Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0117: Disparities in Prescription Medications Among Myositis Patients in a Large Urban Medical Center
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DA
Diala Alawneh, MD
University of Illinois at Chicago
Chicago, IL, United States
Abstract Poster Presenter(s)
Diala Alawneh1, Zita Chan1, William Galanter2, John Berry3, Mina Al-Awqati4 and Huan Chang5, 1University of Illinois at Chicago, Chicago, IL, 2University of Chicago, Chicago, IL, 3University of Illinois Hospital & Health Sciences System, Chicago, IL, 4University of Illinois, Chicago, IL, 5University of Illinois at Chicago and Jesse Brown VA Medical Center, Chicago, IL
Background/Purpose: Although women are twice as likely as men to develop myositis, Black women are affected disproportionately. Additionally, minorities with juvenile dermatomyositis are significantly more likely to have low family income and significantly worse scores on physical function, disease activity and quality of life. This pilot study investigates the relationship between race/ethnicity, sex, living in a disadvantaged neighborhood, and the frequency of being prescribed a DMARD (biologic or conventional) or a steroid in myositis patients. The objective of this study is to demonstrate a relationship between race/ethnicity, sex, living in a disadvantaged neighborhood, and the frequency of being prescribed disease-specific treatment for myositis in patients seen in the rheumatology clinic.
Methods: Data from the electronic health record (EHR) of a large urban hospital were analyzed from January 1, 2010 through August 31, 2020. Independent variables included age, race/ethnicity, sex, and address with zip code. The area deprivation index (ADI) score was calculated using the neighborhood atlas website mapping tool. Rheumatologic medications were the dependent variables. Prescribed steroids, DMARDs, and cyclophosphamide were compared between socioeconomic and racial/ethnic groups. Prescription of non-steroidal medications was also compared. Regression analysis was used to predict steroid use as a function of age, race/ethnicity, sex, and ADI. The analysis was repeated for DMARD and cyclophosphamide use.
Results: There were 158 unique patients with myositis. Of these, 118 (74.7%) were women and 40 (25.3%) were men. Race/ethnicity was 17 (10.8%) non-Hispanic Whites, 94 (59.5%) non-Hispanic Blacks, 34 (21.5%) Latinx, and 13 (8.2%) Other. Women were more likely to receive cyclophosphamide, mycophenolate, or rituximab than men. Men were more likely to receive etanercept than women. ADI scores were higher among Black and Latinx patients compared with White patients (p < 0.00001). There was no difference between steroid (p=0.41) or cyclophosphamide (p=0.93) use between minority and white patients. White patients were 22.6% as likely to receive a DMARD as Black patients (p< 0.016). Latinx patients were as likely to receive a DMARD as Black patients. Results showed that physician prescribing pattern does not vary with area deprivation index scores.
