Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0403–0431) Spondyloarthritis Including PsA – Treatment Poster I: AxSpA
0411: Bimekizumab Improves Signs and Symptoms Including Inflammation in Patients with Active Ankylosing Spondylitis: 24-Week Efficacy & Safety from a Phase 3, Multicenter, Randomized, Placebo Controlled Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- XB
Xenofon Baraliakos, MD
Rheumazentrum Ruhrgebiet Herne
Herne, Germany
Abstract Poster Presenter(s)
Désirée van der Heijde1, Xenofon Baraliakos2, Maxime Dougados3, Matthew Brown4, Denis Poddubnyy5, Filip Van den bosch6, Nigil Haroon7, Huji Xu8, Tetsuya Tomita9, Lianne Gensler10, Marga Oortgiesen11, Carmen Fleurinck12, Natasha de Peyrecave13, Thomas Vaux14, Alexander Marten15 and Atul Deodhar16, 1Department of Rheumatology, Leiden University Medical Center, Leiden, The Netherlands, Leiden, Netherlands, 2Rheumazentrum Ruhrgebiet Herne, Herne, Germany, 3Department of Rheumatology, Hôpital Cochin, Paris, France, Paris, France, 4Genomics England, London, United Kingdom, 5Department of Gastroenterology, Infectious Diseases and Rheumatology, Charité – Universitätsmedizin Berlin, Berlin, Germany, 6Department of Internal Medicine and Paediatrics, Ghent University and VIB Centre for Inflammation Research, Ghent, Belgium, 7Schroeder Arthritis Institute, University Health Network; University of Toronto, Toronto, ON, Canada, 8Department of Rheumatology and Immunology, Shanghai Changzheng Hospital, Affiliated to Second Military Medical University, Shanghai, China, 9Department of Orthopaedic Biomaterial Science, Osaka University Graduate School of Medicine, Osaka, Japan, Suita Osaka, Japan, 10Department of Medicine, Division of Rheumatology, University of California San Francisco, San Francisco, CA, 11UCB Pharma, Raleigh, NC, 12UCB Pharma, Brussels, Belgium, Oosterzele, Belgium, 13UCB Pharma, Brussels, Belgium, 14UCB Pharma, Slough, United Kingdom, 15UCB Pharma, Monheim am Rhein, Germany, 16Oregon Health & Science University, Portland, OR, USA, Portland, OR
Background/Purpose: Bimekizumab (BKZ) is a monoclonal IgG1 antibody that selectively inhibits IL-17F in addition to IL-17A. In a phase 2b study, BKZ showed rapid and sustained efficacy and was well tolerated up to 156 weeks (wks) in patients (pts) with active ankylosing spondylitis (AS).1,2 Here, we assess efficacy and safety of BKZ vs placebo (PBO) in pts with active AS up to Wk 24 in the ongoing pivotal phase 3 study, BE MOBILE 2.
Methods: BE MOBILE 2 (NCT03928743) comprises a 16-wk double blind, PBO-controlled period and 36-wk maintenance period. Pts were aged ≥18 years (yrs), met modified New York Criteria and had active AS (BASDAI ≥4, spinal pain ≥4) at baseline (BL). Pts were randomized 2:1, BKZ 160 mg Q4W:PBO. From Wk 16, all pts received BKZ 160 mg Q4W. Primary and secondary efficacy endpoints were assessed at Wk 16, and up to Wk 24. Treatment-emergent adverse events (TEAEs; MedDRA v19.0) are reported among patients who received ≥1 BKZ dose by preferred term up to Wk 24.
Results: Of 332 randomized pts (BKZ: 221; PBO: 111), 322 (97.0%) completed Wk 16 and 313 (94.3%) Wk 24. BL characteristics were comparable between groups: mean age 40.4 yrs, symptom duration 13.5 yrs; 27.7% pts female, 85.5% HLA-B27+, 16.3% TNFi-inadequate responders (IR).
