Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0241–0271) RA – Diagnosis, Manifestations, and Outcomes Poster I
0246: Comorbidity Clusters in Patients with Rheumatoid Arthritis Predict Survival Prognosis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
.png)
Cynthia S. Crowson, PhD
Mayo Clinic
Eyota, MN, United States
Abstract Poster Presenter(s)
Cynthia Crowson1, Tina Gunderson2, John Davis2, Elena Myasoedova2, Vanessa Kronzer2, Caitrin Coffey2, Bradly Kimbrough3 and Elizabeth Atkinson2, 1Mayo Clinic, Eyota, MN, 2Mayo Clinic, Rochester, MN, 3Mayo Clinic Rochester, Rochester, MN
Background/Purpose: Comorbidities are common in patients with rheumatoid arthritis (RA), but there is little information regarding the occurrence of distinct comorbidity patterns in patients with RA and how these patterns impact outcomes. We aimed to examine clusters of patients with RA based on comorbidities and the impact of these clusters on mortality.
Methods: In this retrospective, population-based study, residents of a geographically well-defined area with prevalent RA on 1-1-2015 were identified from a comprehensive medical record linkage system. Patients were followed for vital status until death, last contact or 12-31-2021. Diagnostic codes were retrieved for 5-years prior to the prevalence date. Using 2 codes at least 30 days apart, a previously described set of 55 comorbidities were defined. Latent class analysis (LCA) was used to cluster patients based on comorbidity patterns, and the optimal number of clusters was determined by Bayesian Information Criteria. Standardized mortality ratios (SMR) were used to assess differences in mortality across the clusters.
Results: A total of 1643 patients with prevalent RA (72% female; 94% white; median age 64 years, median RA duration 7 years) were studied. Comorbidities were present in 1548 (94%) of the subjects with 5+ comorbidities present in 980 (59%) subjects.
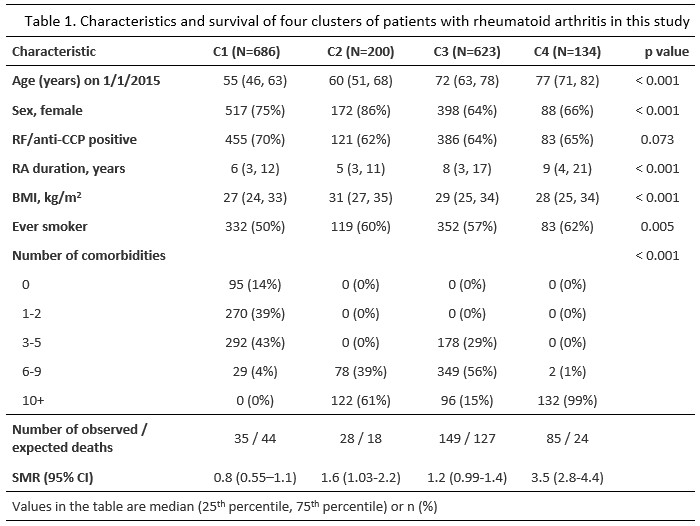
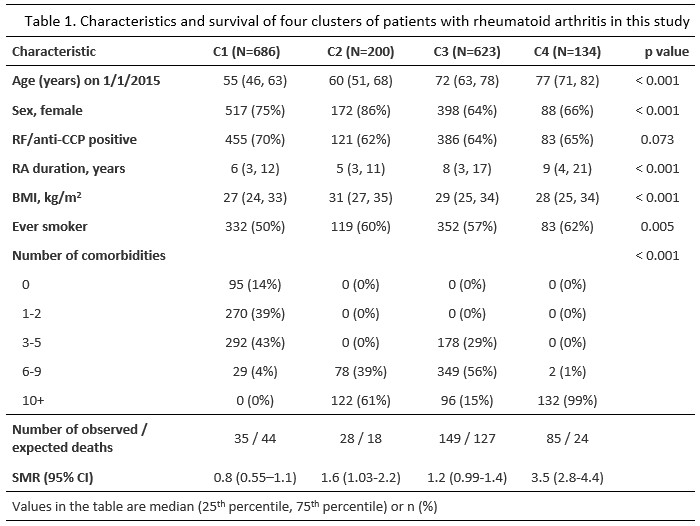
LCA identified 4 clusters of patients. Although only comorbidities were used in the LCA, the clusters differed by age, sex, number of comorbidities, smoking status, body mass index (BMI) and RF/ anti-CCP positivity (Table 1). Cluster 1 (n=686) included younger patients (median age 55 years) who were less likely to smoke and had fewer comorbidities than those in the other clusters. At the other extreme, cluster 4 (n=134) included older patients (median age 77 years) with 6+ comorbidities who were more likely to have smoked. Cluster 2 (n=200) included younger patients (median age 60 years) with 6+ comorbidities and high BMI, while cluster 3 (n=623) included the remaining patients with comorbidities also common in the general population (median age 72 years, 3+ comorbidities consisting mainly of hypertension, hyperlipidemia and back problems). Cluster 1 had no increased mortality based on US lifetables (SMR 0.8; 95% confidence interval [CI: 0.55-1.1). Cluster 4 had the worst survival (SMR 3.5; 95% CI 2.8-4.4). Cluster 2 also had poor survival (SMR 1.6; 95% CI 1.03-2.2), while the poor survival in cluster 3 was less pronounced (SMR 1.2; 95% CI 0.99-1.4).
