Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0377: Differences in Early-onset vs. Late-onset Psoriatic Arthritis: Data from the RESPONDIA and REGISPONSER Studies
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Maria Angeles Puche Larrubia, PhD
Reina Sofia University Hospital
Cordoba, Spain
Abstract Poster Presenter(s)
Maria Angeles Puche Larrubia1, lourdes Ladehesa-Pineda2, María Dolores López Montilla2, Raquel Granados3, Eduardo Collantes4 and Clementina Lopez-Medina5, 1Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Granada, Spain, 2Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Cordoba, Spain, 3Reina Sofia University Hospital/Rheumatology Department/Maimonides Institute for Biomedical Research (IMIBIC), Córdoba, Spain, 4IMIBIC/University of Cordoba/Reina Sofia Hospital, Cordoba, Spain, 5Reina Sofia University Hospital, Rheumatology Department, Jaén, Spain
Background/Purpose: The prevalence of late-onset Psoriatic Arthritis (PsA) is increasing in parallel with the progressive aging of the population. The elderly population presents a greater functional deterioration and a greater number of comorbidities. With this study we aim to find clinically relevant differences to predict the evolution and prognosis of the disease depending on the onset of the symptoms to carry out a more exhaustive follow-up. The objective is to evaluate the association of the age at onset of PsA symptoms with the characteristics and burden of the disease.
Methods: Observational study that includes a subgroup of 231 patients with PsA from the REGISPONSER study (Registry of Spondyloarthritis of Spanish Rheumatology) and the RESPONDIA study (Ibero-American Registry of Spondyloarthropathies). Patients were divided into two groups according to the age of PsA onset (early-onset: ≤40 years old and late-onset: ≥60 years old). The characteristics and burden of the disease were compared using the Student's t-test/Mann-Whitney U test or using the chi-square/Fisher test. Binary logistic regression was performed to determine the factors associated with late-onset psoriatic arthritis.
Results: 231 patients were included [early-onset 179 (77.5%); late-onset 52 (22.5%)] (Table 1). There was a significant higher percentage of men in the late-onset group [94 (62.3%) vs. 38 (86.4%)]. A lower presence of sacroiliitis was found in patients with late-onset PsA [6 (12.2%) vs 58 (32.6%)] as well as enthesitis [5 (9.8%) vs 44 (24.6%)]. Regarding the comorbidities, there was a higher frequency of heart disease among patients with late-onset PsA [4 (7.8%) vs. 0 (0%)]. In respect of the outcome measures, the late-onset group showed higher scores in BASFI [3.3 (2.5) vs. 2.2 (2.2)] and lower scores in FSF12 component [34.6 (8.7) vs. 38.7 (10.5)]. The radiographic indices measured by BASRI showed worse results in those patients with late-onset disease both in the spine [2.9 (3) vs 1.6 (2)] and in the total BASRI [3.4 (3 .4) vs 1.9 (2.4)]. Late-onset PsA is associated with being male (OR 4.4, 95% CI: 1.3, 16.3), greater structural damage (total BASRI) (OR 3.3, 95% CI: 1.3, 8.1), higher frequency of arthritis (upper limbs) (OR 2.8, 95% CI: 1, 7.7), and greater loss of functionality (BASFI) (OR 1.3, 95% CI: 1, 1.6) (Table 2). In addition, it is associated with a shorter diagnostic delay (OR 0.7, 95% CI: 0.6, 0.8), lower frequency of enthesitis (OR 0.1, 95% CI: 0, 0.5), and sacroiliitis (OR 0.06, 95% CI: 0, 0.5).
Conclusion: Our study suggests that the age of onset of PsA was associated with different characteristics of the disease. Patients with late-onset PsA were more frequently males, showed worse functionality and more structural damage. Sacroiliitis and enthesitis were found less frequently in the late-onset group. Quality of life, disease activity and treatments taken were not associated significantly with age of onset. Late-onset PsA is associated with being male, greater structural damage, higher frequency of arthritis (upper limbs), and greater loss of functionality (BASFI). Finally, it is associated with a shorter diagnostic delay, lower frequency of enthesitis and sacroiliitis.
