Back
Poster Session A
Patient engagement/self-management
Session: (PP01–PP22) Patient Perspectives Poster
PP03: To Err Is Human: The Need for Patients with Rheumatic and Musculoskeletal Diseases to Continuously Monitor Their Health Care Records
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- IH
Ida Hakkarinen, -None-
self (patient)
Greenbelt, MD, United StatesDisclosure: Disclosure(s): No financial relationships with ineligible companies to disclose
Patient Poster Presenter(s)
Ida Hakkarinen, Greenbelt, MD
Background/Purpose: In November 1999, the Institute of Medicine issued a press release announcing publication of To Err is Human: Building a Safer Health System (Kohn et al., 2000), which documented medical errors and their impacts upon patient safety. The report was a watershed moment for the US health care system.
Over my 10-year journey with Granulomatosis with Polyangiitis, my health care experiences have included encountering errors in health care records, financial data, and insurance claims diagnoses. The Federal rule implementing policies related to the 21st Century Cures Act issued in April 2021 outlined eight types of clinical notes in Electronic Health Information to be made available to patients without charge as part of the US Core Data for Interoperability.
Intervention: In July 2021, I underwent an ultrasound of my neck and downloaded the radiology report to find the clinical history for a different patient had been assigned to me. The radiology Fellow interpreted the imagery based upon a 65-year-old woman with a history of surgery and thyroid cancer. When I reported this, I learned there'd been incorrect patient identification – a "Red Rule" violation.
Figure 1 shows the "Swiss Cheese" model of failure in human systems (Reason, 1990). In my case, atrophy of my thyroid gland had been interpreted incorrectly as previous surgery. This error was compounded by a second one, due to duplicate medical record numbers in the enterprise Radiology Picture Archiving and Communications System.
After reviewing the summary bill from a recent hospitalization, I noted the drug costs were high. I requested an itemized bill and found I'd been charged twice for an infusion drug I'd only received once.
Figure 2 shows mistakes discovered from a review of my Personal Health Record in my health insurance portal. Incorrect diagnosis codes can lead to errors in research that uses health claims databases.
Maintenance: Patients with Rheumatic and Musculoskeletal Diseases often have chronic conditions and see multiple specialists for treatment. Clear communication with one's medical team is vital to minimize risk.
I regularly confirm verbally the next step of a procedure. After working with a pharmacy clerk to obtain a high-dose influenza vaccine, I repeated to the pharmacist I was getting the high dose. Looking at the vial, he saw he had the regular dose.
Written discharge instructions for a recent hospitalization showed the tablet increment (2.5 mg) listed for a drug was half the pharmacy-provided tablet increment (5 mg.) Health literacy is important in reducing errors.
Quality of Life: The Patient Advocacy Coordinator for my academic medical center has been helpful in resolving issues I've raised. I've submitted an application to serve on the hospital's Patient and Family Advisory Council for Safety and Quality.
Communication (Figure 3) is indeed the most frequently used medical procedure, and I strive to ensure mine is proactive, clear, and concise when I partner with my team.
References Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
Reason J. Human Error. Cambridge: Cambridge University Press; 1990.
