test (MMT-8; MMT-12) and hand-held dynamometer, physical performance by 6-minute walking test (6mWT) and disability by Health Assessment Questionnaire (HAQ).
Results: 34 patients were prospectively enrolled. They suffered from DM (n= 5), necrotizing autoimmune myopathy (NAIM, n=10), anti-synthetase syndrome (ASS, n=11), scleromyositis (SM, n=8) since 4.9 years (3.0-8.6). 7 patients (20.6%) were sarcopenic (vs 0% in controls) (figure 1).
At the enrolment, sarcopenic patients were globally weaker; they had a lower physical performance and a greater disability. Both extent and severity of damage score according to the IMACS were significantly higher in sarcopenic patients (figure 2). LM and ALM negatively correlated with the IMACS damage scores, and positively with the physical performance parameters and with grip strength (figure 3).
Sarcopenic patients generally suffered from NAIM. Consistently, they had higher maximum CK levels. Moreover, 50% of sarcopenic patients had myocarditis. By contrast, extramuscular involvements were less frequent and none of sarcopenic patients had inflammatory joint involvement during the follow-up (figure 1).
In a multivariate analysis, myositis subtypes and myocarditis were independently associated with sarcopenia (respectively p=0.04 and p=0.001).
Interestingly, sarcopenic patients required more frequently aggressive therapy as intravenous immunoglobulins (83.3% vs 33.3%, p=0.03), plasmapheresis (33.3% vs 3.7%, p=0.02) and/or janus kinase inhibitors (16.7% vs 0 (0%), p=0.03).
Conclusion: Prevalence of sarcopenia in myositis with inactive or low activity disease is more than 20%. Sarcopenic patients are a subgroup with severe muscle disease, important damage and disability. Muscle mass measured by DXA is a quantitative tool to rapidly assess muscle damage in myositis.
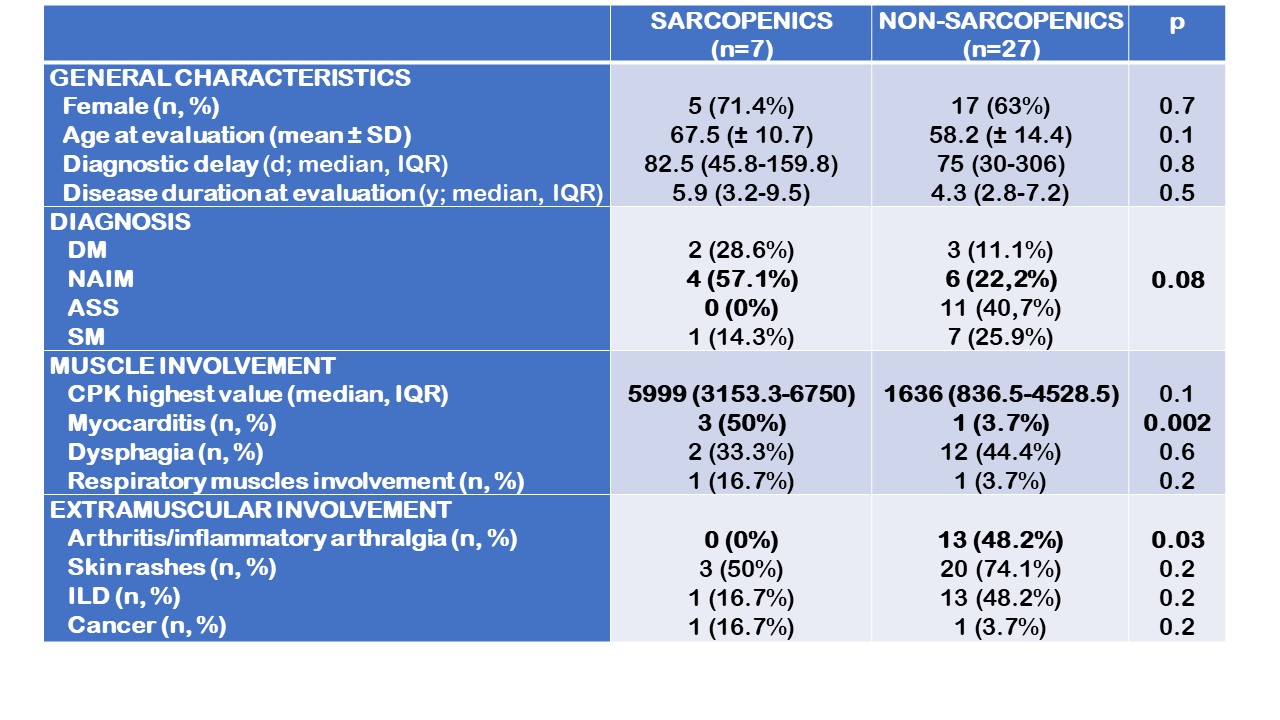 Figure 1. Demographic and clinical data on myositis cohort with low or no disease activity. Categorical data were expressed as percentages, normally distributed continuous variables as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. ASS: anti-synthetase syndrome. CPK: creatine phosphokinase. DM: dermatomyositis. ILD: interstitial lung disease. NAIM: necrotizing autoimmune myopathy. SM: scleromyositis.
