Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0241–0271) RA – Diagnosis, Manifestations, and Outcomes Poster I
0241: Inequity in Disease Impact Between Male and Female Rheumatoid Arthritis Patients
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GK
Gonul Koc, MD
Erasmus MC
Rotterdam, Netherlands
Abstract Poster Presenter(s)
Gonul Hazal Koc1 and Pascal de Jong2, 1Department of Rheumatology, Erasmus University Medical Centre, Rotterdam, the Netherlands, Rotterdam, Netherlands, 2ErasmusMC, Hendrik Ido Ambacht, Netherlands
Background/Purpose: Rheumatoid arthritis (RA) is more common in females than males. Moreover, males and females may have different disease courses and burdens, but data on these sex differences are lagging behind. Disease burden can be measured with patient-reported outcomes (PROs) and recently International Consortium for Health Outcomes Measurement (ICHOM) agreed upon which domains are most relevant for RA patients. These domains are pain, fatigue, activity limitation, overall emotional and physical health impact, work/school/housework ability, and productivity. Although the domains are to a certain extent addressed in previous literature, they have never been addressed all at once. Therefore, our aim is to explore the effect of sex differences on all patient-relevant outcome domains for newly-diagnosed, DMARD naïve, early RA patients over a five-year follow-up period.
Methods: For this analysis, we selected all RA patients (n = 507), according to 1987 and/or 2010 criteria, of the tREACH trial. The tREACH was a multi-center, single-blinded, stratified randomized controlled trial with a treat-to-target approach. Following PROs were compared between females and males: pain (10-point Likert scale), fatigue (FAS), functional ability (HAQ-DI), general health (VAS), quality of life (EQ-5D-3L and SF-36, including physical (PCS) and mental (MCS) component score), possible anxiety disorder and depression (HADS), and productivity loss (WPAI). An adjusted linear mixed model (LMM) and mixed-effects logistic regression model (GLMM) were used to compare them over time. The models were adjusted for age, initial treatment, DAS, and baseline PRO. PRO comparisons between sexes at diagnosis, after 2 and 5 years were made by Student's t-test, chi-squared test, or Wilcoxon rank-sum test. Effect sizes were weighted against the minimal clinically important differences (MCIDs) for each PRO.
Results: Of the 507 RA patients, 343 were female (68%). The diagnosis was made at a younger age (mean(S.D)) in women (52(14)) compared to men (57(14)). Although the baseline DAS score was similar between the sexes, the TJC (median(IQR)) was higher for females (11(6–16)) compared to males (7(3–13)). Disease activity improves over time in both sexes, but females have a more active disease compared to males (β=0.39 (95% CI 0.32, 0.45), P< 0.001)). After correction for possible confounders, including disease activity, females scored worse than males on following PROs: HAQ (β=0.08 (95% CI 0.04, 0.12), P< 0.001), fatigue (β=0.75 (95% CI 0.29, 1.21), P=0.001), morning stiffness duration (β=0.19 (95% CI 0.81, 0.030), P=0.001), and the PCS (β=-0.80 (95% CI -1.49, -0.12), P=0.020) and MCS (β=-0.73 (95% CI -1.38, -0.08), P=0.028) of the SF-36 (figure 1). Additional analyses at 2 and 5 years showed that effect sizes of adjusted sex differences for EQ-5D-3L (only 5 years), HAQ-DI (only 2 years), fatigue (2 and 5 years), and the PCS (2 and 5 years) of the SF-36 were larger than the MCID.
Conclusion: Disease activity and disease burden are intertwined and both improve with a treat-to-target approach. Nevertheless, females experience more problems in the activity limitation domain compared to men, which cannot entirely be explained by the difference in disease activity.