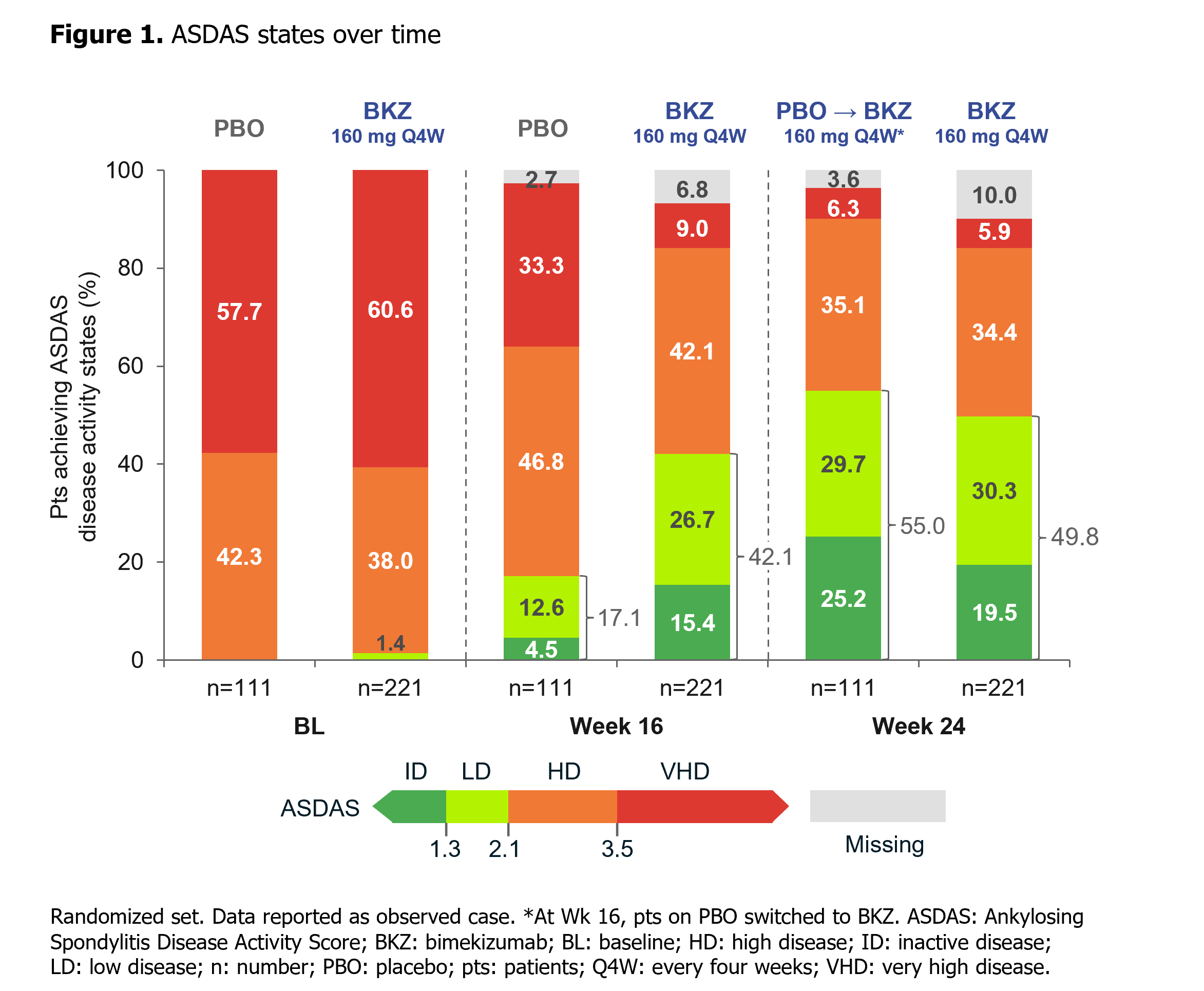
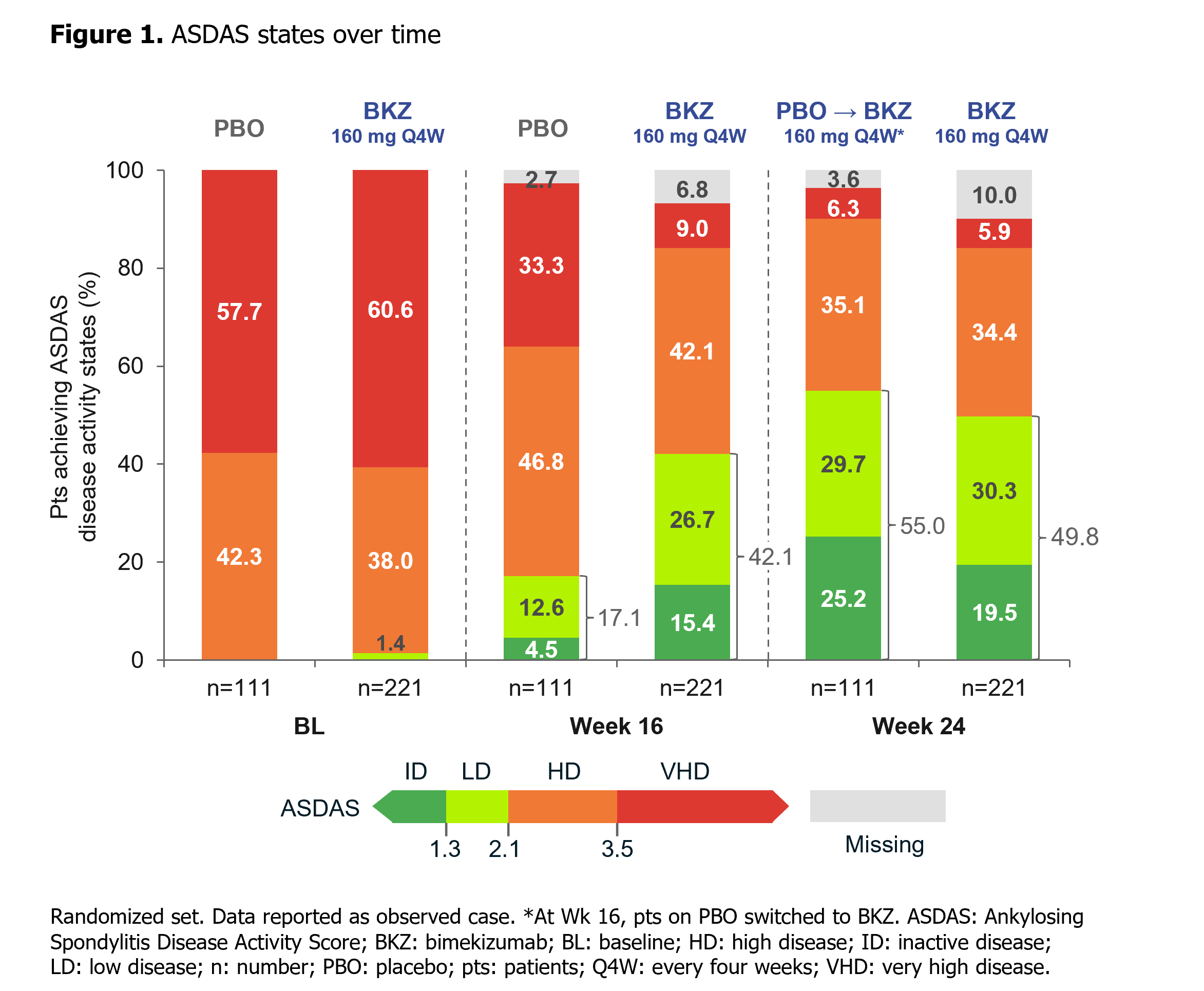
At Wk 16, the primary (ASAS40: 44.8% BKZ vs 22.5% PBO; p< 0.001) and all ranked secondary endpoints were met (Table). ASAS40 responses at Wk 16 were consistent across both TNFi-naïve (45.7% BKZ vs 23.4% PBO) and TNFi-IR (40.5% BKZ vs 17.6% PBO) populations. Responses with BKZ were rapid, including in PBO pts who switched to BKZ at Wk 16, and increased to Wk 24 (Table; Figure 1). At Wk 24, nearly 50% BKZ-randomized pts had achieved ASDAS < 2.1 (Figure 1).
