Back
Poster Session A
Professional development and education
Session: (0214–0240) Professional Education Poster
0219: COVID-19 Impact on Second Year Medical Students Experience with Interactive Patient Encounters as a Supplement to Teaching the Skin and Rheumatology Course
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EL
Emily Littman, BS
University of Central Florida College of Medicine
Boca Raton, FL, United States
Abstract Poster Presenter(s)
Emily Littman1, Jeremy Adamson2 and Shazia Beg3, 1UCF College of Medicine, Boca Raton, FL, 2UCF College of Medicine, Orlando, FL, 3UCF, Orlando, FL
Background/Purpose: The use of interactive patient scenarios has long been a valuable component of medical school curricula, as this type of learning facilitates empathy, comprehensive understanding, and cultural sensitivity. The COVID-19 pandemic, however, has precipitated a shift to more virtual strategies to keep students, faculty, and patients safe. We evaluated second year medical students' perceptions on the use of live patient encounters during the teaching of the skin and rheumatology course (BMS 6635) using different teaching formats due to changes from the COVID-19 pandemic.
Methods: Four to five patients with systemic lupus erythematosus, psoriatic arthritis, dermatomyositis, scleroderma, and pyoderma gangrenosum volunteered to participate in an interactive teaching session with medical students at the University of Central Florida College of Medicine (UCF COM). Second year medical students enrolled in BMS 6635 were asked to complete a survey about their learning experiences using these patient cases. Participation was voluntary. Students who did not respond to the survey questions were excluded. Data analysis using Chi Square testing was performed on survey responses obtained pre-pandemic as compared to those collected in academic years 2020-2021 and 2021-2022 during the COVID-19 pandemic.
Results: 700 surveys were obtained after patient cases given in different formats. When the interactive patient cases were given in person before COVID-19, 93% of students enjoyed the cases and 95% of students believed that the cases were an appropriate learning experience in their education. When these cases were delivered virtually beginning in the academic year 2020-2021, however, students' enjoyment of these cases decreased to 86%, with 92% of students believing that the cases were an appropriate learning experience in their education. This is a 7% and 9% decrease, respectively, from pre-pandemic years. During the academic year 2021-2022, use of a hybrid model, with students and faculty in-person and patients participating virtually, resulted in 81% of students enjoying the interactive patient cases and 83% of students believing that the cases were an appropriate learning experience in their education. This was a 12% decrease from before the COVID-19 pandemic (p < .001) and a 5% and 9% decrease, respectively, from the previous year (p < .001) (Figure 1). 37% of students who had their cases in a completely virtual format preferred the interactive patient sessions to stay completely virtual, while 51% of students who participated in hybrid sessions during COVID-19 preferred the sessions to be completely virtual (p< .029) (Table 1).
Conclusion: The use of live interactive patient cases in medical school education has been met with positive feedback over the years. As such, these interactive case strategies should continue to be used in medical education. This study showed that medical students had a decrease in enjoyment when changed to a completely virtual format and an even further decrease when changed to a hybrid format. Careful consideration should be given to delivery format to optimize student learning and enjoyment.
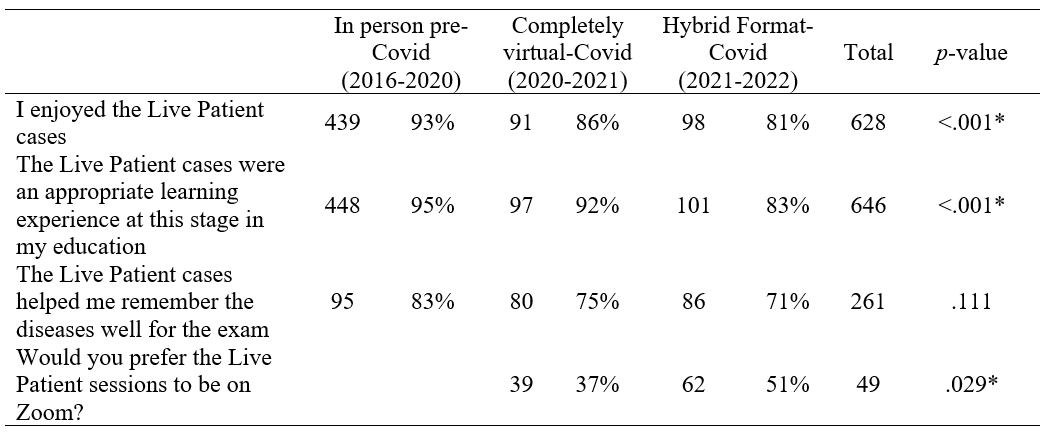 Table. 1 Medical student survey responses comparing live patient encounters given in person, completely virtually, and a hybrid format.