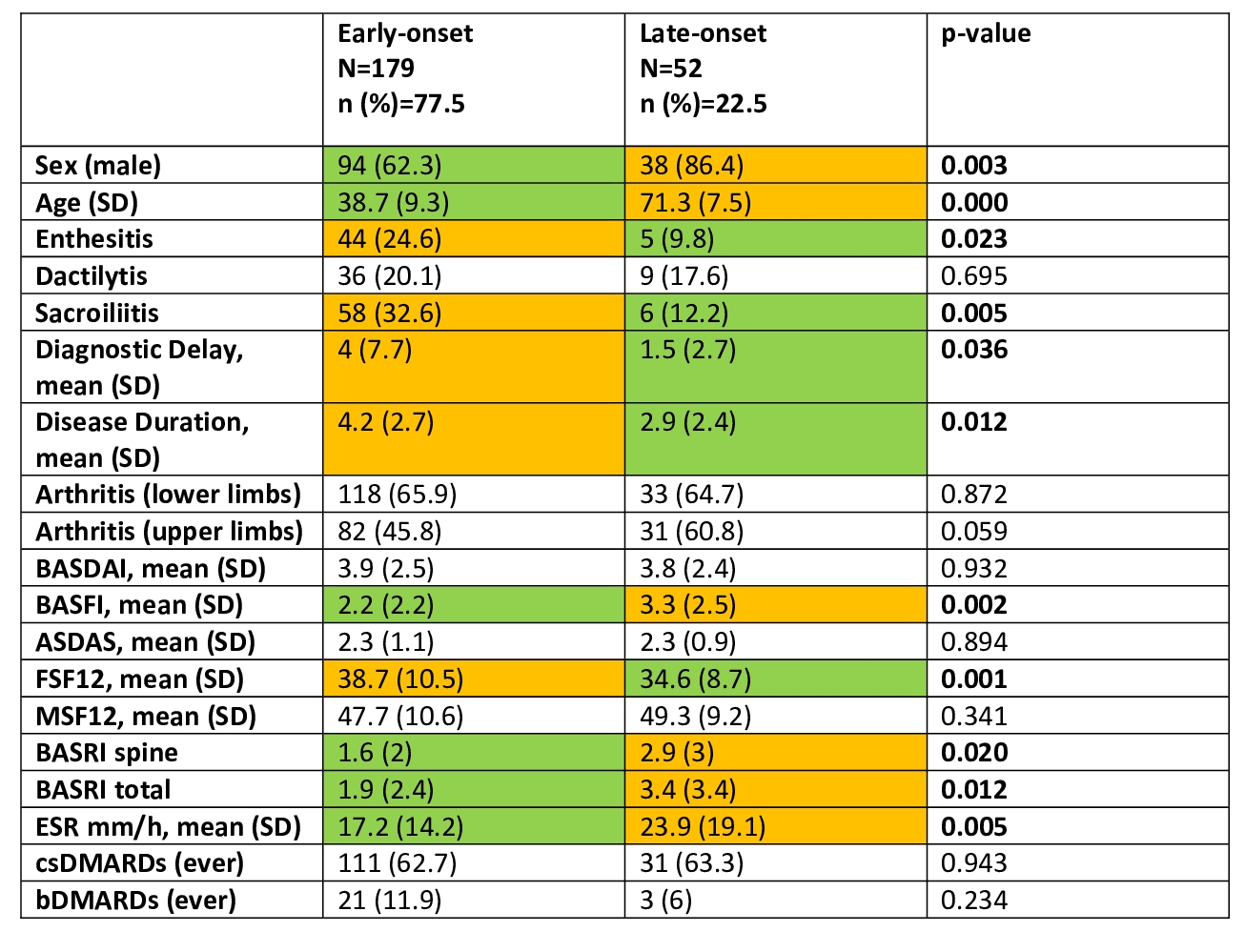 Table 1. Description of different characteristics between two groups: early and late onset
Table 1. Description of different characteristics between two groups: early and late onset
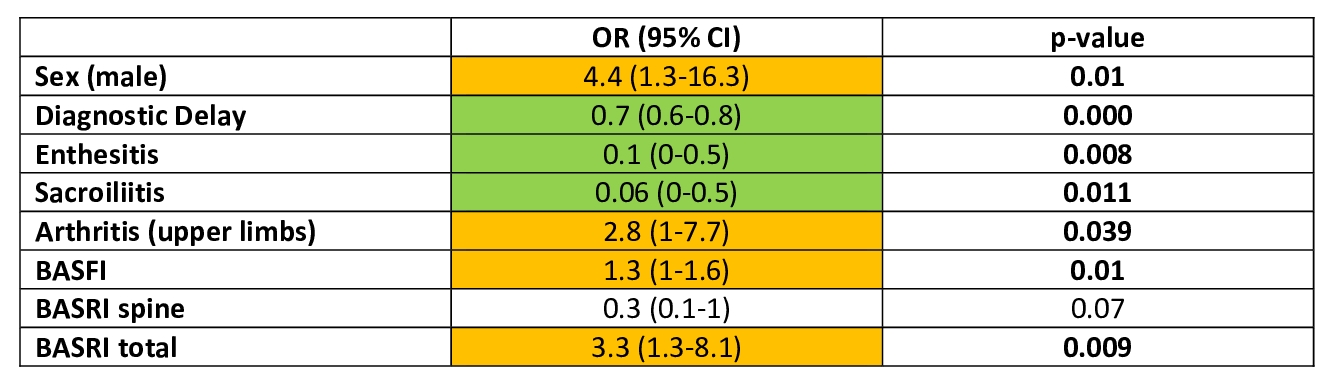 Table 2. Factors associated with late-onset psoriatic arthritis
Table 2. Factors associated with late-onset psoriatic arthritis
Disclosures: M. Puche Larrubia, None; l. Ladehesa-Pineda, None; M. López Montilla, None; R. Granados, None; E. Collantes, None; C. Lopez-Medina, None.
Background/Purpose: The prevalence of late-onset Psoriatic Arthritis (PsA) is increasing in parallel with the progressive aging of the population. The elderly population presents a greater functional deterioration and a greater number of comorbidities. With this study we aim to find clinically relevant differences to predict the evolution and prognosis of the disease depending on the onset of the symptoms to carry out a more exhaustive follow-up. The objective is to evaluate the association of the age at onset of PsA symptoms with the characteristics and burden of the disease.
Methods: Observational study that includes a subgroup of 231 patients with PsA from the REGISPONSER study (Registry of Spondyloarthritis of Spanish Rheumatology) and the RESPONDIA study (Ibero-American Registry of Spondyloarthropathies). Patients were divided into two groups according to the age of PsA onset (early-onset: ≤40 years old and late-onset: ≥60 years old). The characteristics and burden of the disease were compared using the Student's t-test/Mann-Whitney U test or using the chi-square/Fisher test. Binary logistic regression was performed to determine the factors associated with late-onset psoriatic arthritis.
