Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0164: Anti-SSa/SSb and Ro52 Status and Pulmonary Function Tests in Patients with Interstitial Lung Disease and Idiopathic Inflammatory Myopathies
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SN
Sonali Narain, MD, MPH
Northwell Health
Great Neck, NY, United States
Abstract Poster Presenter(s)
Abdullah Ahmed1, Sonali Narain2, Ivana Ilic1, Can Hu3, Jaspreet Bhatti4 and Galina Marder5, 1Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Manhasset, NY, 2Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Great Neck, NY, 3Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Fort Lee, NJ, 4Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New York, NY, 5Donald and Barbara Zucker School of Medicine at Hofstra/ Northwell, Great Neck, NY
Background/Purpose: Interstitial lung disease (ILD) is a major cause of morbidity and mortality in patients with idiopathic inflammatory myositis (IIM). Anti-SSa/SSb and Ro52 are frequently reported in myositis. We have previously reported an association between presence of SSa/SSb antibodies and interstitial lung disease (ILD). The aim of this analysis was to evaluate the prognostic utility of anti-SSa/SSb and Ro52 in predicting severity and progression of ILD in IIM patients.
Methods: This is a follow up analysis of the Northwell Myositis cohort incepted 1/1/2007- 4/6/2018 ensuing through 6/1/2022. All patients met 2017 EULAR/ACR classification criteria for IIM and had anti-SSa/SSb serologies available. Anti-SSb was only found in association with anti-SSa in this cohort and