Back
Poster Session A
Epidemiology, health policy and outcomes
Session: (0187–0213) Patient Outcomes, Preferences, and Attitudes Poster I
0195: Acceptance of Virtual Reality for Managing Their Disease Among People with Rheumatologic Conditions with and Without Prior Experience Using Virtual Reality
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Jeffrey Curtis, MD, MS, MPH
University of Alabama at Birmingham
Hoover, AL, United States
Abstract Poster Presenter(s)
Jeffrey Curtis1, Kimberly Garza2, Cassie Clinton3, Heqin Yang2, Alexicia Richardson2, Cheryl Seals2, Gary Hawkins2, Chad Rose2, William Benjamin Nowell4, Kelly Gavigan5 and Liana Fraenkel6, 1Division of Clinical Immunology & Rheumatology, University of Alabama at Birmingham, Birmingham, AL, 2Auburn University, Auburn, AL, 3University of Alabama at Birmingham, Hoover, AL, 4Global Healthy Living Foundation, Nyack, NY, 5Global Healthy Living Foundation, Upper Nyack, NY, 6Berkshire Medical Center, Lenox, MA
Background/Purpose: We aimed to assess enthusiasm for the use of virtual reality (VR) for clinical and educational use among people with rheumatologic diseases, comparing those with prior experience using VR to those with no prior experience.
Methods: A cross-sectional, online survey was conducted among adults with rheumatologic conditions who are members of ArthritisPower, an online patient-powered research network (registry). The Technology Acceptance Model was used as a conceptual framework, proposing perceived usefulness of, attitudes toward, and intention to use technology as factors that affect user acceptance. Survey items included prior experience with VR, perceived usefulness and potential enjoyment of using VR, and willingness to use VR to learn how rheumatologic conditions affect the body and what daily life might be like in more advanced stages of disease. Descriptive statistics and Pearson's chi square were used to compare perceived usefulness, enjoyment, and willingness to use VR in people with and without prior VR experience.
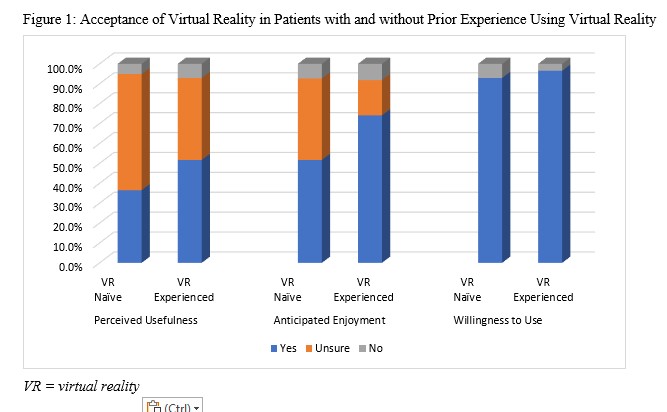
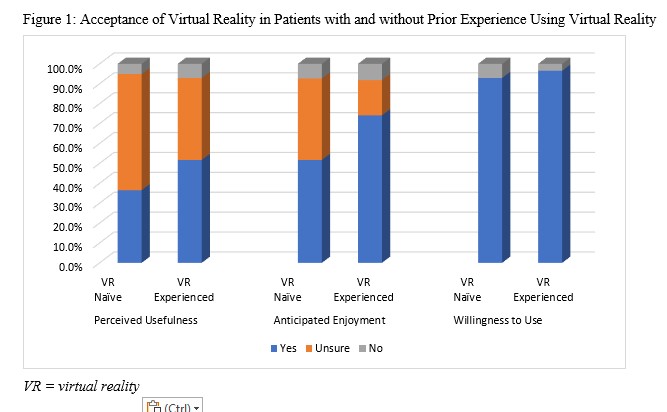
Results: A total of 523 individuals completed the survey. Mean age was 59.4 (SD=11.1) years. Most were female (86.6%) and White (88.3%). The most commonly reported conditions were rheumatoid arthritis (59.7%) and osteoarthritis (53.9%), and the majority (52.4%) had been diagnosed in the last 10 years. Frequencies of perceptions are shown in Table 1. Few participants reported having prior experience using VR (16.3%). Of these, the majority thought they could learn useful information about their condition using VR. A small percentage did not think it would be useful. In contrast, about one-third of respondents who had never used VR thought it would be useful, while the majority were unsure. Three-fourths of respondents who had prior experience using VR reported that they thought they would enjoy using it for this purpose, while only half of the respondents with no prior experience using VR thought they might enjoy using it. Nearly all respondents expressed willingness to use VR to manage their disease, regardless of prior experience using VR. The most commonly endorsed uses of VR included for exercise (77.8%), for physical therapy (73.8%), and for education (61.8%).