Table. 1 Medical student survey responses comparing live patient encounters given in person, completely virtually, and a hybrid format.
* = Statistical significance defined as p < 0.05.
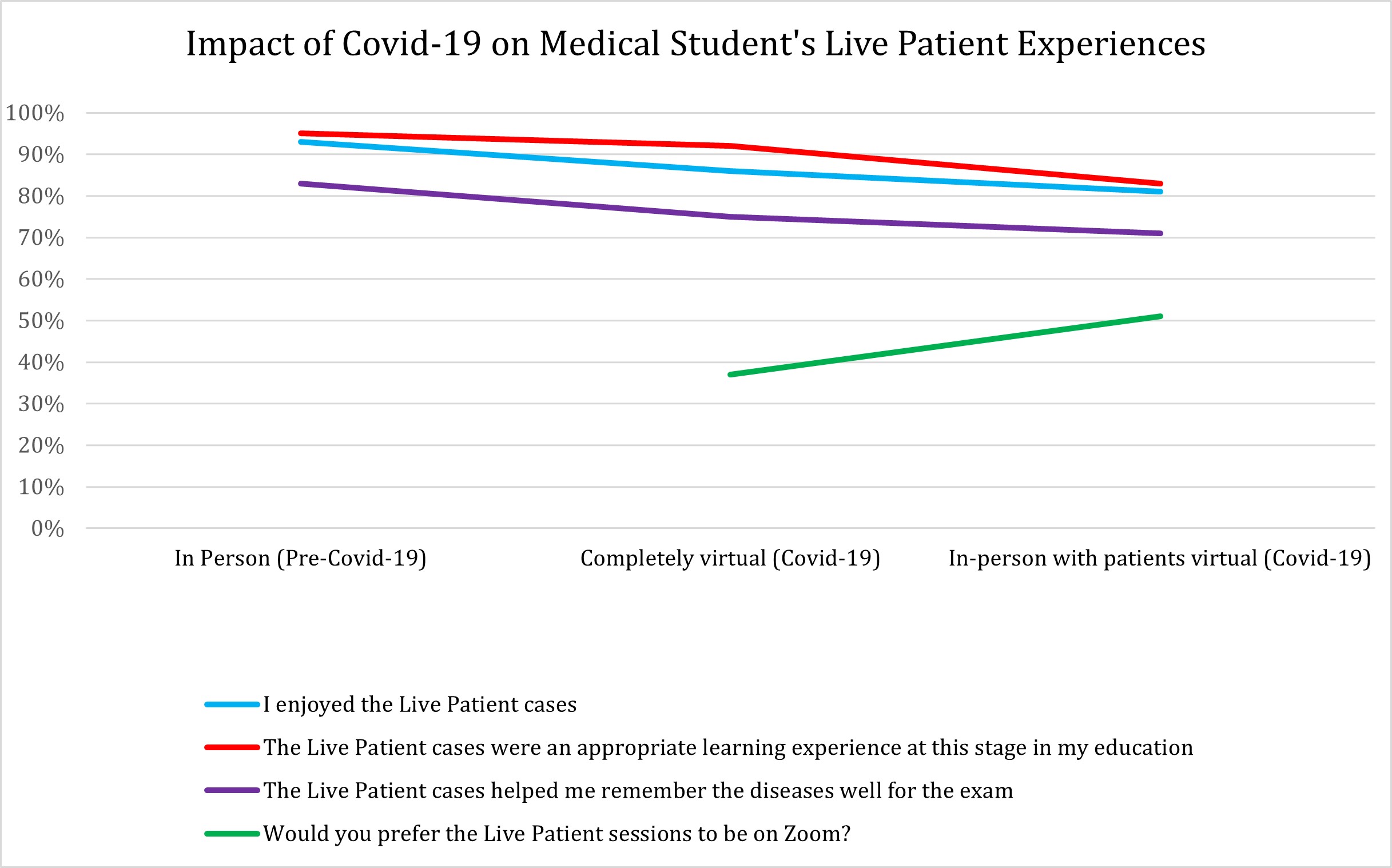 Figure 1. Medical students’ feedback on live patient cases given in different platforms before COVID-19 and during the COVID-19 pandemic.