Results: 231 patients were included [early-onset 179 (77.5%); late-onset 52 (22.5%)] (Table 1). There was a significant higher percentage of men in the late-onset group [94 (62.3%) vs. 38 (86.4%)]. A lower presence of sacroiliitis was found in patients with late-onset PsA [6 (12.2%) vs 58 (32.6%)] as well as enthesitis [5 (9.8%) vs 44 (24.6%)]. Regarding the comorbidities, there was a higher frequency of heart disease among patients with late-onset PsA [4 (7.8%) vs. 0 (0%)]. In respect of the outcome measures, the late-onset group showed higher scores in BASFI [3.3 (2.5) vs. 2.2 (2.2)] and lower scores in FSF12 component [34.6 (8.7) vs. 38.7 (10.5)]. The radiographic indices measured by BASRI showed worse results in those patients with late-onset disease both in the spine [2.9 (3) vs 1.6 (2)] and in the total BASRI [3.4 (3 .4) vs 1.9 (2.4)]. Late-onset PsA is associated with being male (OR 4.4, 95% CI: 1.3, 16.3), greater structural damage (total BASRI) (OR 3.3, 95% CI: 1.3, 8.1), higher frequency of arthritis (upper limbs) (OR 2.8, 95% CI: 1, 7.7), and greater loss of functionality (BASFI) (OR 1.3, 95% CI: 1, 1.6) (Table 2). In addition, it is associated with a shorter diagnostic delay (OR 0.7, 95% CI: 0.6, 0.8), lower frequency of enthesitis (OR 0.1, 95% CI: 0, 0.5), and sacroiliitis (OR 0.06, 95% CI: 0, 0.5).
