Back
Poster Session A
Epidemiology, health policy and outcomes
Session: (0187–0213) Patient Outcomes, Preferences, and Attitudes Poster I
0206: Differences in Medicinal Cannabis Use According to Demography, Rationale, and Patient-Physician Interactions Between the United States and Canada
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
.png)
Mary-Ann Fitzcharles, MD, FRCPC
McGill University
Montreal-West, QC, Canada
Abstract Poster Presenter(s)
kevin boehnke1, Ying He1, Tristin Smith1, marc martel2, david williams1 and Mary-Ann Fitzcharles3, 1University of Michigan, Ann Arbor, MI, 2McGill University, Montréal-Ouest, Canada, 3McGill University, Montréal, QC, Canada
Background/Purpose: Medical cannabis (MC) is increasingly used by persons with rheumatic conditions worldwide, although legal status varies by country. In Canada, MC has been federally available for over 2 decades, while 37 states in the United States (US) legalized MC since 1996. Similarly, recreational cannabis was federally legalized in Canada in 2018, whereas recreational use is currently legalized in 19 states in the US but remains federally illegal. In this study, we sought to understand whether and how these legal differences affected rationale for MC use and patient-physician interactions around MC between individuals residing in the US and Canada.
Methods: Partnering with the Arthritis Foundation (US) and the Arthritis Society (Canada), we surveyed persons self-reporting a rheumatic condition about MC use. Our final sample included n=459 participants in the US and n=347 in Canada. Excluded were those under 18, residing in a country outside US or Canada, not fluent in English or French, without a rheumatic condition, and failing to provide consent, or completion of the survey. We used R (version 4.1.1) for statistical analyses. Differences between subgroups were assessed using Pearsons' Chi-square tests with Yates' continuity correction for categorical variables and two sample t-tests for continuous variables.
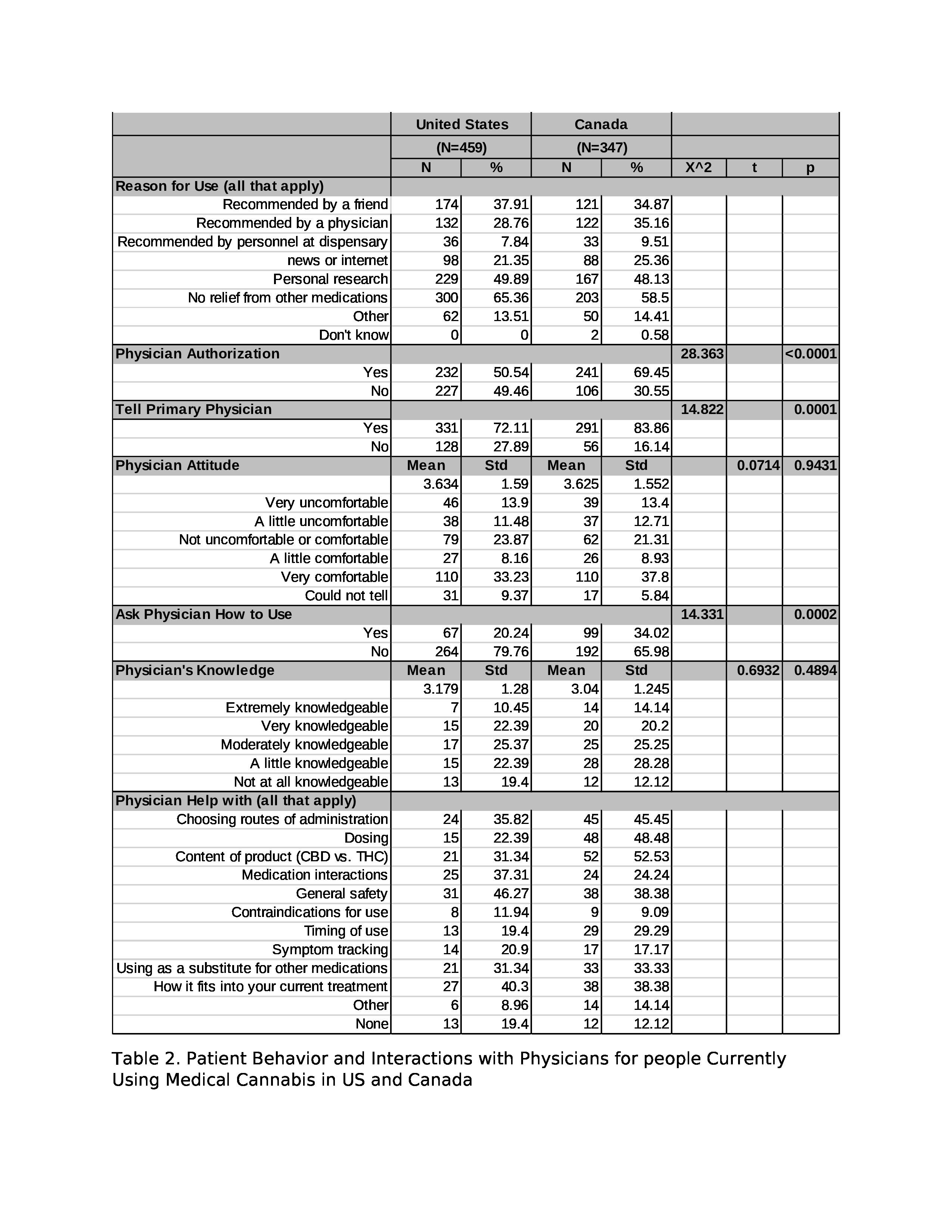
Results: Compared to those in Canada, participants in the US were younger (55.5 vs. 63.6, p< 0.0001) and a higher proportion were female (89.5% vs. 77.5%, p < 0.0001) (Table 1). The distribution of race, educational level, employment status, tobacco use, and alcohol use were significantly different between countries (p's < 0.05). Participants generally initiated cannabis use due to inadequate relief from medications or personal research. Compared to Canadian participants, a lower proportion of US participants obtained a MC license, initiated use due to physician recommendation, disclosed MC use to their physician, and asked for advice on how to use cannabis (all p's < 0.001). Among participants who disclosed MC use to their physician, there were no significant differences between countries in perceptions of physician comfort or knowledge around MC (p's >0.05). However, Canadian participants generally received more physician help on optimizing MC use (e.g., routes of administration (45% vs 35%), dosing (48.5% vs 22.4%), content of products (52.5% vs 31.3%), while US participants asked more questions about general safety (46.3% vs. 38.4%) and medication interactions (37.3% vs. 24.2%).
