Back
Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Endoscopy / Stomach / GI Bleeding
35 - Cap Assisted Endoscopic Treatment of Esophageal Food Bolus and/or Foreign Body Ingestion: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
9:40 AM – 9:50 AM ET
Location: Hall C1
- BM
Babu P. Mohan, MD, MS
University of Utah School of Medicine
Salt Lake City, UT
Presenting Author(s)
Award: Outstanding Research Award in the General Endoscopy Category (Trainee)
Babu P. Mohan, MD, MS1, Jay Bapaye, MD2, Syed Hamaad Rahman, DO3, Priyadarshini Loganathan, MD4, Arunkumar Muthusamy, MD5, Daryl Ramai, MD, MPH1, Suresh Ponnada, MD6, Saurabh Chandan, MD7, John Fang, MD1
1University of Utah School of Medicine, Salt Lake City, UT; 2Rochester General Hospital, Rochester, NY; 3Methodist Dallas Medical Center, Dallas, TX; 4UT Health, San Antonio, TX; 5Cedar Valley Medical Specialists, Waterloo, IA; 6Carilion Roanoke Memorial Center, Roanoke, VA; 7CHI Health Creighton School of Medicine, Omaha, NE
Introduction: Esophageal food bolus and/ or foreign body (FB) impaction is one of the most common gastrointestinal emergencies where early endoscopic intervention is warranted. Early time to intervention with faster procedure time are associated with good patient outcomes. In recent literature, cap assisted endoscopic removal of esophageal FB seems to be associated with favorable outcomes as compared to conventional methods. This meta-analysis reports on the pooled outcomes of cap-assisted endoscopic removal of esophageal FB.
Methods: We conducted a comprehensive search of several databases including Medline, Scopus, Embase, from inception to February 2022, to identify studies reporting on the use of cap in endoscopic treatment of esophageal FB. Standard meta-analysis methods and random effects model was used to calculate the pooled odds-ratio (OR) and mean-difference (MD) with corresponding 95% confidence intervals (CI). I2% statistics was used to assess the heterogeneity.
Results: Six studies were included that evaluated 677 patients treated with cap-assistance and 694 patients treated with conventional methods. Peptic stricture (32%) and eosinophilic esophagitis (20%) were the most common esophageal disorders.
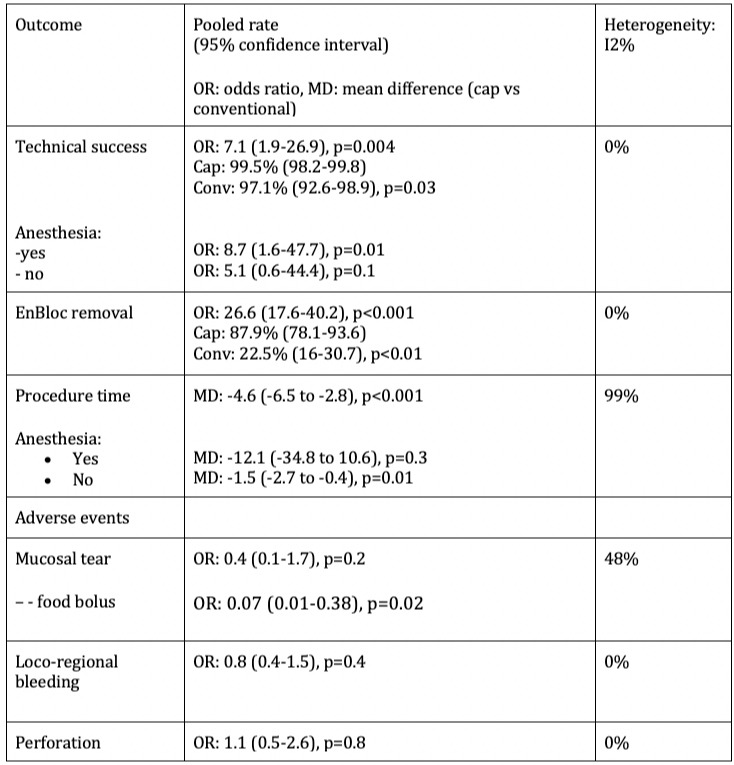
Cap-assisted method demonstrated statistically significant pooled OR for technical success: 7.1 (95% CI [1.9-26.9, p=0.004, I2%=0]), and enbloc removal: 26.6 [17.6-40.2, p< 0.001, I2%=0], with significantly faster procedure time, MD: -4.6min [-6.5to-2.8, p< 0.001, I2%=99]; when compared to conventional method.