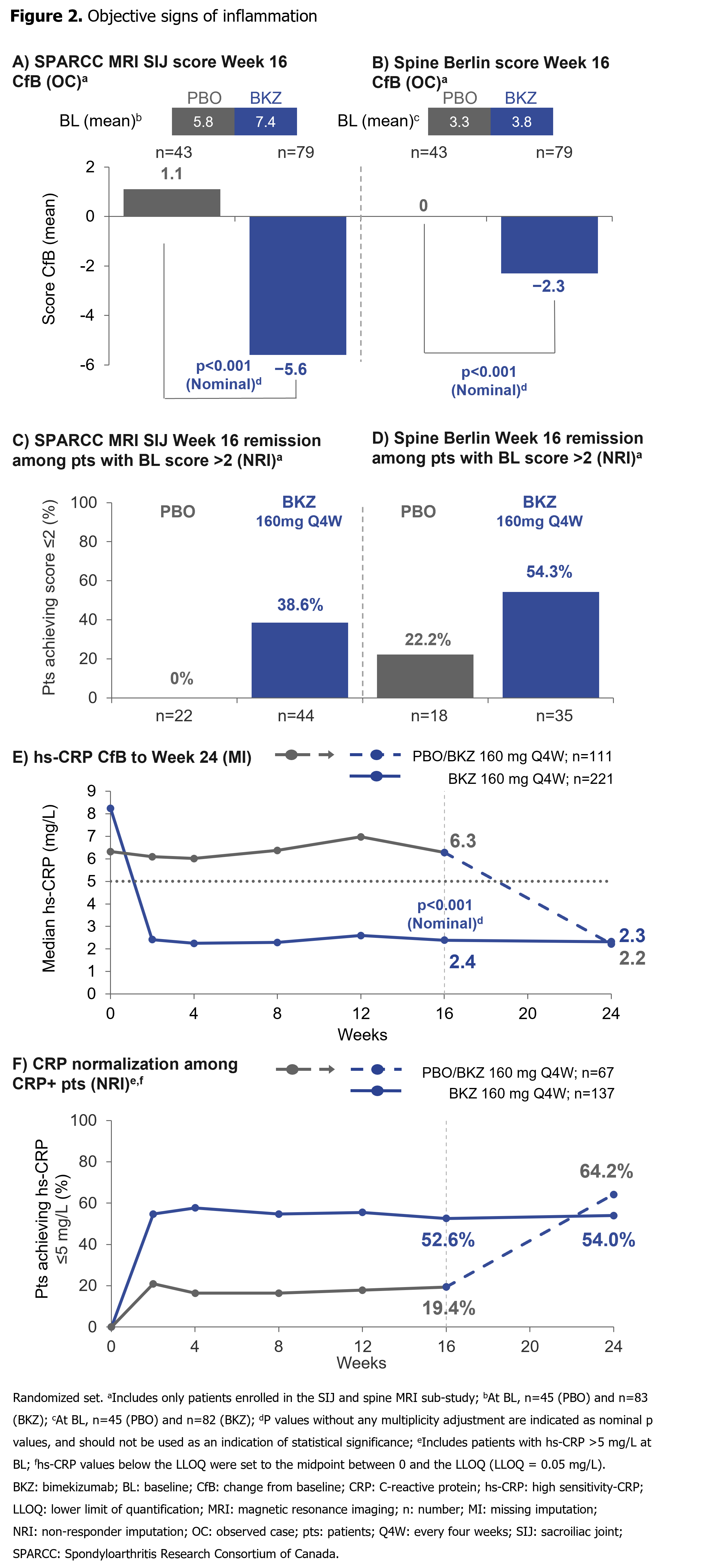
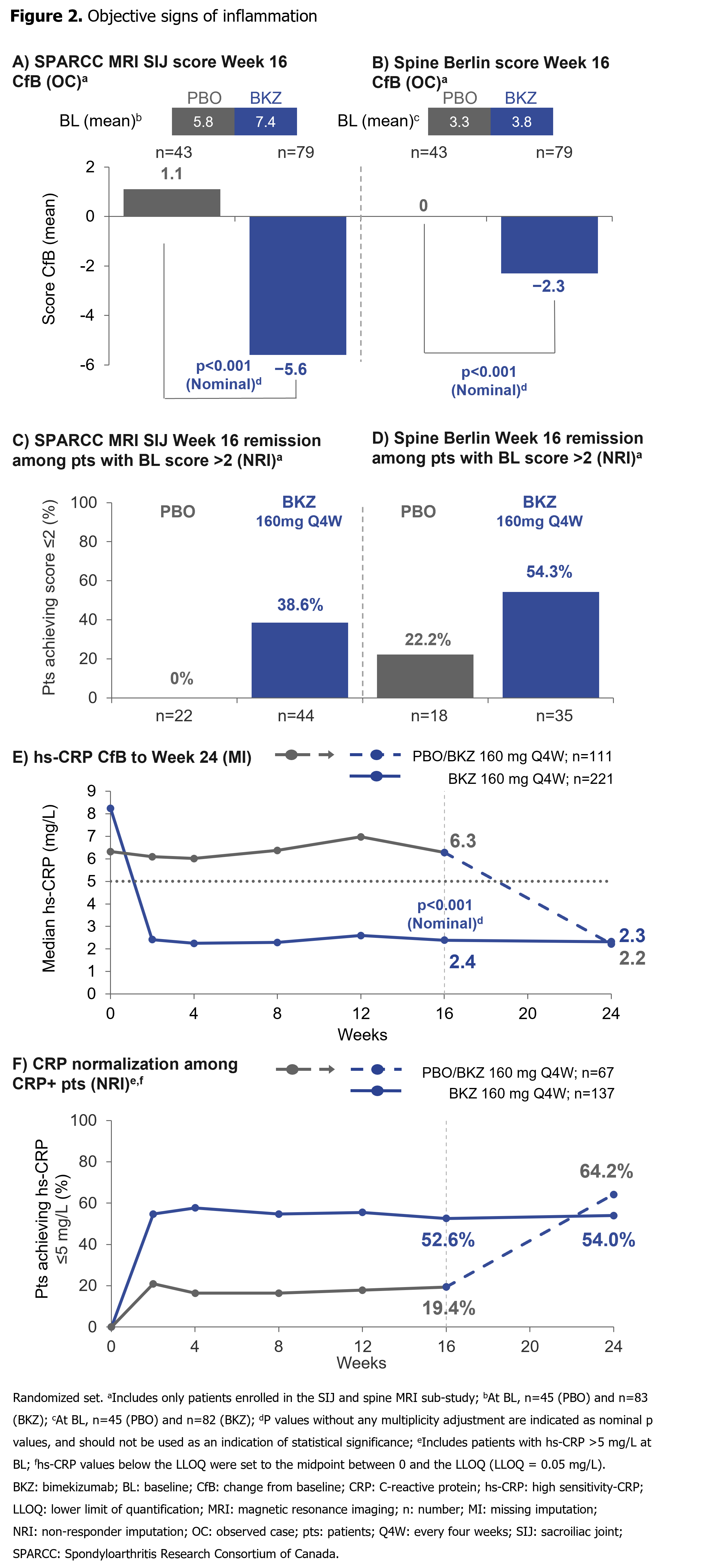
Substantial reductions from BL in SPARCC MRI SIJ inflammation and Berlin MRI Spine scores by Wk 16, and hs-CRP by Wk 2, were achieved with BKZ vs PBO (Figure 2). A higher proportion of pts with SPARCC MRI SIJ and Berlin MRI Spine scores >2 at BL achieved MRI remission (score ≤2) at Wk 16 with BKZ vs PBO. Among CRP+ pts (hs-CRP >5.0 mg/L), a greater proportion of pts treated with BKZ vs PBO achieved normalization (hs-CRP ≤5.0 mg/L) of CRP through Wk 16. For pts who switched from PBO to BKZ at Wk 16, Wk 24 normalization rates approached those seen in BKZ-randomized pts (Figure 2).