Conclusion: There are considerable differences between the US and Canada regarding the demographics of rheumatology patients using MC. Canadian patients report a greater dialogue with their physicians regarding MC use, although there were no differences in perceptions of physician knowledge or comfort with cannabis between countries. Our results suggest that MC legality may lower stigma and barriers to patient-physician communication about MC use.
.jpg) Table1. Demographic Characteristics of US and Canada Patients Currently using Medical Cannabis
Table1. Demographic Characteristics of US and Canada Patients Currently using Medical Cannabis
Disclosures: k. boehnke, Tryp therapeutics; Y. He, None; T. Smith, None; m. martel, Sant cannabis; d. williams, Swing therapeutics; M. Fitzcharles, None.
Background/Purpose: Medical cannabis (MC) is increasingly used by persons with rheumatic conditions worldwide, although legal status varies by country. In Canada, MC has been federally available for over 2 decades, while 37 states in the United States (US) legalized MC since 1996. Similarly, recreational cannabis was federally legalized in Canada in 2018, whereas recreational use is currently legalized in 19 states in the US but remains federally illegal. In this study, we sought to understand whether and how these legal differences affected rationale for MC use and patient-physician interactions around MC between individuals residing in the US and Canada.
Methods: Partnering with the Arthritis Foundation (US) and the Arthritis Society (Canada), we surveyed persons self-reporting a rheumatic condition about MC use. Our final sample included n=459 participants in the US and n=347 in Canada. Excluded were those under 18, residing in a country outside US or Canada, not fluent in English or French, without a rheumatic condition, and failing to provide consent, or completion of the survey. We used R (version 4.1.1) for statistical analyses. Differences between subgroups were assessed using Pearsons' Chi-square tests with Yates' continuity correction for categorical variables and two sample t-tests for continuous variables.
Results: Compared to those in Canada, participants in the US were younger (55.5 vs. 63.6, p< 0.0001) and a higher proportion were female (89.5% vs. 77.5%, p < 0.0001) (Table 1). The distribution of race, educational level, employment status, tobacco use, and alcohol use were significantly different between countries (p's < 0.05). Participants generally initiated cannabis use due to inadequate relief from medications or personal research. Compared to Canadian participants, a lower proportion of US participants obtained a MC license, initiated use due to physician recommendation, disclosed MC use to their physician, and asked for advice on how to use cannabis (all p's < 0.001). Among participants who disclosed MC use to their physician, there were no significant differences between countries in perceptions of physician comfort or knowledge around MC (p's >0.05). However, Canadian participants generally received more physician help on optimizing MC use (e.g., routes of administration (45% vs 35%), dosing (48.5% vs 22.4%), content of products (52.5% vs 31.3%), while US participants asked more questions about general safety (46.3% vs. 38.4%) and medication interactions (37.3% vs. 24.2%).