Better technical success was achieved with cap-assisted method done under general-anesthesia (OR: 8.7, 1.6-47.7, p=0.01, I2%=0), but faster procedure time was noted with cap-assisted method performed without general-anesthesia (MD: -1.5, -2.7to-0.4, p=0.01, I2%=99). Pooled adverse events were comparable. However, pooled OR of mucosal tear was significantly less with the use of cap in food-bolus impactions (OR: 0.07, 0.01-0.38, p=0.02, I2%=0). No airway related adverse events were reported when general anesthesia was not used.
Discussion: This meta-analysis demonstrates significantly better pooled technical success, enbloc removal and faster procedure time with cap-assisted endoscopic removal of esophageal food-bolus and/ or foreign-body impaction as compared to conventional method. With cap-assistance, faster procedure time seems achievable without the need for general anesthesia. However, additional randomized controlled trials are required to further validate this finding.
Disclosures:
Babu P. Mohan, MD, MS1, Jay Bapaye, MD2, Syed Hamaad Rahman, DO3, Priyadarshini Loganathan, MD4, Arunkumar Muthusamy, MD5, Daryl Ramai, MD, MPH1, Suresh Ponnada, MD6, Saurabh Chandan, MD7, John Fang, MD1, 35, Cap Assisted Endoscopic Treatment of Esophageal Food Bolus and/or Foreign Body Ingestion: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Babu P. Mohan, MD, MS1, Jay Bapaye, MD2, Syed Hamaad Rahman, DO3, Priyadarshini Loganathan, MD4, Arunkumar Muthusamy, MD5, Daryl Ramai, MD, MPH1, Suresh Ponnada, MD6, Saurabh Chandan, MD7, John Fang, MD1
1University of Utah School of Medicine, Salt Lake City, UT; 2Rochester General Hospital, Rochester, NY; 3Methodist Dallas Medical Center, Dallas, TX; 4UT Health, San Antonio, TX; 5Cedar Valley Medical Specialists, Waterloo, IA; 6Carilion Roanoke Memorial Center, Roanoke, VA; 7CHI Health Creighton School of Medicine, Omaha, NE
Introduction: Esophageal food bolus and/ or foreign body (FB) impaction is one of the most common gastrointestinal emergencies where early endoscopic intervention is warranted. Early time to intervention with faster procedure time are associated with good patient outcomes. In recent literature, cap assisted endoscopic removal of esophageal FB seems to be associated with favorable outcomes as compared to conventional methods. This meta-analysis reports on the pooled outcomes of cap-assisted endoscopic removal of esophageal FB.
Methods: We conducted a comprehensive search of several databases including Medline, Scopus, Embase, from inception to February 2022, to identify studies reporting on the use of cap in endoscopic treatment of esophageal FB. Standard meta-analysis methods and random effects model was used to calculate the pooled odds-ratio (OR) and mean-difference (MD) with corresponding 95% confidence intervals (CI). I2% statistics was used to assess the heterogeneity.
Results: Six studies were included that evaluated 677 patients treated with cap-assistance and 694 patients treated with conventional methods. Peptic stricture (32%) and eosinophilic esophagitis (20%) were the most common esophageal disorders.