At Wk 24, 183/330 (55.5%) pts had ≥1 TEAE on BKZ; most frequent were nasopharyngitis (6.4%), diarrhea (3.9%), headache (3.6%) and oral candidiasis (3.0%). All fungal infections were non-severe and non-systemic; 2 (0.6%) led to treatment discontinuation. Up to Wk 24, incidence of serious TEAEs was low (3.6%); no active tuberculosis, MACE or deaths were reported; incidence of adjudicated IBD (0.3%) and uveitis (0.6%) were low.
Conclusion: Dual inhibition of IL-17A and IL-17F with BKZ in pts with active AS resulted in rapid, clinically relevant improvements in efficacy outcomes vs PBO, including suppression of inflammation. No new safety signals were observed.1,2
References: 1. van der Heijde D. Ann Rheum Dis 2020;79:595–604; 2. Gensler L. Arthritis Rheumatol 2021;73(suppl 10):0491.
.jpeg)
Disclosures: D. van der Heijde, AbbVie, Bayer, BMS, Cyxone, Eisai, Galapagos, Gilead, Glaxo-Smith-Kline, Janssen, Novartis, Pfizer, UCB, Imaging Rheumatology bv, Lilly; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi; M. Dougados, Novartis, AbbVie, Eli Lilly, Merck, Pfizer, UCB Pharma; M. Brown, UCB Pharma, Pfizer, Clementia, Ipsen, Incyte, Regeneron, Grey Wolf Therapeutics, Xinthera, Novartis; D. Poddubnyy, AbbVie, Biocad, Bristol-Myers Squibb, Eli Lilly, Gilead, GlaxoSmithKline, MSD, Moonlake, Novartis, Pfizer, Samsung-Bioepis, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; N. Haroon, AbbVie/Abbott, Janssen, Eli Lilly, Novartis, UCB; H. Xu, None; T. Tomita, Graduate School of Health Sciences, Morinomiya University of Medical Sciences, Osaka, Japan, AbbVie, Eli Lilly, Gilead, Novartis, Pfizer, Astellas, Bristol-Myers Squibb (BMS), Eisai, Janssen, Kyowa Kirin, Mitsubishi-Tanabe, Department of Orthopaedic Biomaterial Science, Osaka University Graduate School of Medicine, Osaka, Japan; L. Gensler, Novartis, Pfizer Inc, UCB Pharma, AbbVie, Eli Lilly, Janssen, Gilead, Moonlake; M. Oortgiesen, UCB Pharma; C. Fleurinck, UCB Pharma; N. de Peyrecave, UCB Pharma, GlaxoSmithKlein (GSK); T. Vaux, UCB Pharma; A. Marten, UCB Pharma; A. Deodhar, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Pfizer Inc, UCB Pharma, Aurinia, Moonlake.
Background/Purpose: Bimekizumab (BKZ) is a monoclonal IgG1 antibody that selectively inhibits IL-17F in addition to IL-17A. In a phase 2b study, BKZ showed rapid and sustained efficacy and was well tolerated up to 156 weeks (wks) in patients (pts) with active ankylosing spondylitis (AS).1,2 Here, we assess efficacy and safety of BKZ vs placebo (PBO) in pts with active AS up to Wk 24 in the ongoing pivotal phase 3 study, BE MOBILE 2.
Methods: BE MOBILE 2 (NCT03928743) comprises a 16-wk double blind, PBO-controlled period and 36-wk maintenance period. Pts were aged ≥18 years (yrs), met modified New York Criteria and had active AS (BASDAI ≥4, spinal pain ≥4) at baseline (BL). Pts were randomized 2:1, BKZ 160 mg Q4W:PBO. From Wk 16, all pts received BKZ 160 mg Q4W. Primary and secondary efficacy endpoints were assessed at Wk 16, and up to Wk 24. Treatment-emergent adverse events (TEAEs; MedDRA v19.0) are reported among patients who received ≥1 BKZ dose by preferred term up to Wk 24.
Results: Of 332 randomized pts (BKZ: 221; PBO: 111), 322 (97.0%) completed Wk 16 and 313 (94.3%) Wk 24. BL characteristics were comparable between groups: mean age 40.4 yrs, symptom duration 13.5 yrs; 27.7% pts female, 85.5% HLA-B27+, 16.3% TNFi-inadequate responders (IR).