was analyzed as a single group.Diagnosis of ILD was defined by presence of NSIP, COP/BOOP, UIP, and unspecified patterns on CT chest and confirmed by chart review. PFTs were analyzed at baseline and longitudinally over a 48-month period. Descriptive statistics, ANOVA and repeated measures ANOVA (non-parametric) were used for statistical analysis.
Results: Of 94 patients in the cohort, 36.2% (34/94) had a diagnosis of ILD, 22 patients had at least 2 PFTs and were included in follow-up analysis.
45.5% (10/22) patients were anti-SSa/SSb positive, of which, 27.3% (6/22) were double positive, 54.5% (12/22) patients were negative for anti-SSa/SSb and anti-Ro52. Demographics, clinical characteristics, and medications are presented in Table 1.
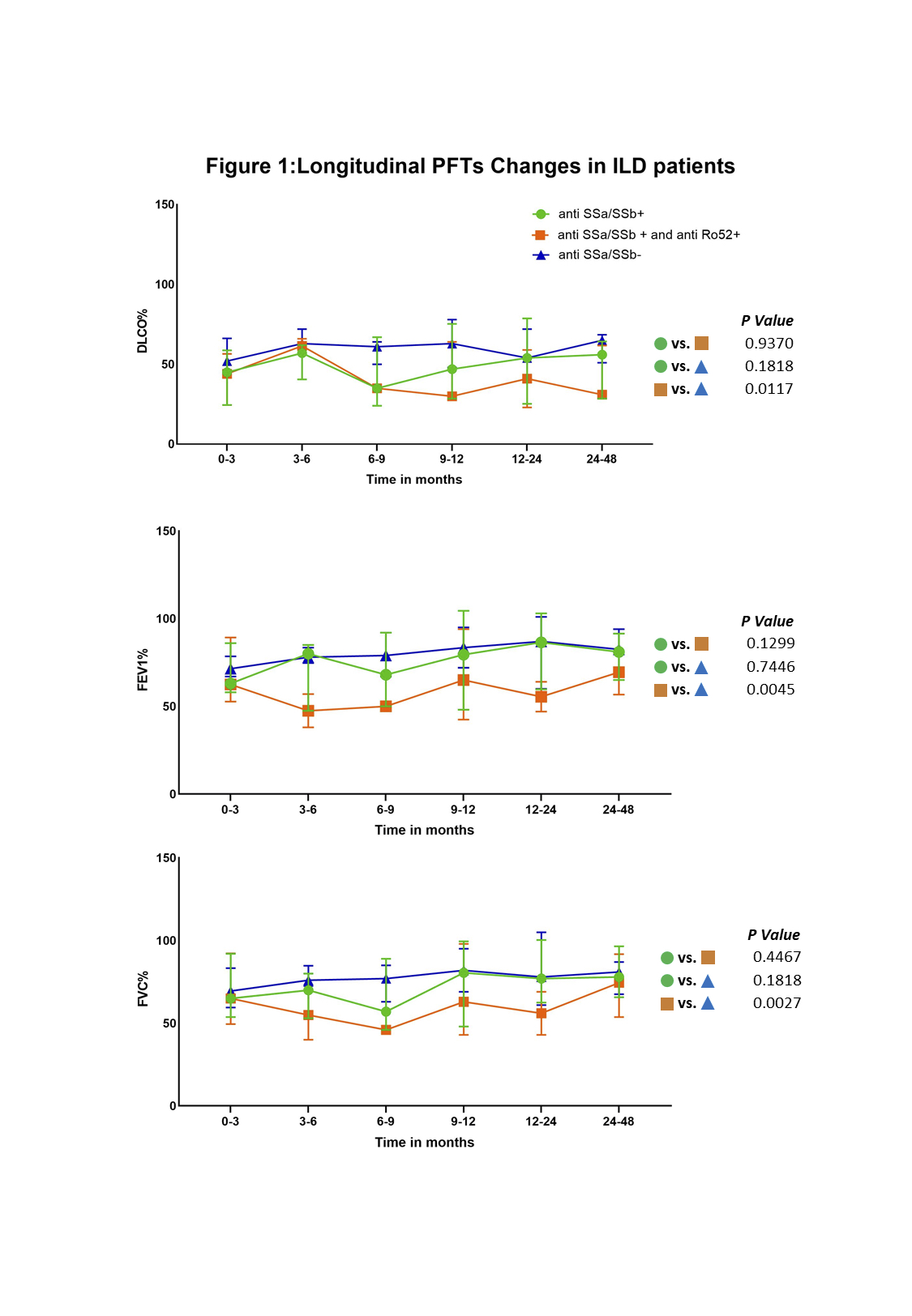
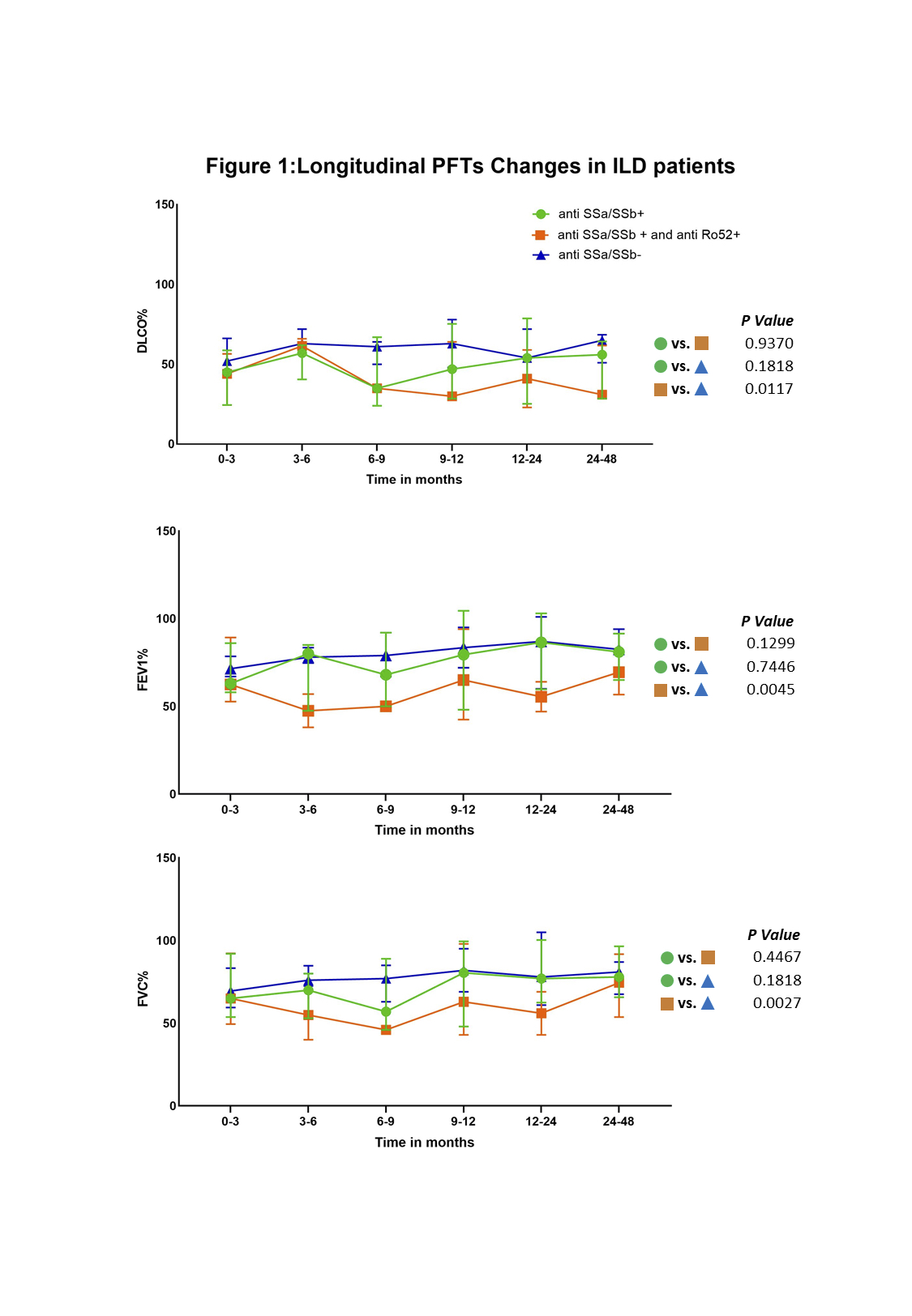
PFT parameters (FVC, FEV1 and DLCO) were similar across all 3 groups at the time of inception as shown in Table 2. During the 48-month follow-up, FVC, FEV1 and DLCO remained stable over time in the anti-SSa/SSB negative group (n=39). While there were fluctuations in the FVC, FEV1 and DLCO in both anti-SSa/SSb positive (n=37) and the double positive groups (n=19), a statistically significant decline was observed in the double positive group when compared to the anti-SSa negative group (FVC, p = 0.0117; FEV1, p = 0.0045; and DLCO p = 0.0027). This difference was not observed between the anti-SSa/SSB positive and the double positive groups nor between the anti-SSa/SSb positive and negative groups. PFT change time over time in each group is shown on Figure 1.
