Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0114: Addressing Healthcare Disparities Through Implementation of a Medical Student-Based Patient Navigator Program
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GS
Grace Shadid, MS
SUNY Downstate College of Medicine
Brooklyn, NY, United States
Abstract Poster Presenter(s)
Grace Shadid1, Zaid Nakadar1, Miar Elaskandrany1, Huchong Cai1, Alejandra Moncayo1, Ayten Sergios1, Marcos Vargas1, Jeremy Wilson1, Naureen Kabani2, Olga Dvorkina1 and Ellen M. Ginzler2, 1SUNY Downstate Health Sciences University, Brooklyn, NY, 2SUNY Downstate Health Sciences University, Department of Medicine, Brooklyn, NY
Background/Purpose: African American, Afro-Caribbean, and Hispanic patients diagnosed with rheumatic diseases such as systemic lupus erythematosus (SLE) exhibit more severe disease manifestations compared to white patients. Outcomes are attributed to an interplay of genetic, environmental, and socioeconomic factors that lead to higher mortality and more rapid accrual of irreversible damage (Contreras et al. Kidney Int 2006; 69:1846-1851 and Gonzalez et al. Rheum Dis Clin N Am 2014; 40:433-454). Differences in education, health literacy, social support, income, and access to care contribute to these disparities. In addition, our Arthritis Clinic has seen an average 30% no-show rate per visit date since the COVD-19 pandemic. The objective of the Patient Navigator Program is to identify and support our underserved and high-risk patients by pairing them with 2nd year medical students, and to increase medical student understanding of health disparities that impact outcome in the rheumatic diseases.
Methods: Patients are enrolled based on a history of severe disease manifestations, poor adherence to appointments or medications, low educational level, and/or language difficulties. Seven second year medical students were recruited to become patient navigators responsible for acting as liaisons between patients and rheumatology physicians. Navigators were chosen to increase Arthritis Clinic language proficiency in Spanish, Creole, Russian, Chinese, Arabic, and Yiddish. Navigators contact patients before and after appointments, ensure prescriptions are filled, assist with scheduling follow-up or referral appointments, and aid patients with other health related concerns. Students immerse themselves within the rheumatology field through shadowing experiences. Encounters are recorded in REDCap and identify enrolled patients by their medical record number, age, gender, race/ethnicity, and date of encounter.
Results: 69 patients have been enrolled in the program; most are female (86%) and identify as black (78%). The primary diagnosis was SLE (66%). Most encounters occurred via phone call (77%) or during in-person clinic visits (20%). Assistance in scheduling appointments (35%) and wellness checks (27%) were the top reasons for an encounter.
Conclusion: The Patient Navigator Program was started to improve the care of high-risk patients suffering from SLE and other rheumatic diseases. While the program is still in its early stages, it demonstrates the ability of medical student patient navigators to connect with patients and facilitate their care. Additional research during Summer 2022 will assess patient needs, screen for food insecurity, and examine the impact on patient adherence, clinic attendance, and the educational impact on medical students.
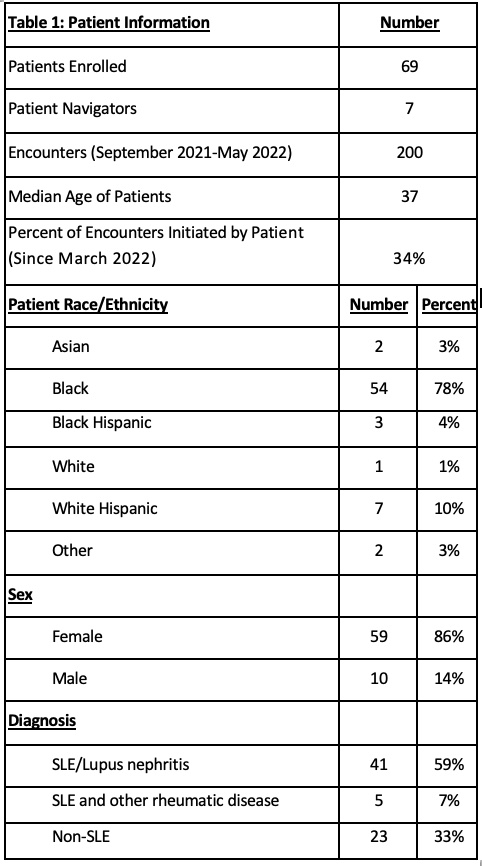 Table 1: Patient Information
Table 1: Patient Information
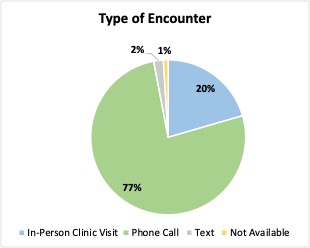 Figure 1: Type of Encounter
Figure 1: Type of Encounter
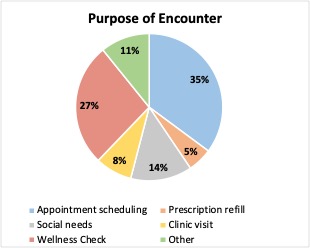 Figure 2: Purpose of Encounter
Figure 2: Purpose of Encounter
Disclosures: G. Shadid, None; Z. Nakadar, None; M. Elaskandrany, None; H. Cai, None; A. Moncayo, None; A. Sergios, None; M. Vargas, None; J. Wilson, None; N. Kabani, None; O. Dvorkina, None; E. Ginzler, Aurinia Pharma.