Figure 1. Demographic and clinical data on myositis cohort with low or no disease activity. Categorical data were expressed as percentages, normally distributed continuous variables as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. ASS: anti-synthetase syndrome. CPK: creatine phosphokinase. DM: dermatomyositis. ILD: interstitial lung disease. NAIM: necrotizing autoimmune myopathy. SM: scleromyositis. 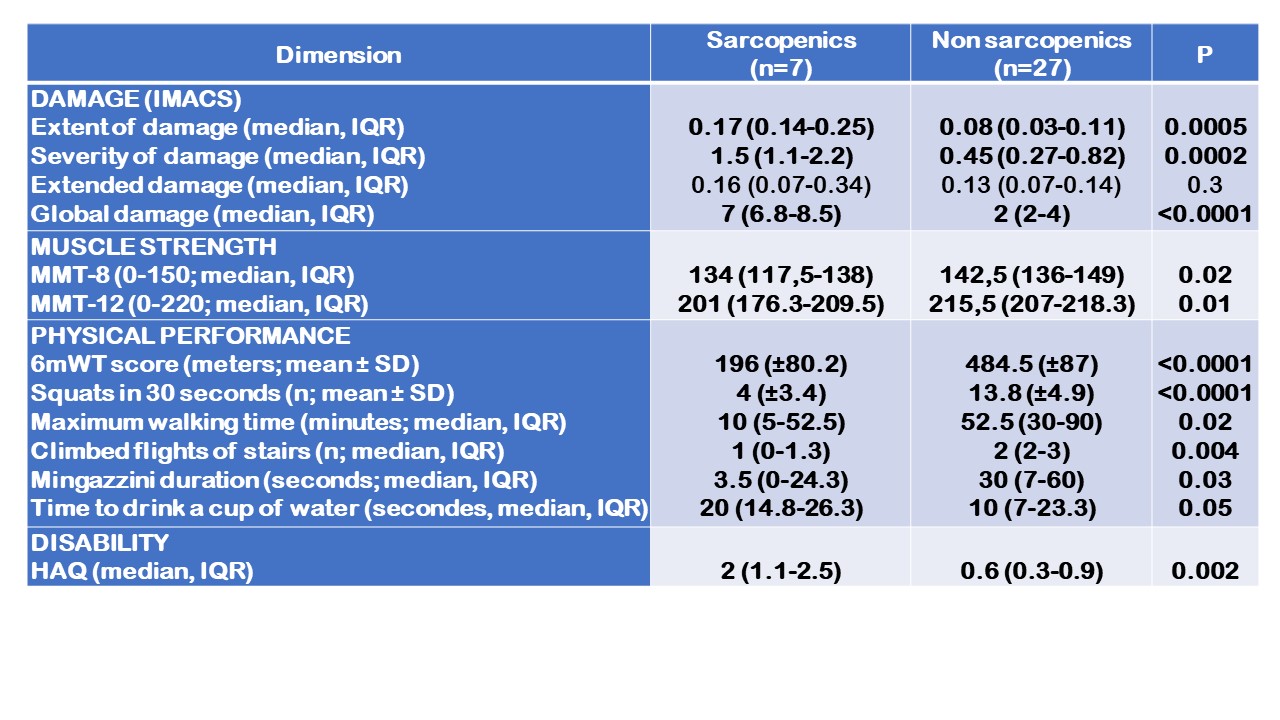 Figure 2. Parameters assessed at inclusion. Normally distributed continuous variables were expressed as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. HAQ: health assessment questionnaire. IMACS: International Myositis Assessment and Clinical Studies Group. IQR: interquartile range. MMT: manual muscle test. 6mWT: 6-minute walking test.