Conclusion: In patients with diagnosis of ILD, the presence or absence of anti-SSa/SSb and anti-Ro52 did not affect baseline PFT parameters. IIM associated ILD patients, irrespective of anti-SSA/SSB positivity, tend to maintain their pulmonary function over time. However, patients who are anti-Ro52 positive are more likely to decline despite aggressive therapy. This further supports that presence of Ro52 antibodies is a negative prognostic marker for ILD in patients with IIM.
.jpg)
.jpg)
Disclosures: A. Ahmed, None; S. Narain, None; I. Ilic, None; C. Hu, None; J. Bhatti, None; G. Marder, None.
Background/Purpose: Interstitial lung disease (ILD) is a major cause of morbidity and mortality in patients with idiopathic inflammatory myositis (IIM). Anti-SSa/SSb and Ro52 are frequently reported in myositis. We have previously reported an association between presence of SSa/SSb antibodies and interstitial lung disease (ILD). The aim of this analysis was to evaluate the prognostic utility of anti-SSa/SSb and Ro52 in predicting severity and progression of ILD in IIM patients.
Methods: This is a follow up analysis of the Northwell Myositis cohort incepted 1/1/2007- 4/6/2018 ensuing through 6/1/2022. All patients met 2017 EULAR/ACR classification criteria for IIM and had anti-SSa/SSb serologies available. Anti-SSb was only found in association with anti-SSa in this cohort and was analyzed as a single group.Diagnosis of ILD was defined by presence of NSIP, COP/BOOP, UIP, and unspecified patterns on CT chest and confirmed by chart review. PFTs were analyzed at baseline and longitudinally over a 48-month period. Descriptive statistics, ANOVA and repeated measures ANOVA (non-parametric) were used for statistical analysis.
Results: Of 94 patients in the cohort, 36.2% (34/94) had a diagnosis of ILD, 22 patients had at least 2 PFTs and were included in follow-up analysis.
45.5% (10/22) patients were anti-SSa/SSb positive, of which, 27.3% (6/22) were double positive, 54.5% (12/22) patients were negative for anti-SSa/SSb and anti-Ro52. Demographics, clinical characteristics, and medications are presented in Table 1.
PFT parameters (FVC, FEV1 and DLCO) were similar across all 3 groups at the time of inception as shown in Table 2. During the 48-month follow-up, FVC, FEV1 and DLCO remained stable over time in the anti-SSa/SSB negative group (n=39). While there were fluctuations in the FVC, FEV1 and DLCO in both anti-SSa/SSb positive (n=37) and the double positive groups (n=19), a statistically significant decline was observed in the double positive group when compared to the anti-SSa negative group (FVC, p = 0.0117; FEV1, p = 0.0045; and DLCO p = 0.0027). This difference was not observed between the anti-SSa/SSB positive and the double positive groups nor between the anti-SSa/SSb positive and negative groups. PFT change time over time in each group is shown on Figure 1.
Conclusion: In patients with diagnosis of ILD, the presence or absence of anti-SSa/SSb and anti-Ro52 did not affect baseline PFT parameters. IIM associated ILD patients, irrespective of anti-SSA/SSB positivity, tend to maintain their pulmonary function over time. However, patients who are anti-Ro52 positive are more likely to decline despite aggressive therapy. This further supports that presence of Ro52 antibodies is a negative prognostic marker for ILD in patients with IIM.
.jpg)
.jpg)
Disclosures: A. Ahmed, None; S. Narain, None; I. Ilic, None; C. Hu, None; J. Bhatti, None; G. Marder, None.