.jpg) Swiss Cheese Model of Failure in Human Systems (Reason, 1990)
Swiss Cheese Model of Failure in Human Systems (Reason, 1990)
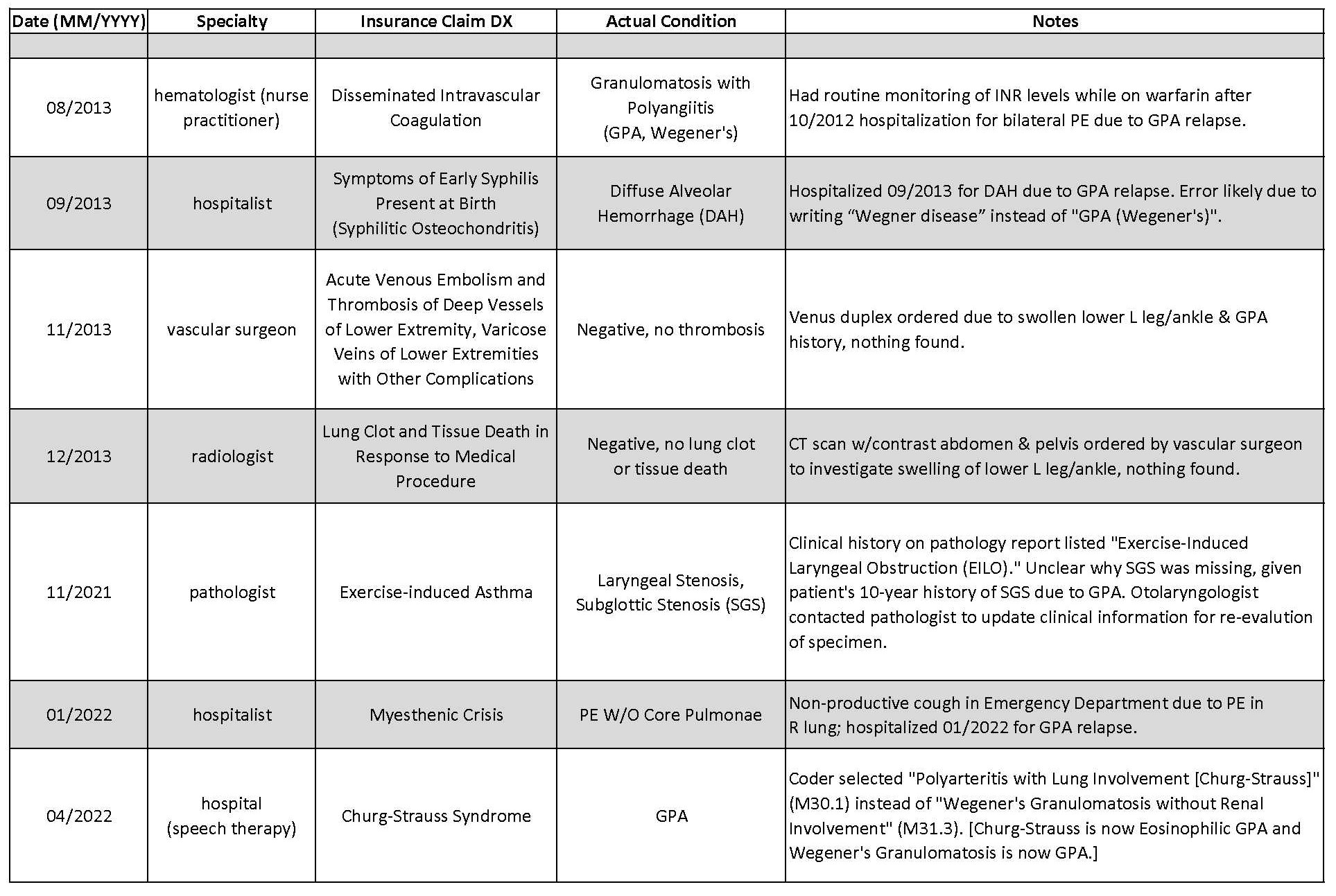 Author's Insurance Information Showing Claim Diagnosis (DX) Submitted versus Actual Condition
Author's Insurance Information Showing Claim Diagnosis (DX) Submitted versus Actual Condition
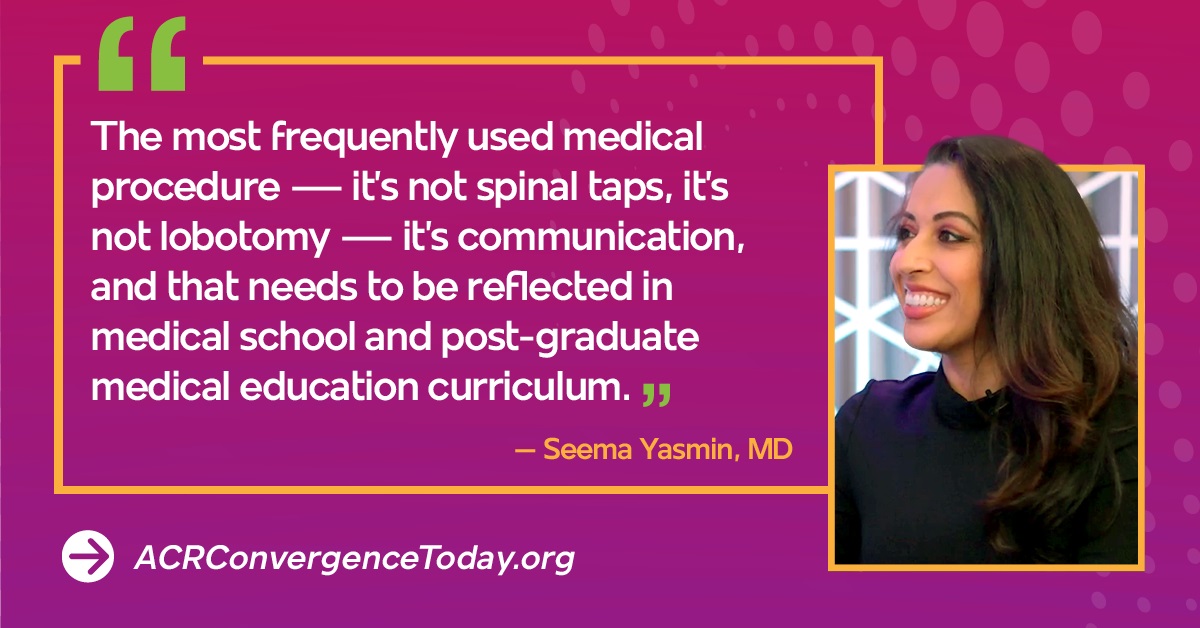 ACR Convergence 2021 Keynote Speaker on the Importance of Communication
ACR Convergence 2021 Keynote Speaker on the Importance of Communication
Disclosures: I. Hakkarinen, None.
Background/Purpose: In November 1999, the Institute of Medicine issued a press release announcing publication of To Err is Human: Building a Safer Health System (Kohn et al., 2000), which documented medical errors and their impacts upon patient safety. The report was a watershed moment for the US health care system.
Over my 10-year journey with Granulomatosis with Polyangiitis, my health care experiences have included encountering errors in health care records, financial data, and insurance claims diagnoses. The Federal rule implementing policies related to the 21st Century Cures Act issued in April 2021 outlined eight types of clinical notes in Electronic Health Information to be made available to patients without charge as part of the US Core Data for Interoperability.
Intervention: In July 2021, I underwent an ultrasound of my neck and downloaded the radiology report to find the clinical history for a different patient had been assigned to me. The radiology Fellow interpreted the imagery based upon a 65-year-old woman with a history of surgery and thyroid cancer. When I reported this, I learned there'd been incorrect patient identification – a "Red Rule" violation.
Figure 1 shows the "Swiss Cheese" model of failure in human systems (Reason, 1990). In my case, atrophy of my thyroid gland had been interpreted incorrectly as previous surgery. This error was compounded by a second one, due to duplicate medical record numbers in the enterprise Radiology Picture Archiving and Communications System.
After reviewing the summary bill from a recent hospitalization, I noted the drug costs were high. I requested an itemized bill and found I'd been charged twice for an infusion drug I'd only received once.
Figure 2 shows mistakes discovered from a review of my Personal Health Record in my health insurance portal. Incorrect diagnosis codes can lead to errors in research that uses health claims databases.
Maintenance: Patients with Rheumatic and Musculoskeletal Diseases often have chronic conditions and see multiple specialists for treatment. Clear communication with one's medical team is vital to minimize risk.