Figure 1. Medical students’ feedback on live patient cases given in different platforms before COVID-19 and during the COVID-19 pandemic.
Disclosures: E. Littman, None; J. Adamson, None; S. Beg, None.
Background/Purpose: The use of interactive patient scenarios has long been a valuable component of medical school curricula, as this type of learning facilitates empathy, comprehensive understanding, and cultural sensitivity. The COVID-19 pandemic, however, has precipitated a shift to more virtual strategies to keep students, faculty, and patients safe. We evaluated second year medical students' perceptions on the use of live patient encounters during the teaching of the skin and rheumatology course (BMS 6635) using different teaching formats due to changes from the COVID-19 pandemic.
Methods: Four to five patients with systemic lupus erythematosus, psoriatic arthritis, dermatomyositis, scleroderma, and pyoderma gangrenosum volunteered to participate in an interactive teaching session with medical students at the University of Central Florida College of Medicine (UCF COM). Second year medical students enrolled in BMS 6635 were asked to complete a survey about their learning experiences using these patient cases. Participation was voluntary. Students who did not respond to the survey questions were excluded. Data analysis using Chi Square testing was performed on survey responses obtained pre-pandemic as compared to those collected in academic years 2020-2021 and 2021-2022 during the COVID-19 pandemic.
Results: 700 surveys were obtained after patient cases given in different formats. When the interactive patient cases were given in person before COVID-19, 93% of students enjoyed the cases and 95% of students believed that the cases were an appropriate learning experience in their education. When these cases were delivered virtually beginning in the academic year 2020-2021, however, students' enjoyment of these cases decreased to 86%, with 92% of students believing that the cases were an appropriate learning experience in their education. This is a 7% and 9% decrease, respectively, from pre-pandemic years. During the academic year 2021-2022, use of a hybrid model, with students and faculty in-person and patients participating virtually, resulted in 81% of students enjoying the interactive patient cases and 83% of students believing that the cases were an appropriate learning experience in their education. This was a 12% decrease from before the COVID-19 pandemic (p < .001) and a 5% and 9% decrease, respectively, from the previous year (p < .001) (Figure 1). 37% of students who had their cases in a completely virtual format preferred the interactive patient sessions to stay completely virtual, while 51% of students who participated in hybrid sessions during COVID-19 preferred the sessions to be completely virtual (p< .029) (Table 1).
Conclusion: The use of live interactive patient cases in medical school education has been met with positive feedback over the years. As such, these interactive case strategies should continue to be used in medical education. This study showed that medical students had a decrease in enjoyment when changed to a completely virtual format and an even further decrease when changed to a hybrid format. Careful consideration should be given to delivery format to optimize student learning and enjoyment.
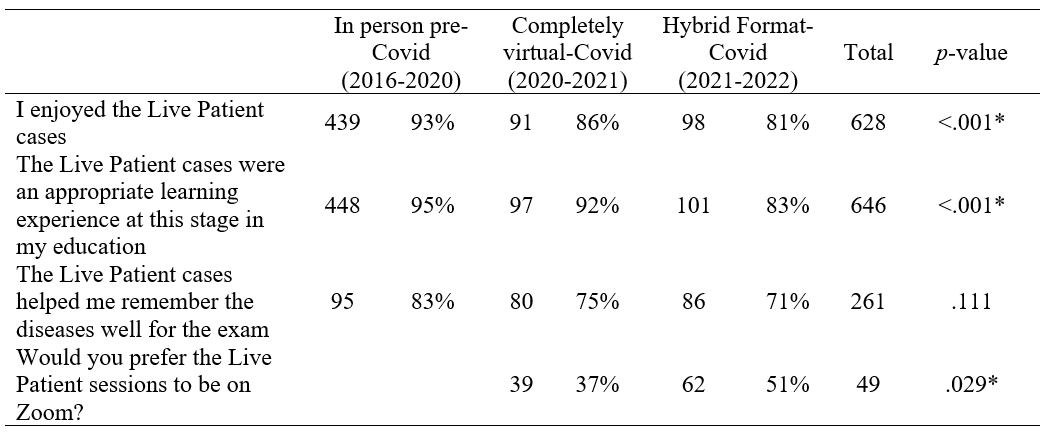 Table. 1 Medical student survey responses comparing live patient encounters given in person, completely virtually, and a hybrid format.