Cap-assisted method demonstrated statistically significant pooled OR for technical success: 7.1 (95% CI [1.9-26.9, p=0.004, I2%=0]), and enbloc removal: 26.6 [17.6-40.2, p< 0.001, I2%=0], with significantly faster procedure time, MD: -4.6min [-6.5to-2.8, p< 0.001, I2%=99]; when compared to conventional method.
Better technical success was achieved with cap-assisted method done under general-anesthesia (OR: 8.7, 1.6-47.7, p=0.01, I2%=0), but faster procedure time was noted with cap-assisted method performed without general-anesthesia (MD: -1.5, -2.7to-0.4, p=0.01, I2%=99). Pooled adverse events were comparable. However, pooled OR of mucosal tear was significantly less with the use of cap in food-bolus impactions (OR: 0.07, 0.01-0.38, p=0.02, I2%=0). No airway related adverse events were reported when general anesthesia was not used.
Discussion: This meta-analysis demonstrates significantly better pooled technical success, enbloc removal and faster procedure time with cap-assisted endoscopic removal of esophageal food-bolus and/ or foreign-body impaction as compared to conventional method. With cap-assistance, faster procedure time seems achievable without the need for general anesthesia. However, additional randomized controlled trials are required to further validate this finding.
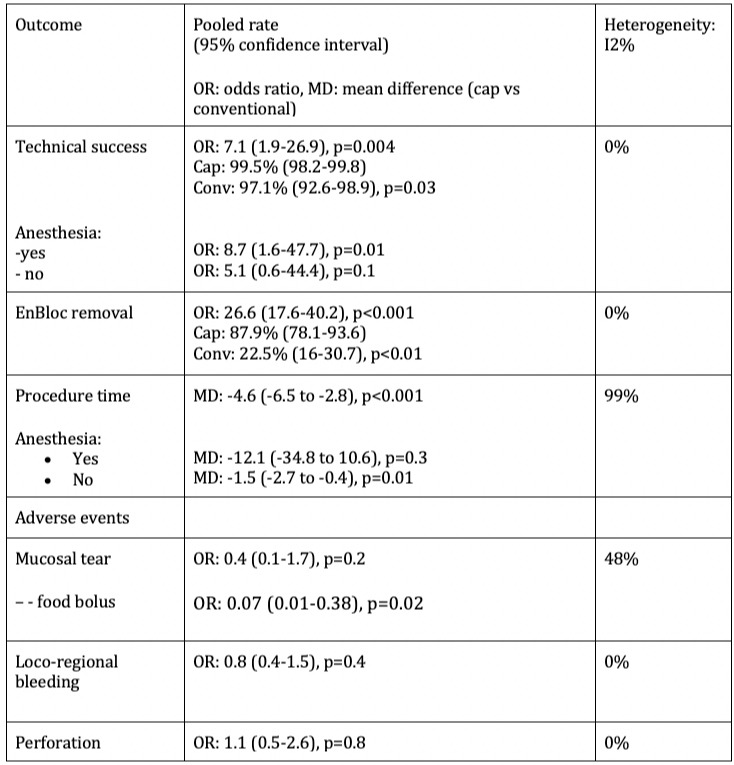
Figure: Summary of pooled results
Disclosures:
Babu Mohan indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Priyadarshini Loganathan indicated no relevant financial relationships.
Arunkumar Muthusamy indicated no relevant financial relationships.
Daryl Ramai indicated no relevant financial relationships.
Suresh Ponnada indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
John Fang indicated no relevant financial relationships.
Babu P. Mohan, MD, MS1, Jay Bapaye, MD2, Syed Hamaad Rahman, DO3, Priyadarshini Loganathan, MD4, Arunkumar Muthusamy, MD5, Daryl Ramai, MD, MPH1, Suresh Ponnada, MD6, Saurabh Chandan, MD7, John Fang, MD1, 35, Cap Assisted Endoscopic Treatment of Esophageal Food Bolus and/or Foreign Body Ingestion: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