Conclusion: Even among people with no prior experience with virtual reality, people with rheumatologic conditions are enthusiastic about using VR to manage their disease state, particularly those with prior experience using VR. Interventions that introduce VR to this patient population for use in learning about and managing their disease are likely to be accepted.
Disclosures: J. Curtis, Amgen, Bristol-Myers Squibb (BMS), CorEvitas, IlluminationHealth, Janssen, Lilly, Myriad, Novartis, Pfizer, Sanofi, UCB, Aqtual, Bendcare, FASTER, GlaxoSmithKlein (GSK), Labcorp, Scipher, Setpoint, United Rheumatology, AbbVie, ArthritisPower; K. Garza, None; C. Clinton, None; H. Yang, None; A. Richardson, None; C. Seals, None; G. Hawkins, None; C. Rose, None; W. Nowell, Global Healthy Living Foundation, AbbVie Inc., Amgen, Eli Lilly; K. Gavigan, None; L. Fraenkel, None.
Background/Purpose: We aimed to assess enthusiasm for the use of virtual reality (VR) for clinical and educational use among people with rheumatologic diseases, comparing those with prior experience using VR to those with no prior experience.
Methods: A cross-sectional, online survey was conducted among adults with rheumatologic conditions who are members of ArthritisPower, an online patient-powered research network (registry). The Technology Acceptance Model was used as a conceptual framework, proposing perceived usefulness of, attitudes toward, and intention to use technology as factors that affect user acceptance. Survey items included prior experience with VR, perceived usefulness and potential enjoyment of using VR, and willingness to use VR to learn how rheumatologic conditions affect the body and what daily life might be like in more advanced stages of disease. Descriptive statistics and Pearson's chi square were used to compare perceived usefulness, enjoyment, and willingness to use VR in people with and without prior VR experience.
Results: A total of 523 individuals completed the survey. Mean age was 59.4 (SD=11.1) years. Most were female (86.6%) and White (88.3%). The most commonly reported conditions were rheumatoid arthritis (59.7%) and osteoarthritis (53.9%), and the majority (52.4%) had been diagnosed in the last 10 years. Frequencies of perceptions are shown in Table 1. Few participants reported having prior experience using VR (16.3%). Of these, the majority thought they could learn useful information about their condition using VR. A small percentage did not think it would be useful. In contrast, about one-third of respondents who had never used VR thought it would be useful, while the majority were unsure. Three-fourths of respondents who had prior experience using VR reported that they thought they would enjoy using it for this purpose, while only half of the respondents with no prior experience using VR thought they might enjoy using it. Nearly all respondents expressed willingness to use VR to manage their disease, regardless of prior experience using VR. The most commonly endorsed uses of VR included for exercise (77.8%), for physical therapy (73.8%), and for education (61.8%).
Conclusion: Even among people with no prior experience with virtual reality, people with rheumatologic conditions are enthusiastic about using VR to manage their disease state, particularly those with prior experience using VR. Interventions that introduce VR to this patient population for use in learning about and managing their disease are likely to be accepted.
Disclosures: J. Curtis, Amgen, Bristol-Myers Squibb (BMS), CorEvitas, IlluminationHealth, Janssen, Lilly, Myriad, Novartis, Pfizer, Sanofi, UCB, Aqtual, Bendcare, FASTER, GlaxoSmithKlein (GSK), Labcorp, Scipher, Setpoint, United Rheumatology, AbbVie, ArthritisPower; K. Garza, None; C. Clinton, None; H. Yang, None; A. Richardson, None; C. Seals, None; G. Hawkins, None; C. Rose, None; W. Nowell, Global Healthy Living Foundation, AbbVie Inc., Amgen, Eli Lilly; K. Gavigan, None; L. Fraenkel, None.