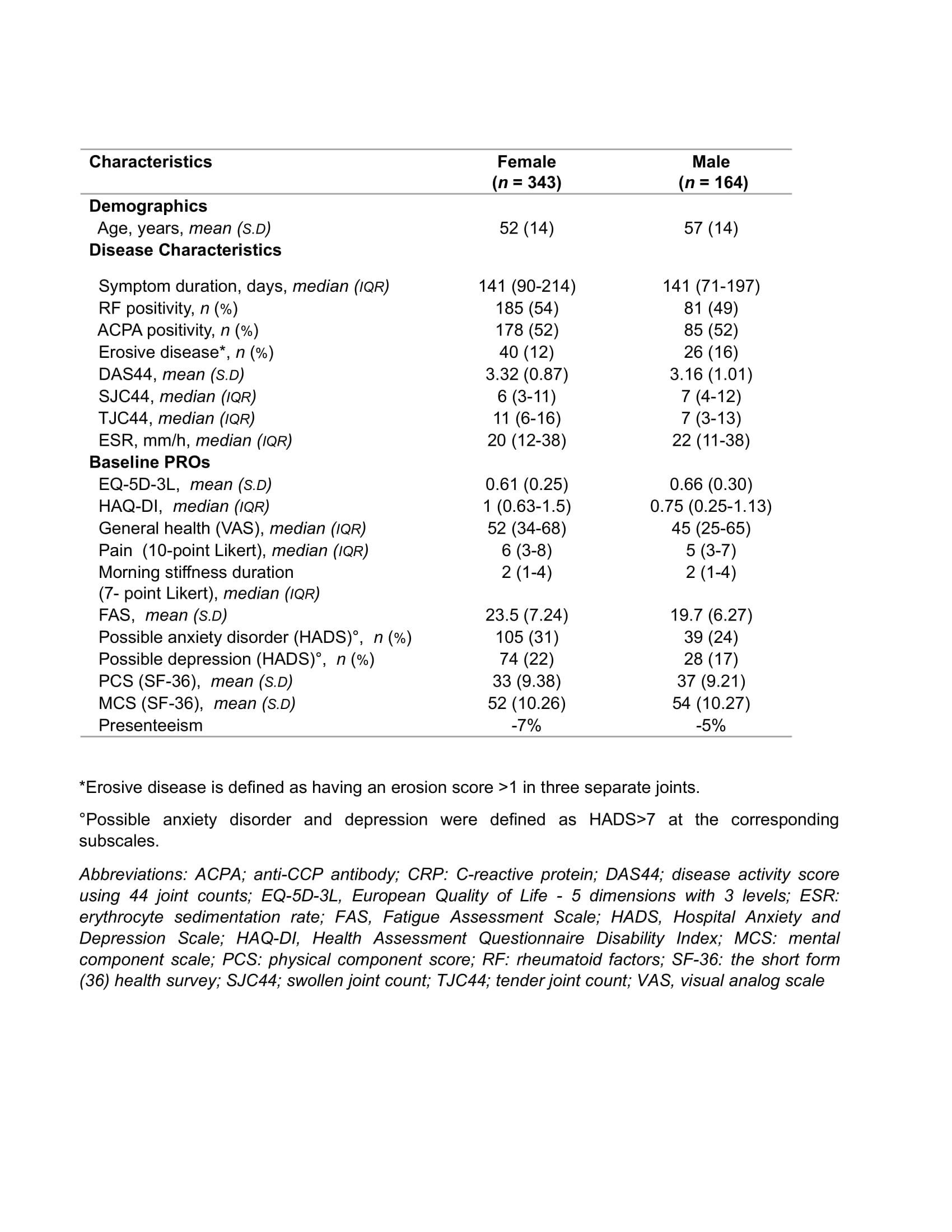 Table 1: Baseline characteristics and PROs of females and males with rheumatoid arthritis
Table 1: Baseline characteristics and PROs of females and males with rheumatoid arthritis
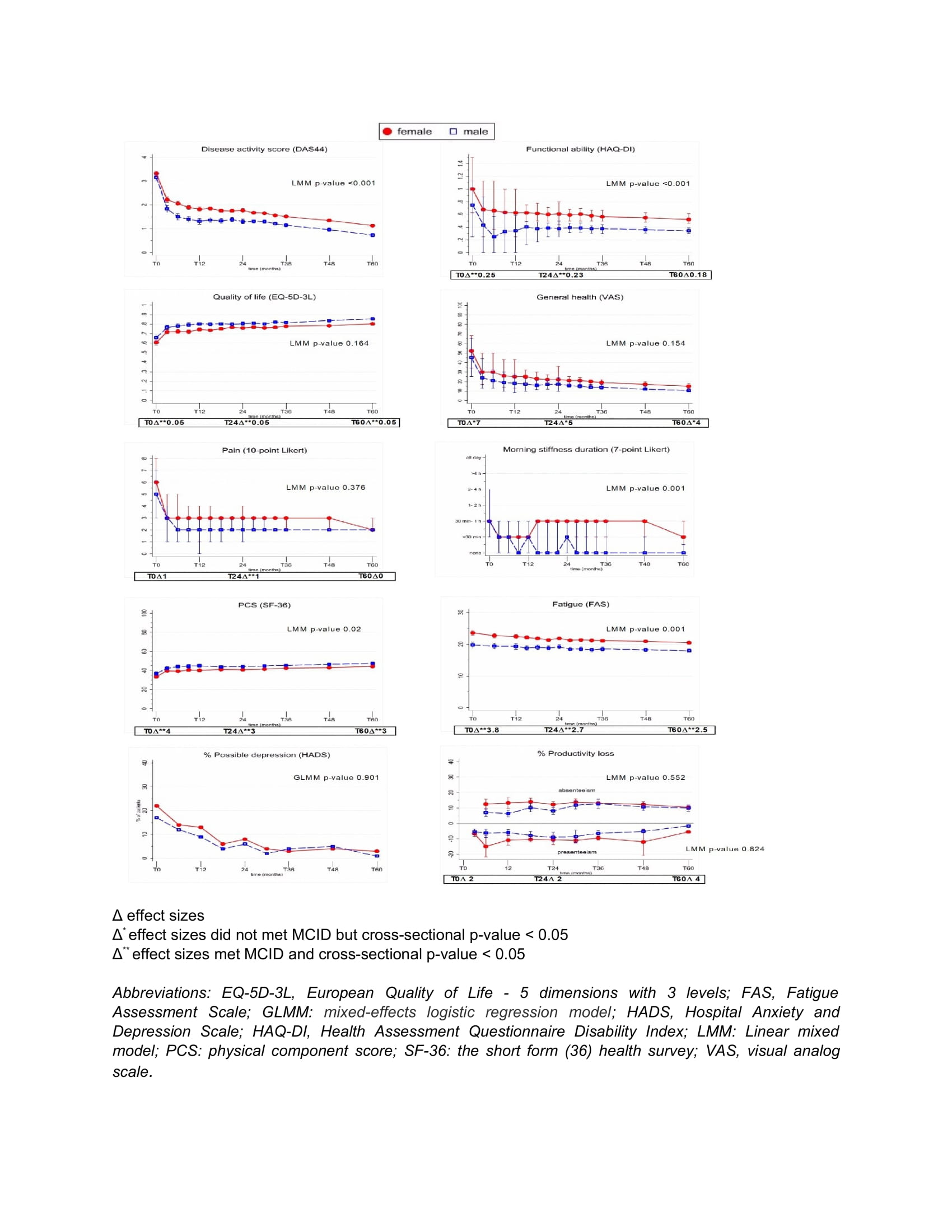 Figure 1: Disease activity and patient-reported outcomes (over time)
Figure 1: Disease activity and patient-reported outcomes (over time)
Disclosures: G. Koc, None; P. de Jong, None.
Background/Purpose: Rheumatoid arthritis (RA) is more common in females than males. Moreover, males and females may have different disease courses and burdens, but data on these sex differences are lagging behind. Disease burden can be measured with patient-reported outcomes (PROs) and recently International Consortium for Health Outcomes Measurement (ICHOM) agreed upon which domains are most relevant for RA patients. These domains are pain, fatigue, activity limitation, overall emotional and physical health impact, work/school/housework ability, and productivity. Although the domains are to a certain extent addressed in previous literature, they have never been addressed all at once. Therefore, our aim is to explore the effect of sex differences on all patient-relevant outcome domains for newly-diagnosed, DMARD naïve, early RA patients over a five-year follow-up period.
Methods: For this analysis, we selected all RA patients (n = 507), according to 1987 and/or 2010 criteria, of the tREACH trial. The tREACH was a multi-center, single-blinded, stratified randomized controlled trial with a treat-to-target approach. Following PROs were compared between females and males: pain (10-point Likert scale), fatigue (FAS), functional ability (HAQ-DI), general health (VAS), quality of life (EQ-5D-3L and SF-36, including physical (PCS) and mental (MCS) component score), possible anxiety disorder and depression (HADS), and productivity loss (WPAI). An adjusted linear mixed model (LMM) and mixed-effects logistic regression model (GLMM) were used to compare them over time. The models were adjusted for age, initial treatment, DAS, and baseline PRO. PRO comparisons between sexes at diagnosis, after 2 and 5 years were made by Student's t-test, chi-squared test, or Wilcoxon rank-sum test. Effect sizes were weighted against the minimal clinically important differences (MCIDs) for each PRO.