At Wk 16, the primary (ASAS40: 44.8% BKZ vs 22.5% PBO; p< 0.001) and all ranked secondary endpoints were met (Table). ASAS40 responses at Wk 16 were consistent across both TNFi-naïve (45.7% BKZ vs 23.4% PBO) and TNFi-IR (40.5% BKZ vs 17.6% PBO) populations. Responses with BKZ were rapid, including in PBO pts who switched to BKZ at Wk 16, and increased to Wk 24 (Table; Figure 1). At Wk 24, nearly 50% BKZ-randomized pts had achieved ASDAS < 2.1 (Figure 1).
Substantial reductions from BL in SPARCC MRI SIJ inflammation and Berlin MRI Spine scores by Wk 16, and hs-CRP by Wk 2, were achieved with BKZ vs PBO (Figure 2). A higher proportion of pts with SPARCC MRI SIJ and Berlin MRI Spine scores >2 at BL achieved MRI remission (score ≤2) at Wk 16 with BKZ vs PBO. Among CRP+ pts (hs-CRP >5.0 mg/L), a greater proportion of pts treated with BKZ vs PBO achieved normalization (hs-CRP ≤5.0 mg/L) of CRP through Wk 16. For pts who switched from PBO to BKZ at Wk 16, Wk 24 normalization rates approached those seen in BKZ-randomized pts (Figure 2).
At Wk 24, 183/330 (55.5%) pts had ≥1 TEAE on BKZ; most frequent were nasopharyngitis (6.4%), diarrhea (3.9%), headache (3.6%) and oral candidiasis (3.0%). All fungal infections were non-severe and non-systemic; 2 (0.6%) led to treatment discontinuation. Up to Wk 24, incidence of serious TEAEs was low (3.6%); no active tuberculosis, MACE or deaths were reported; incidence of adjudicated IBD (0.3%) and uveitis (0.6%) were low.
Conclusion: Dual inhibition of IL-17A and IL-17F with BKZ in pts with active AS resulted in rapid, clinically relevant improvements in efficacy outcomes vs PBO, including suppression of inflammation. No new safety signals were observed.1,2
References: 1. van der Heijde D. Ann Rheum Dis 2020;79:595–604; 2. Gensler L. Arthritis Rheumatol 2021;73(suppl 10):0491.
.jpeg)
Disclosures: D. van der Heijde, AbbVie, Bayer, BMS, Cyxone, Eisai, Galapagos, Gilead, Glaxo-Smith-Kline, Janssen, Novartis, Pfizer, UCB, Imaging Rheumatology bv, Lilly; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi; M. Dougados, Novartis, AbbVie, Eli Lilly, Merck, Pfizer, UCB Pharma; M. Brown, UCB Pharma, Pfizer, Clementia, Ipsen, Incyte, Regeneron, Grey Wolf Therapeutics, Xinthera, Novartis; D. Poddubnyy, AbbVie, Biocad, Bristol-Myers Squibb, Eli Lilly, Gilead, GlaxoSmithKline, MSD, Moonlake, Novartis, Pfizer, Samsung-Bioepis, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; N. Haroon, AbbVie/Abbott, Janssen, Eli Lilly, Novartis, UCB; H. Xu, None; T. Tomita, Graduate School of Health Sciences, Morinomiya University of Medical Sciences, Osaka, Japan, AbbVie, Eli Lilly, Gilead, Novartis, Pfizer, Astellas, Bristol-Myers Squibb (BMS), Eisai, Janssen, Kyowa Kirin, Mitsubishi-Tanabe, Department of Orthopaedic Biomaterial Science, Osaka University Graduate School of Medicine, Osaka, Japan; L. Gensler, Novartis, Pfizer Inc, UCB Pharma, AbbVie, Eli Lilly, Janssen, Gilead, Moonlake; M. Oortgiesen, UCB Pharma; C. Fleurinck, UCB Pharma; N. de Peyrecave, UCB Pharma, GlaxoSmithKlein (GSK); T. Vaux, UCB Pharma; A. Marten, UCB Pharma; A. Deodhar, AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Pfizer Inc, UCB Pharma, Aurinia, Moonlake.