Conclusion: There are considerable differences between the US and Canada regarding the demographics of rheumatology patients using MC. Canadian patients report a greater dialogue with their physicians regarding MC use, although there were no differences in perceptions of physician knowledge or comfort with cannabis between countries. Our results suggest that MC legality may lower stigma and barriers to patient-physician communication about MC use.
.jpg) Table1. Demographic Characteristics of US and Canada Patients Currently using Medical Cannabis
Table1. Demographic Characteristics of US and Canada Patients Currently using Medical Cannabis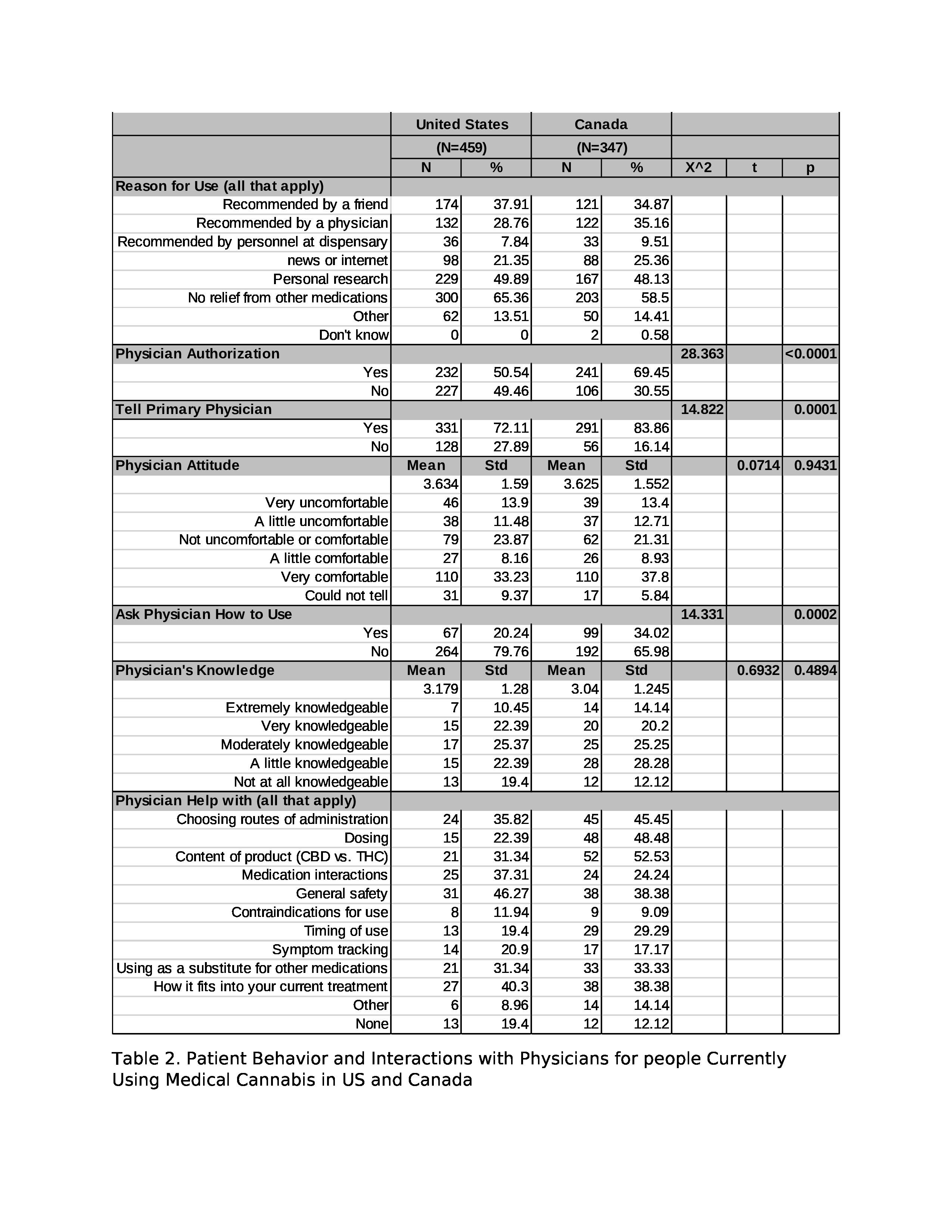
Disclosures: k. boehnke, Tryp therapeutics; Y. He, None; T. Smith, None; m. martel, Sant cannabis; d. williams, Swing therapeutics; M. Fitzcharles, None.