Conclusion: Among patients with myositis, Blacks and Latinx are more likely to live in an area with a higher area deprivation index score. There was no difference between minorities and Whites of being prescribed a steroid or cyclophosphamide; White patients were less likely to receive a DMARD than Black patients. Physician prescribing pattern did not vary with area deprivation scores. Future studies with larger sample sizes are needed to help quantify the relationship between area deprivation score, race/ethnicity, and sex; to better understand physician prescribing patterns in patients, particularly among minority groups; and to understand how these factors may influence disease-related health outcomes in myositis.
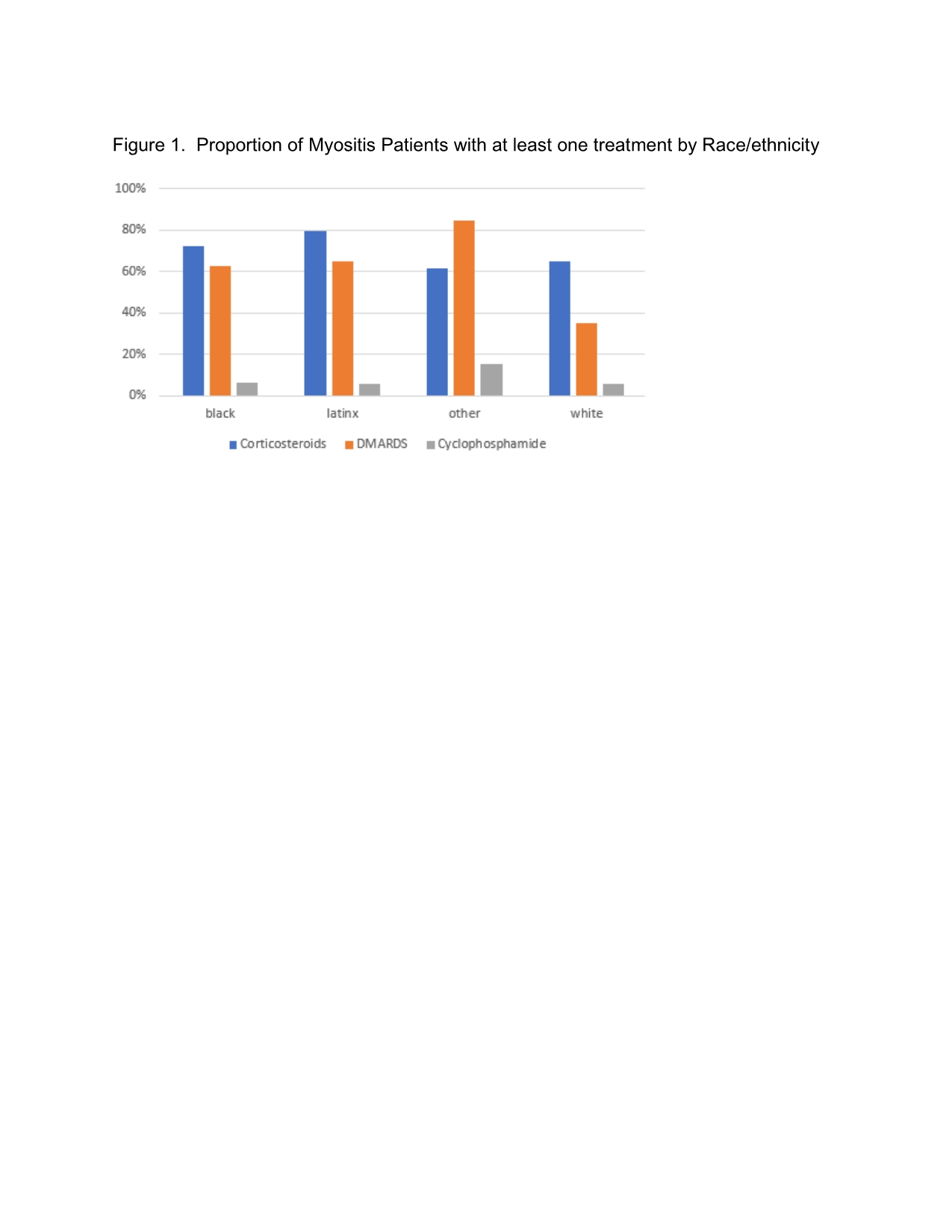 Figure 1. Proportion of Myositis Patients with at least one treatment by Race/Ethnicity
Figure 1. Proportion of Myositis Patients with at least one treatment by Race/Ethnicity
 Figure 2. Proportion of Myositis Patients with at least one treatment by Area Deprivation Index Score Quantile
Figure 2. Proportion of Myositis Patients with at least one treatment by Area Deprivation Index Score Quantile
Disclosures: D. Alawneh, None; Z. Chan, None; W. Galanter, None; J. Berry, None; M. Al-Awqati, None; H. Chang, None.
Background/Purpose: Although women are twice as likely as men to develop myositis, Black women are affected disproportionately. Additionally, minorities with juvenile dermatomyositis are significantly more likely to have low family income and significantly worse scores on physical function, disease activity and quality of life. This pilot study investigates the relationship between race/ethnicity, sex, living in a disadvantaged neighborhood, and the frequency of being prescribed a DMARD (biologic or conventional) or a steroid in myositis patients. The objective of this study is to demonstrate a relationship between race/ethnicity, sex, living in a disadvantaged neighborhood, and the frequency of being prescribed disease-specific treatment for myositis in patients seen in the rheumatology clinic.
Methods: Data from the electronic health record (EHR) of a large urban hospital were analyzed from January 1, 2010 through August 31, 2020. Independent variables included age, race/ethnicity, sex, and address with zip code. The area deprivation index (ADI) score was calculated using the neighborhood atlas website mapping tool. Rheumatologic medications were the dependent variables. Prescribed steroids, DMARDs, and cyclophosphamide were compared between socioeconomic and racial/ethnic groups. Prescription of non-steroidal medications was also compared. Regression analysis was used to predict steroid use as a function of age, race/ethnicity, sex, and ADI. The analysis was repeated for DMARD and cyclophosphamide use.
Results: There were 158 unique patients with myositis. Of these, 118 (74.7%) were women and 40 (25.3%) were men. Race/ethnicity was 17 (10.8%) non-Hispanic Whites, 94 (59.5%) non-Hispanic Blacks, 34 (21.5%) Latinx, and 13 (8.2%) Other. Women were more likely to receive cyclophosphamide, mycophenolate, or rituximab than men. Men were more likely to receive etanercept than women. ADI scores were higher among Black and Latinx patients compared with White patients (p < 0.00001). There was no difference between steroid (p=0.41) or cyclophosphamide (p=0.93) use between minority and white patients. White patients were 22.6% as likely to receive a DMARD as Black patients (p< 0.016). Latinx patients were as likely to receive a DMARD as Black patients. Results showed that physician prescribing pattern does not vary with area deprivation index scores.