Background/Purpose: African American, Afro-Caribbean, and Hispanic patients diagnosed with rheumatic diseases such as systemic lupus erythematosus (SLE) exhibit more severe disease manifestations compared to white patients. Outcomes are attributed to an interplay of genetic, environmental, and socioeconomic factors that lead to higher mortality and more rapid accrual of irreversible damage (Contreras et al. Kidney Int 2006; 69:1846-1851 and Gonzalez et al. Rheum Dis Clin N Am 2014; 40:433-454). Differences in education, health literacy, social support, income, and access to care contribute to these disparities. In addition, our Arthritis Clinic has seen an average 30% no-show rate per visit date since the COVD-19 pandemic. The objective of the Patient Navigator Program is to identify and support our underserved and high-risk patients by pairing them with 2nd year medical students, and to increase medical student understanding of health disparities that impact outcome in the rheumatic diseases.
Methods: Patients are enrolled based on a history of severe disease manifestations, poor adherence to appointments or medications, low educational level, and/or language difficulties. Seven second year medical students were recruited to become patient navigators responsible for acting as liaisons between patients and rheumatology physicians. Navigators were chosen to increase Arthritis Clinic language proficiency in Spanish, Creole, Russian, Chinese, Arabic, and Yiddish. Navigators contact patients before and after appointments, ensure prescriptions are filled, assist with scheduling follow-up or referral appointments, and aid patients with other health related concerns. Students immerse themselves within the rheumatology field through shadowing experiences. Encounters are recorded in REDCap and identify enrolled patients by their medical record number, age, gender, race/ethnicity, and date of encounter.
Results: 69 patients have been enrolled in the program; most are female (86%) and identify as black (78%). The primary diagnosis was SLE (66%). Most encounters occurred via phone call (77%) or during in-person clinic visits (20%). Assistance in scheduling appointments (35%) and wellness checks (27%) were the top reasons for an encounter.
Conclusion: The Patient Navigator Program was started to improve the care of high-risk patients suffering from SLE and other rheumatic diseases. While the program is still in its early stages, it demonstrates the ability of medical student patient navigators to connect with patients and facilitate their care. Additional research during Summer 2022 will assess patient needs, screen for food insecurity, and examine the impact on patient adherence, clinic attendance, and the educational impact on medical students.
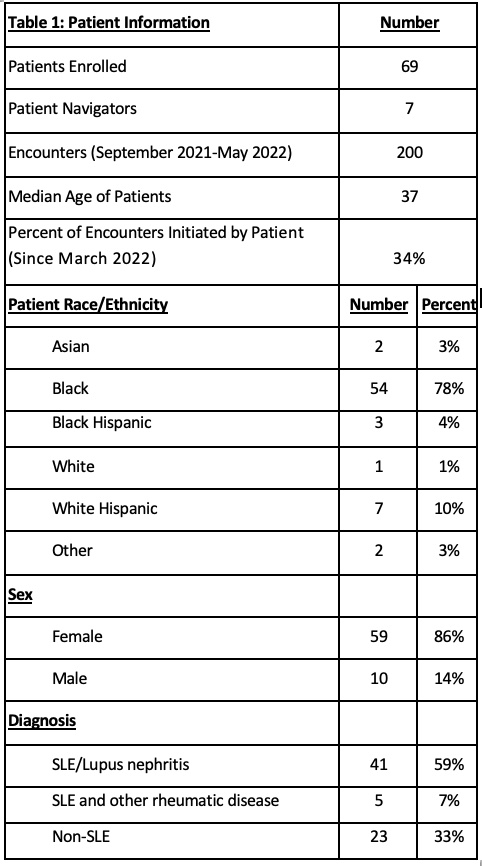 Table 1: Patient Information
Table 1: Patient Information 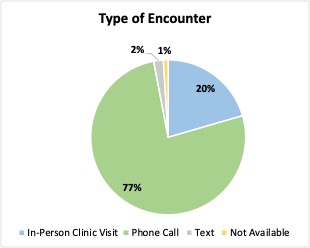 Figure 1: Type of Encounter
Figure 1: Type of Encounter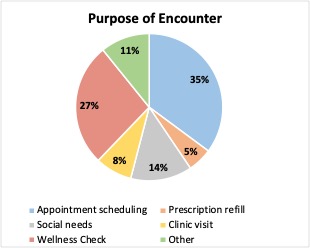 Figure 2: Purpose of Encounter
Figure 2: Purpose of EncounterDisclosures: G. Shadid, None; Z. Nakadar, None; M. Elaskandrany, None; H. Cai, None; A. Moncayo, None; A. Sergios, None; M. Vargas, None; J. Wilson, None; N. Kabani, None; O. Dvorkina, None; E. Ginzler, Aurinia Pharma.