Results: Of the 507 RA patients, 343 were female (68%). The diagnosis was made at a younger age (mean(S.D)) in women (52(14)) compared to men (57(14)). Although the baseline DAS score was similar between the sexes, the TJC (median(IQR)) was higher for females (11(6–16)) compared to males (7(3–13)). Disease activity improves over time in both sexes, but females have a more active disease compared to males (β=0.39 (95% CI 0.32, 0.45), P< 0.001)). After correction for possible confounders, including disease activity, females scored worse than males on following PROs: HAQ (β=0.08 (95% CI 0.04, 0.12), P< 0.001), fatigue (β=0.75 (95% CI 0.29, 1.21), P=0.001), morning stiffness duration (β=0.19 (95% CI 0.81, 0.030), P=0.001), and the PCS (β=-0.80 (95% CI -1.49, -0.12), P=0.020) and MCS (β=-0.73 (95% CI -1.38, -0.08), P=0.028) of the SF-36 (figure 1). Additional analyses at 2 and 5 years showed that effect sizes of adjusted sex differences for EQ-5D-3L (only 5 years), HAQ-DI (only 2 years), fatigue (2 and 5 years), and the PCS (2 and 5 years) of the SF-36 were larger than the MCID.
Conclusion: Disease activity and disease burden are intertwined and both improve with a treat-to-target approach. Nevertheless, females experience more problems in the activity limitation domain compared to men, which cannot entirely be explained by the difference in disease activity.
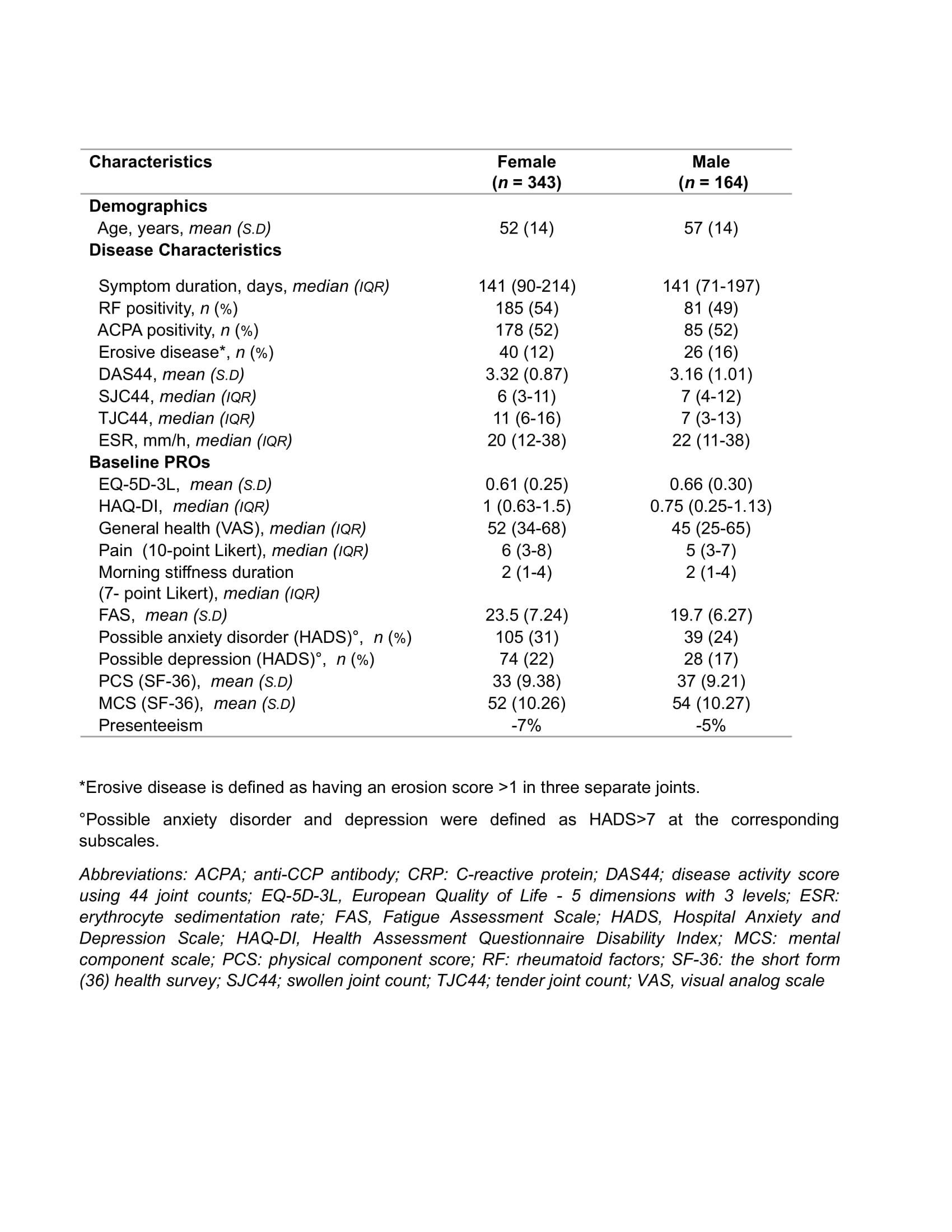 Table 1: Baseline characteristics and PROs of females and males with rheumatoid arthritis
Table 1: Baseline characteristics and PROs of females and males with rheumatoid arthritis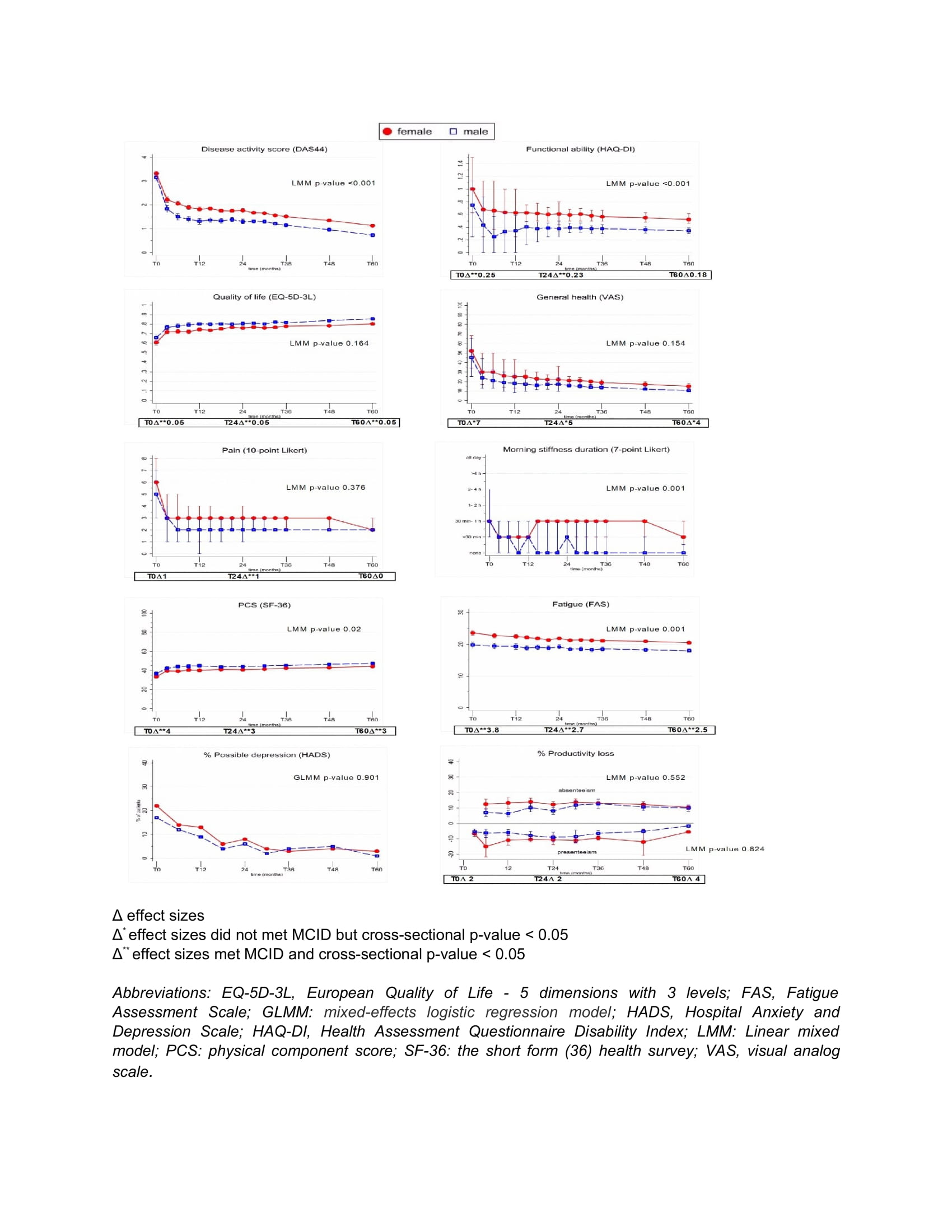 Figure 1: Disease activity and patient-reported outcomes (over time)
Figure 1: Disease activity and patient-reported outcomes (over time)Disclosures: G. Koc, None; P. de Jong, None.

