Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0172: Clinical Characteristics and Outcomes of Inflammatory Myositis Related Interstitial Lung Disease: A 15 Year Retrospective Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EP
Elizabeth Pepper, DO
Dwight D Eisenhower Army Medical Center
Martinez, GA, United States
Abstract Poster Presenter(s)
Ian Ward1, Elizabeth Pepper2 and Geoffrey Loh2, 1United States Army, Evans, GA, 2DDEAMC, Ft. Gordon, GA
Background/Purpose: Interstitial lung disease (ILD) is a common complication of Idiopathic Inflammatory Myopathy (IIM). This extra-muscular manifestation is a significant source of morbidity and has been described as a marker of more severe disease and increased mortality in patients with IIM. Our study aims to describe the frequency, associated clinical characteristics, and outcomes of ILD in IIM receiving care through the military healthcare system.
Methods: We performed an IRB approved, retrospective review of inflammatory myositis diagnosed within the Department of Defense (DoD) from January 2006 to December 2020. Patients were identified by ICD-10 diagnosis codes for inflammatory myositis and included if diagnosed at one of fifteen facilities within the DoD. All patients met the Bohan and Peter 1975 or EULAR/ACR classification criteria for definite or probable myositis. Inflammatory myopathies were categorized into IIM, IIM with ILD (IIM-ILD), Anti-Synthetase Syndrome (IIM-ILD, ASyS), and IIM-ILD, non-ASyS. Demographic, laboratory, pulmonary function test, imaging and biopsy data were identified at initial presentation. Pulmonary function testing, imaging and treatments were collected during the follow up period. Clinical outcomes were based on the last documentation by the evaluating physician. Data points were compared between IIM and IIM-ILD cohorts with subgroup analysis of ASyS and ILD-IIM, non-ASyS. Student’s t-tests for continuous variables and Chi square tests for categorical variables were performed. Odds ratios were calculated for statistically significant variables.
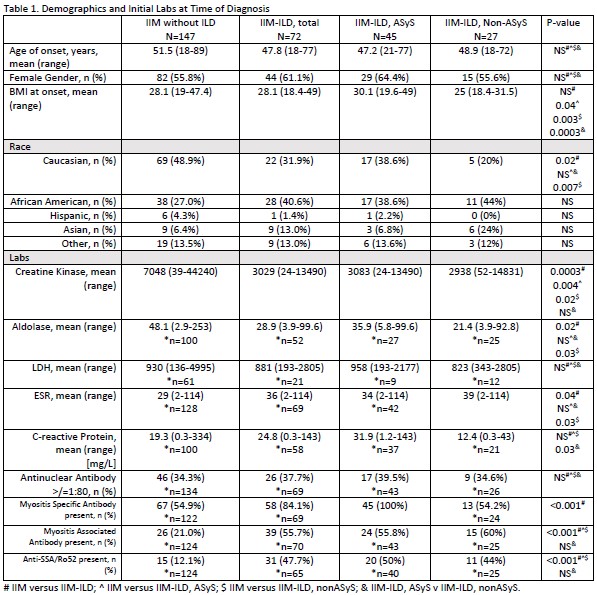
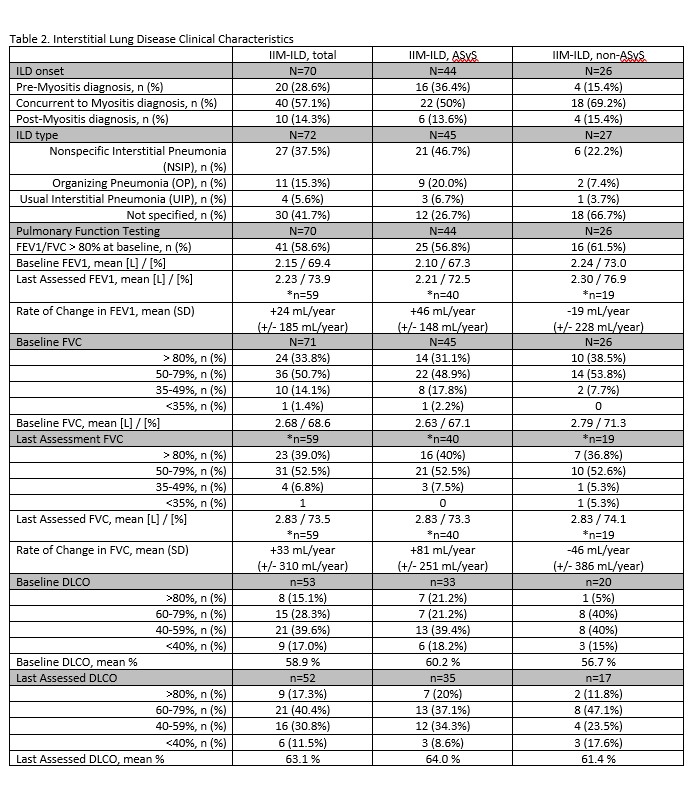
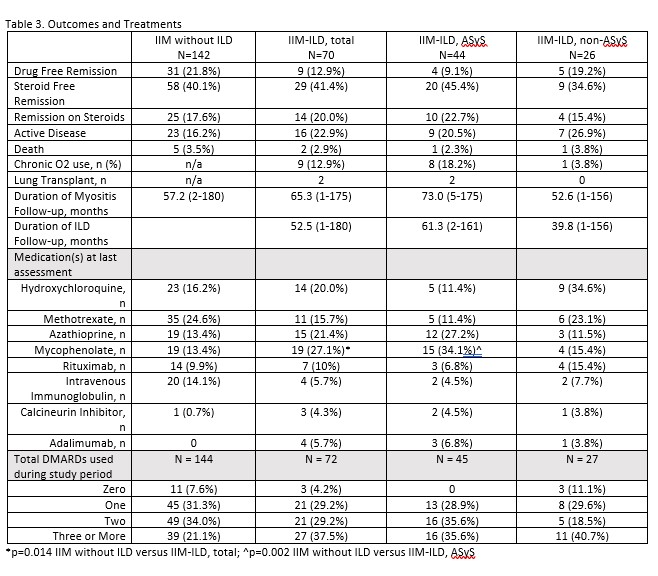
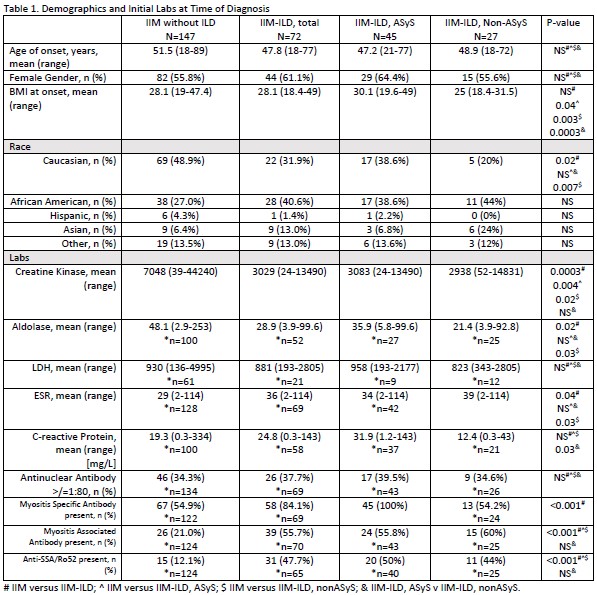
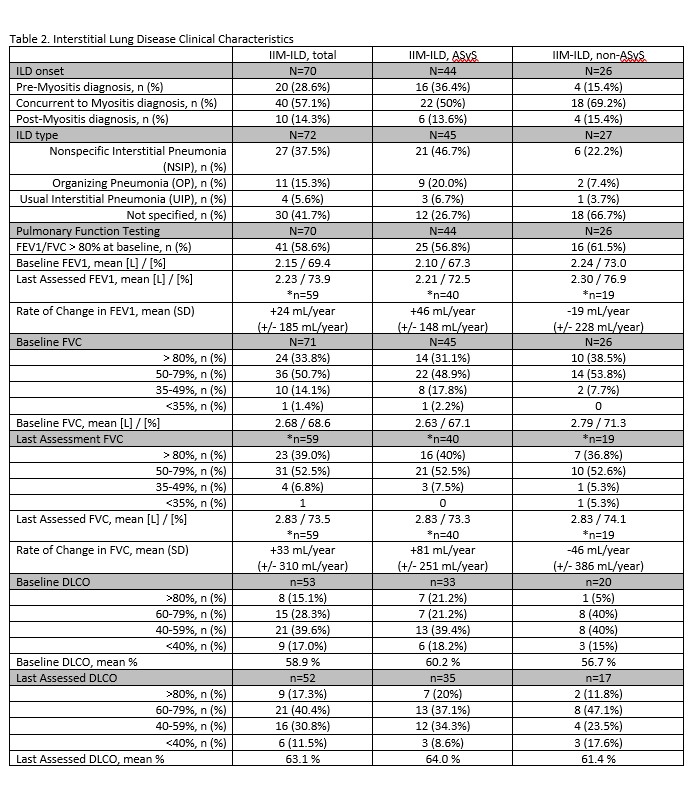