I regularly confirm verbally the next step of a procedure. After working with a pharmacy clerk to obtain a high-dose influenza vaccine, I repeated to the pharmacist I was getting the high dose. Looking at the vial, he saw he had the regular dose.
Written discharge instructions for a recent hospitalization showed the tablet increment (2.5 mg) listed for a drug was half the pharmacy-provided tablet increment (5 mg.) Health literacy is important in reducing errors.
Quality of Life: The Patient Advocacy Coordinator for my academic medical center has been helpful in resolving issues I've raised. I've submitted an application to serve on the hospital's Patient and Family Advisory Council for Safety and Quality.
Communication (Figure 3) is indeed the most frequently used medical procedure, and I strive to ensure mine is proactive, clear, and concise when I partner with my team.
References Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
Reason J. Human Error. Cambridge: Cambridge University Press; 1990.
.jpg) Swiss Cheese Model of Failure in Human Systems (Reason, 1990)
Swiss Cheese Model of Failure in Human Systems (Reason, 1990)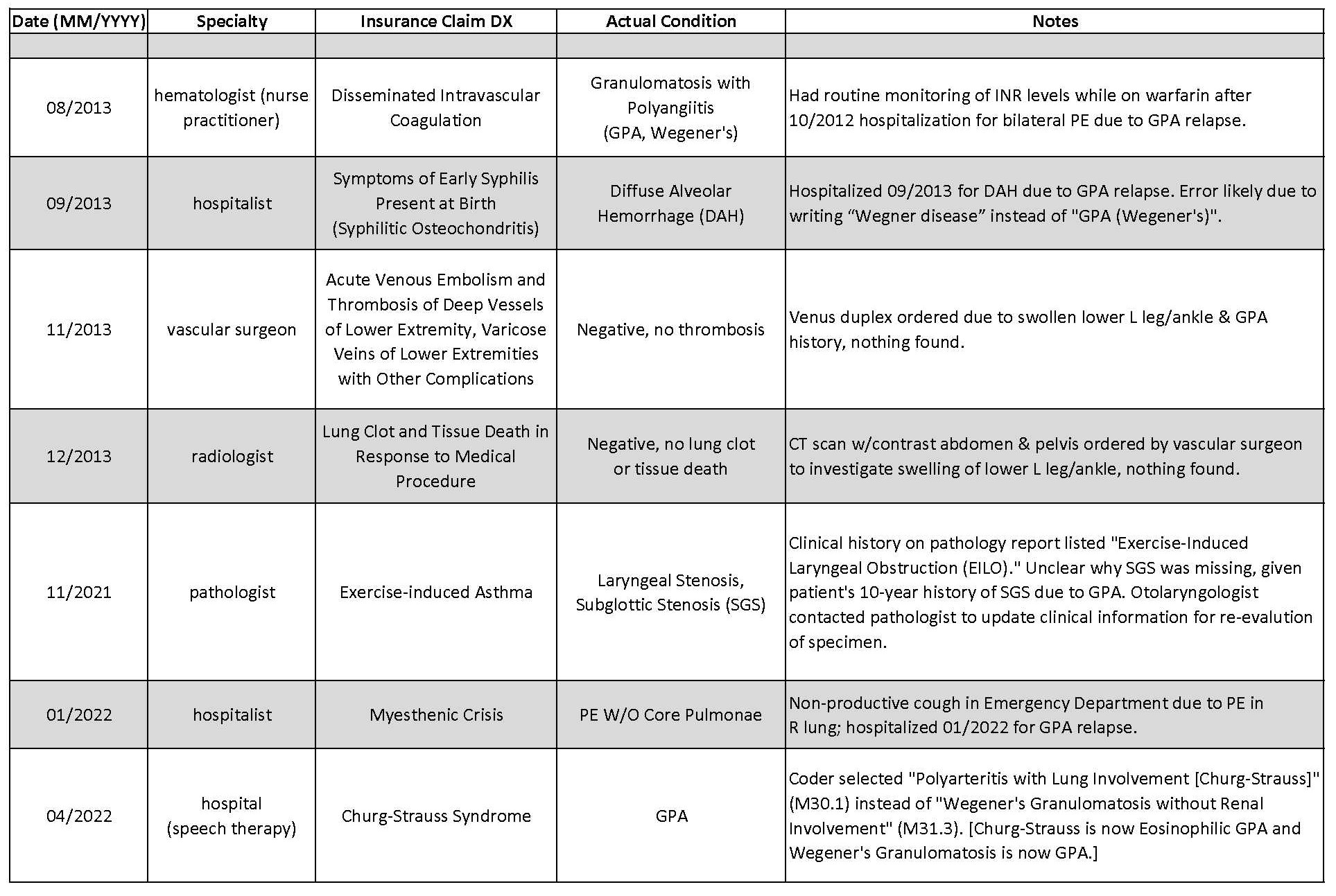 Author's Insurance Information Showing Claim Diagnosis (DX) Submitted versus Actual Condition
Author's Insurance Information Showing Claim Diagnosis (DX) Submitted versus Actual Condition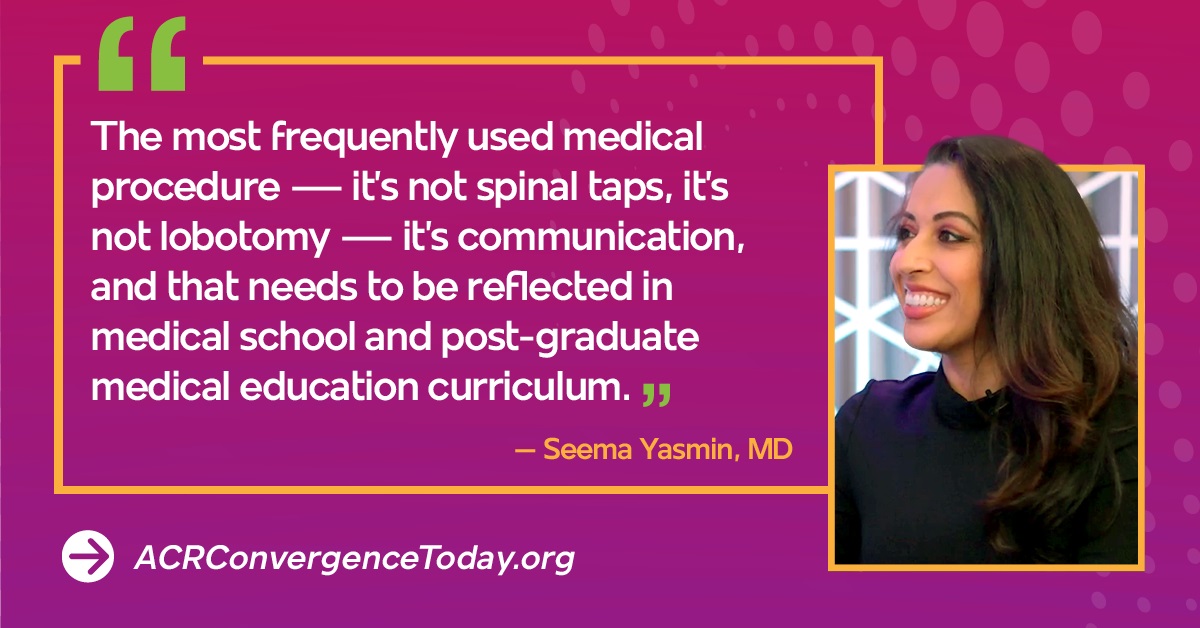 ACR Convergence 2021 Keynote Speaker on the Importance of Communication
ACR Convergence 2021 Keynote Speaker on the Importance of CommunicationDisclosures: I. Hakkarinen, None.