Conclusion: Among patients with myositis, Blacks and Latinx are more likely to live in an area with a higher area deprivation index score. There was no difference between minorities and Whites of being prescribed a steroid or cyclophosphamide; White patients were less likely to receive a DMARD than Black patients. Physician prescribing pattern did not vary with area deprivation scores. Future studies with larger sample sizes are needed to help quantify the relationship between area deprivation score, race/ethnicity, and sex; to better understand physician prescribing patterns in patients, particularly among minority groups; and to understand how these factors may influence disease-related health outcomes in myositis.
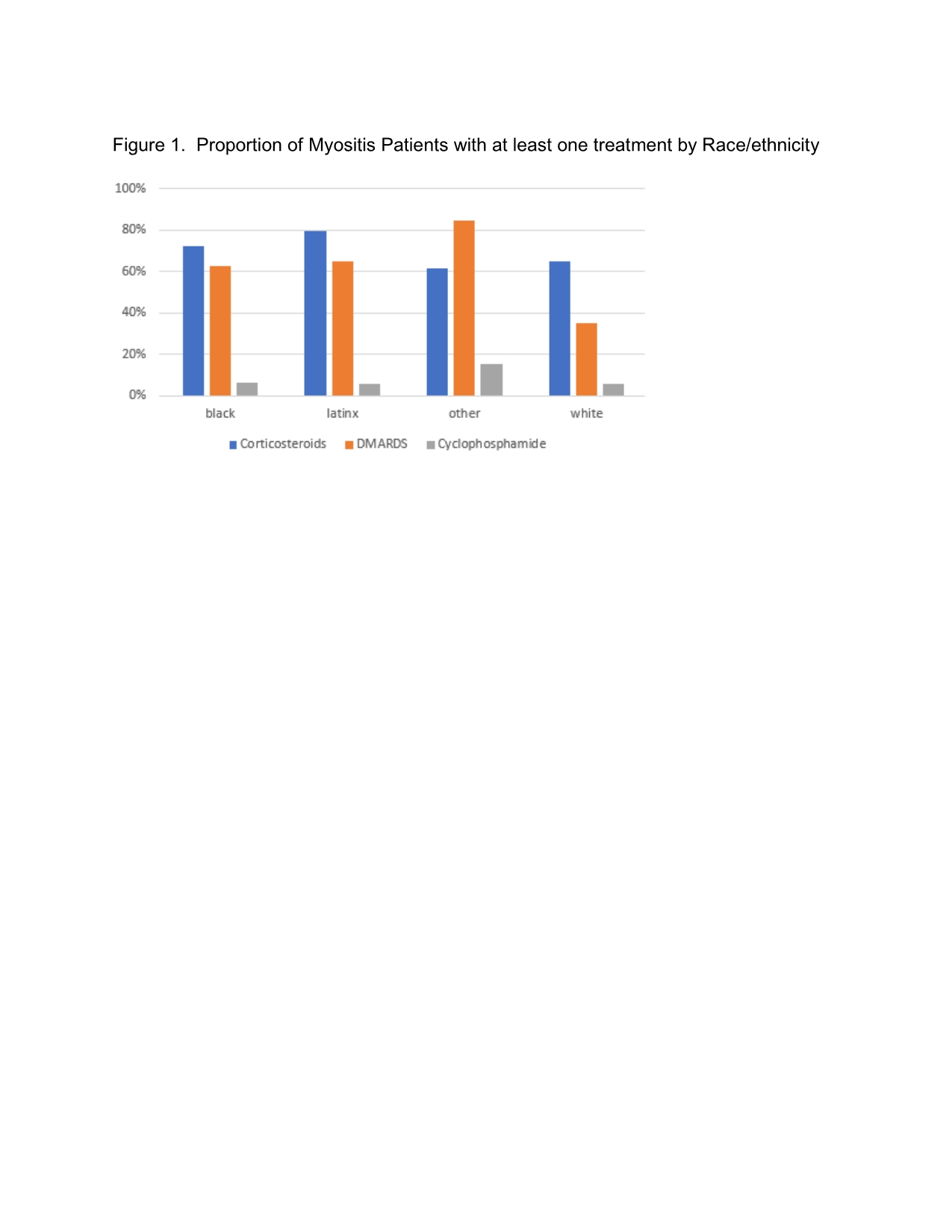 Figure 1. Proportion of Myositis Patients with at least one treatment by Race/Ethnicity
Figure 1. Proportion of Myositis Patients with at least one treatment by Race/Ethnicity Figure 2. Proportion of Myositis Patients with at least one treatment by Area Deprivation Index Score Quantile
Figure 2. Proportion of Myositis Patients with at least one treatment by Area Deprivation Index Score QuantileDisclosures: D. Alawneh, None; Z. Chan, None; W. Galanter, None; J. Berry, None; M. Al-Awqati, None; H. Chang, None.