Figure 2. Parameters assessed at inclusion. Normally distributed continuous variables were expressed as mean (± standard deviation), non-normally distributed continuous variables as median and interquartile range. HAQ: health assessment questionnaire. IMACS: International Myositis Assessment and Clinical Studies Group. IQR: interquartile range. MMT: manual muscle test. 6mWT: 6-minute walking test. 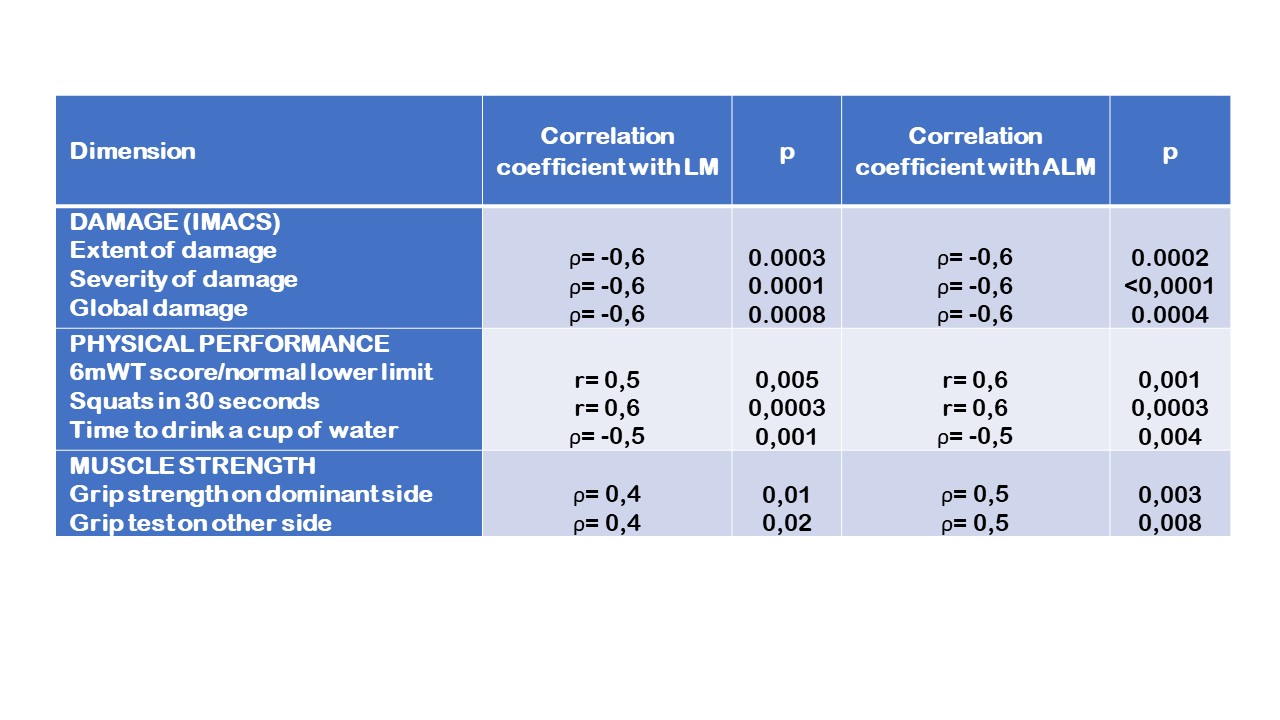 Figure 3. Correlations between total (LM) and appendicular lean mass (ALM) and physical parameters.
Figure 3. Correlations between total (LM) and appendicular lean mass (ALM) and physical parameters.IMACS: International Myositis Assessment and Clinical Studies Group. 6mWT: 6-minute walking test.
Disclosures: M. Giannini, None; L. Debrut, None; A. Charles, None; M. Pizzimenti, None; R. Javier, None; B. Geny, None; A. Meyer, None.