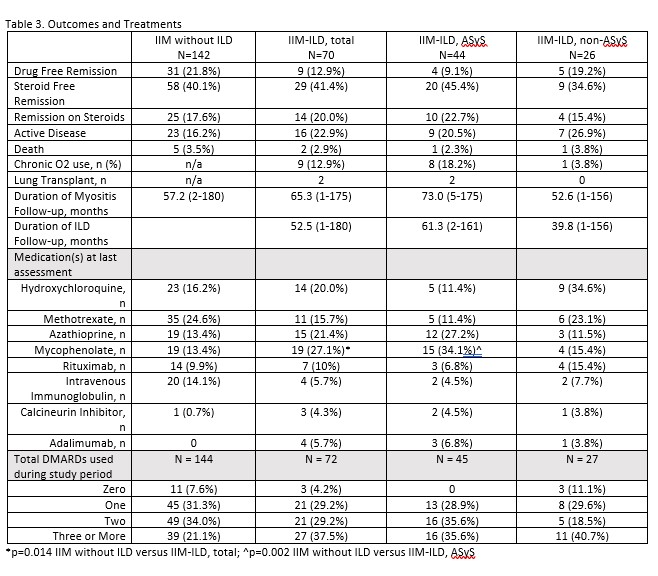
Results: Two-hundred and nineteen patients with IIM were included. ILD was present in 72 of which 45 were ILD-IIM, ASyS. Caucasians were less likely to have ILD (OR 0.49, CI 0.27-0.89). IIM-ILD presented with lower CKs, higher rates of myositis specific antibodies (OR 4.33, CI 2.07-9.04), Ro52/SSA antibodies (OR 6.63, 3.20-13.70), and dysphagia (OR 2.34, CI 1.22-4.47) (Table 1). NSIP was the most common ILD type identified radiographically (Table 2), but 11 of 18 lung biopsies demonstrated OP. At baseline, 50.7% of IIM-ILD had an FVC of 50-79% and 56.6% had a DLCO of less than 60%. FEV1 and FVC improved by 24 and 33 mL/year, respectively, and longitudinally DLCO improved as well. No significant differences were identified between subgroups at baseline or follow up (Table 2). Mycophenolate was more frequently prescribed at last assessment for IIM-ILD and specifically ASyS. Outcomes were comparable between groups (Table 3). While baseline PFTs did not correlate with most outcomes, a baseline FVC < 60% was associated with chronic O2 therapy (p< 0.01, OR 25.1, CI 2.9 – 217.1).