Conclusion: Our study suggests that the age of onset of PsA was associated with different characteristics of the disease. Patients with late-onset PsA were more frequently males, showed worse functionality and more structural damage. Sacroiliitis and enthesitis were found less frequently in the late-onset group. Quality of life, disease activity and treatments taken were not associated significantly with age of onset. Late-onset PsA is associated with being male, greater structural damage, higher frequency of arthritis (upper limbs), and greater loss of functionality (BASFI). Finally, it is associated with a shorter diagnostic delay, lower frequency of enthesitis and sacroiliitis.
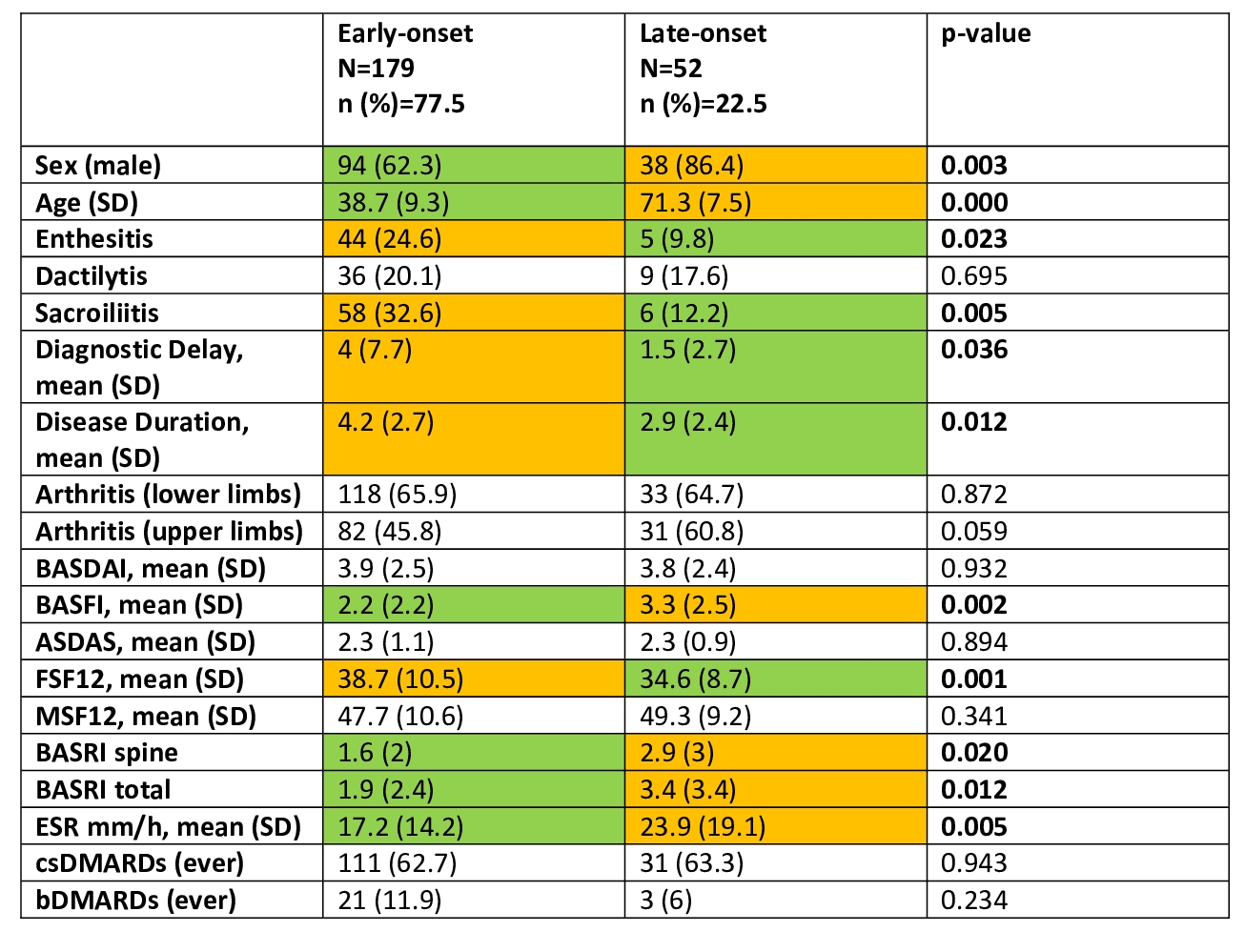 Table 1. Description of different characteristics between two groups: early and late onset
Table 1. Description of different characteristics between two groups: early and late onset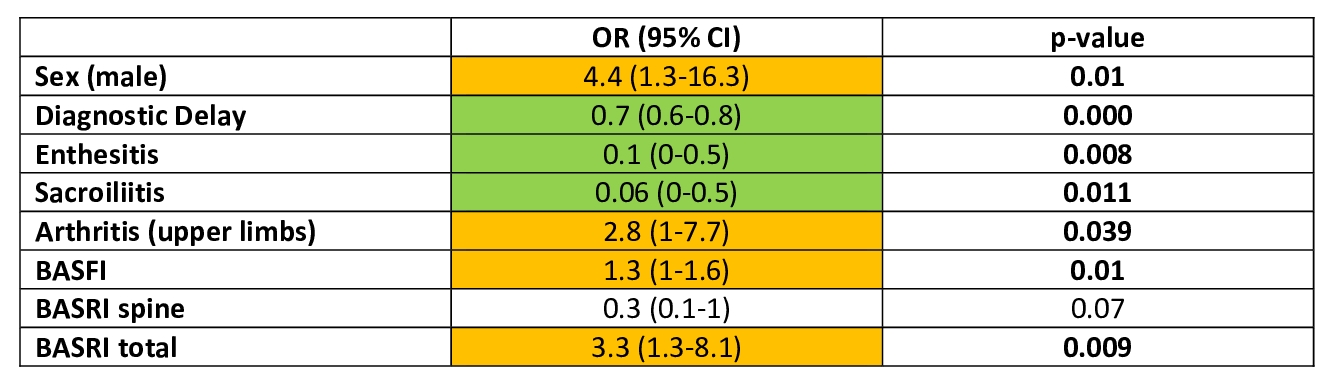 Table 2. Factors associated with late-onset psoriatic arthritis
Table 2. Factors associated with late-onset psoriatic arthritisDisclosures: M. Puche Larrubia, None; l. Ladehesa-Pineda, None; M. López Montilla, None; R. Granados, None; E. Collantes, None; C. Lopez-Medina, None.