Conclusion: Clustering of patients with RA into subgroups based on comorbidity profiles identified distinct groups that exhibited differing survival outcomes compared with expected mortality in the general population. This demonstrates comorbidities congregate in some patients, leading to poor prognosis, while other patients may experience fewer comorbidities and may have a better survival experience than people without RA. Comorbidity patterns may hold the key to moving beyond a one-size-fits-all perspective of survival for patients with RA. Further research is needed to elucidate the contributions of RA disease activity and comorbidity patterns in the long-term prognosis of RA.
Disclosures: C. Crowson, None; T. Gunderson, None; J. Davis, Pfizer; E. Myasoedova, None; V. Kronzer, None; C. Coffey, None; B. Kimbrough, None; E. Atkinson, None.
Background/Purpose: Comorbidities are common in patients with rheumatoid arthritis (RA), but there is little information regarding the occurrence of distinct comorbidity patterns in patients with RA and how these patterns impact outcomes. We aimed to examine clusters of patients with RA based on comorbidities and the impact of these clusters on mortality.
Methods: In this retrospective, population-based study, residents of a geographically well-defined area with prevalent RA on 1-1-2015 were identified from a comprehensive medical record linkage system. Patients were followed for vital status until death, last contact or 12-31-2021. Diagnostic codes were retrieved for 5-years prior to the prevalence date. Using 2 codes at least 30 days apart, a previously described set of 55 comorbidities were defined. Latent class analysis (LCA) was used to cluster patients based on comorbidity patterns, and the optimal number of clusters was determined by Bayesian Information Criteria. Standardized mortality ratios (SMR) were used to assess differences in mortality across the clusters.
Results: A total of 1643 patients with prevalent RA (72% female; 94% white; median age 64 years, median RA duration 7 years) were studied. Comorbidities were present in 1548 (94%) of the subjects with 5+ comorbidities present in 980 (59%) subjects.
LCA identified 4 clusters of patients. Although only comorbidities were used in the LCA, the clusters differed by age, sex, number of comorbidities, smoking status, body mass index (BMI) and RF/ anti-CCP positivity (Table 1). Cluster 1 (n=686) included younger patients (median age 55 years) who were less likely to smoke and had fewer comorbidities than those in the other clusters. At the other extreme, cluster 4 (n=134) included older patients (median age 77 years) with 6+ comorbidities who were more likely to have smoked. Cluster 2 (n=200) included younger patients (median age 60 years) with 6+ comorbidities and high BMI, while cluster 3 (n=623) included the remaining patients with comorbidities also common in the general population (median age 72 years, 3+ comorbidities consisting mainly of hypertension, hyperlipidemia and back problems). Cluster 1 had no increased mortality based on US lifetables (SMR 0.8; 95% confidence interval [CI: 0.55-1.1). Cluster 4 had the worst survival (SMR 3.5; 95% CI 2.8-4.4). Cluster 2 also had poor survival (SMR 1.6; 95% CI 1.03-2.2), while the poor survival in cluster 3 was less pronounced (SMR 1.2; 95% CI 0.99-1.4).
Conclusion: Clustering of patients with RA into subgroups based on comorbidity profiles identified distinct groups that exhibited differing survival outcomes compared with expected mortality in the general population. This demonstrates comorbidities congregate in some patients, leading to poor prognosis, while other patients may experience fewer comorbidities and may have a better survival experience than people without RA. Comorbidity patterns may hold the key to moving beyond a one-size-fits-all perspective of survival for patients with RA. Further research is needed to elucidate the contributions of RA disease activity and comorbidity patterns in the long-term prognosis of RA.
Disclosures: C. Crowson, None; T. Gunderson, None; J. Davis, Pfizer; E. Myasoedova, None; V. Kronzer, None; C. Coffey, None; B. Kimbrough, None; E. Atkinson, None.