Table. 1 Medical student survey responses comparing live patient encounters given in person, completely virtually, and a hybrid format. * = Statistical significance defined as p < 0.05.
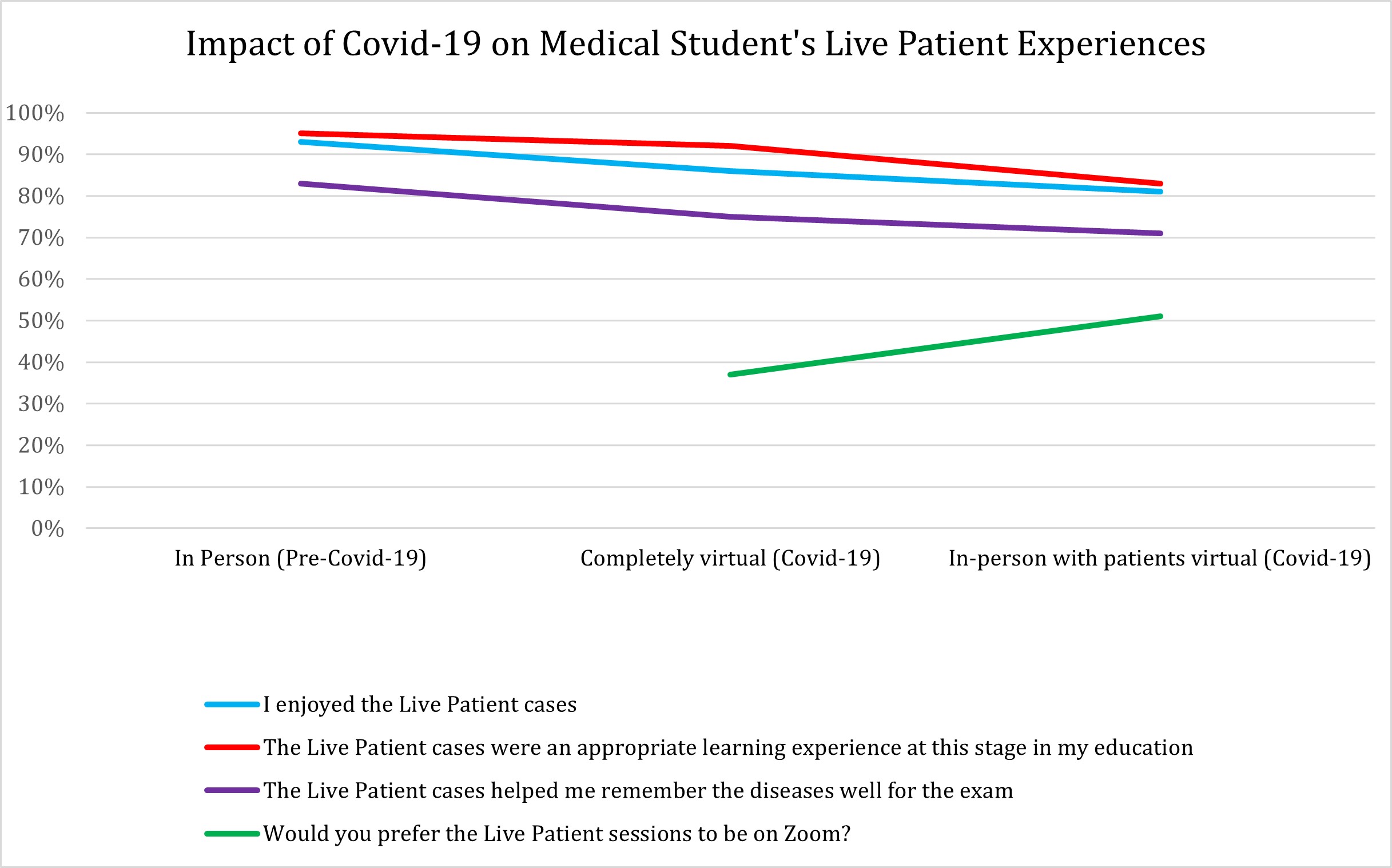 Figure 1. Medical students’ feedback on live patient cases given in different platforms before COVID-19 and during the COVID-19 pandemic.
Figure 1. Medical students’ feedback on live patient cases given in different platforms before COVID-19 and during the COVID-19 pandemic.Disclosures: E. Littman, None; J. Adamson, None; S. Beg, None.