Conclusion: Nearly one third of our IIM population manifested with ILD. IIM-ILD was more likely to be non-Caucasian, MSA and Ro52/SSA positive, present with lower CKs, and develop dysphagia. Over half of IIM-ILD presented with moderate to severe pulmonary disease based on FVC and DLCO, but overall these parameters improved during follow up. IIM-ILD, ASyS and non-ASyS manifested with similar clinical characteristics and lung impairment. ILD remained an important source of morbidity in IIM, but did not significantly impact clinical outcomes in this large cohort.
Disclosures: I. Ward, None; E. Pepper, None; G. Loh, None.
Background/Purpose: Interstitial lung disease (ILD) is a common complication of Idiopathic Inflammatory Myopathy (IIM). This extra-muscular manifestation is a significant source of morbidity and has been described as a marker of more severe disease and increased mortality in patients with IIM. Our study aims to describe the frequency, associated clinical characteristics, and outcomes of ILD in IIM receiving care through the military healthcare system.
Methods: We performed an IRB approved, retrospective review of inflammatory myositis diagnosed within the Department of Defense (DoD) from January 2006 to December 2020. Patients were identified by ICD-10 diagnosis codes for inflammatory myositis and included if diagnosed at one of fifteen facilities within the DoD. All patients met the Bohan and Peter 1975 or EULAR/ACR classification criteria for definite or probable myositis. Inflammatory myopathies were categorized into IIM, IIM with ILD (IIM-ILD), Anti-Synthetase Syndrome (IIM-ILD, ASyS), and IIM-ILD, non-ASyS. Demographic, laboratory, pulmonary function test, imaging and biopsy data were identified at initial presentation. Pulmonary function testing, imaging and treatments were collected during the follow up period. Clinical outcomes were based on the last documentation by the evaluating physician. Data points were compared between IIM and IIM-ILD cohorts with subgroup analysis of ASyS and ILD-IIM, non-ASyS. Student’s t-tests for continuous variables and Chi square tests for categorical variables were performed. Odds ratios were calculated for statistically significant variables.
Results: Two-hundred and nineteen patients with IIM were included. ILD was present in 72 of which 45 were ILD-IIM, ASyS. Caucasians were less likely to have ILD (OR 0.49, CI 0.27-0.89). IIM-ILD presented with lower CKs, higher rates of myositis specific antibodies (OR 4.33, CI 2.07-9.04), Ro52/SSA antibodies (OR 6.63, 3.20-13.70), and dysphagia (OR 2.34, CI 1.22-4.47) (Table 1). NSIP was the most common ILD type identified radiographically (Table 2), but 11 of 18 lung biopsies demonstrated OP. At baseline, 50.7% of IIM-ILD had an FVC of 50-79% and 56.6% had a DLCO of less than 60%. FEV1 and FVC improved by 24 and 33 mL/year, respectively, and longitudinally DLCO improved as well. No significant differences were identified between subgroups at baseline or follow up (Table 2). Mycophenolate was more frequently prescribed at last assessment for IIM-ILD and specifically ASyS. Outcomes were comparable between groups (Table 3). While baseline PFTs did not correlate with most outcomes, a baseline FVC < 60% was associated with chronic O2 therapy (p< 0.01, OR 25.1, CI 2.9 – 217.1).
Conclusion: Nearly one third of our IIM population manifested with ILD. IIM-ILD was more likely to be non-Caucasian, MSA and Ro52/SSA positive, present with lower CKs, and develop dysphagia. Over half of IIM-ILD presented with moderate to severe pulmonary disease based on FVC and DLCO, but overall these parameters improved during follow up. IIM-ILD, ASyS and non-ASyS manifested with similar clinical characteristics and lung impairment. ILD remained an important source of morbidity in IIM, but did not significantly impact clinical outcomes in this large cohort.
Disclosures: I. Ward, None; E. Pepper, None; G. Loh, None.

